Osteoarthritis of the hip joint (HJ), also called coxarthrosis, according to the World Health Organization, is one of the 15 leading causes of disability in people over 45 years of age. By the age of 65, every 10th citizen suffers from it, and by the age of 85, every 4th citizen of our country suffers from it. This disease often leads to the 3rd degree of disability, in which the patient requires constant care from loved ones or a caregiver, and also loses the ability to move independently. Let's figure out what the symptoms and treatment of osteoarthritis of the hip joint are, whether its prevention is effective and whether the prognosis is positive.
Deforming osteoarthritis of the hip joint
Normally, the heads of the bones are covered with a layer of spongy tissue, which is capable of absorbing moisture in a calm state, and then, under load, releasing it, forming a lubricant. Joint lubrication ensures sliding inside the moving joint, and the cartilage itself additionally acts as a shock absorber. This joint function allows us to walk, run and jump without injury with every movement.
In osteoarthritis of the hip joint, the articular cartilage is primarily affected, the destruction of which causes changes in the synovial articular membrane, degenerative processes in the bone and ligament degeneration. Most often, this pathology occurs in a situation where the mechanical load on the cartilage exceeds its “endurance.” In this case, the lining of the joint seems to wear away, exposing the bones and causing them to rub against each other. Depletion of cartilage tissue leads to a narrowing of the lumen in the joint space, a decrease in the range of motion, and even the appearance of microcracks in the pelvic and femur bones. Therefore, among the complications of the disease, a femoral neck fracture is often encountered - a serious injury that requires long and expensive rehabilitation, and at the age of 60 can even pose a threat to life.
The loss of elasticity of cartilage and lack of gliding in the joint contributes to the formation of osteophytes - spike-shaped bone growths that appear at the site of microcracks. Although osteophytes are designed to compensate for the loss of cartilage tissue and increase the articular surface area, their appearance causes discomfort. They not only make movement difficult and lead to chronic inflammation of the tissues around the joint, but they can also break off with sudden movements, causing severe pain. Nodules can also form in the periarticular tissue.
The deformity can occur on one side, leading to noticeable shortening of the limb and lameness, or on both sides at the same time. The first condition is more typical for post-traumatic disorders, and the second for complex, for example, metabolic diseases that provoke degeneration of cartilage tissue.
Sometimes the disease even affects young people, especially men. In adulthood, it is 2 times more common in women whose bones rapidly lose calcium during menopause.
Diagnostic measures
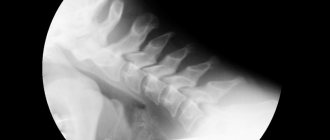
Confirmation of the diagnosis of coxarthrosis is carried out during a physical examination of the patient by a rheumatologist. Additional studies are prescribed to evaluate degenerative changes in joint tissue. Radiography allows you to determine the degree of coxarthrosis and the probable cause of the development of the pathology. Computed tomography and magnetic resonance imaging provide doctors with visual data about the pathological processes inside the joint. Images obtained during MRI record changes in bone structures. CT scan demonstrates the extent of soft tissue damage. This information allows doctors to determine the patient’s treatment strategy and exclude from the medical history other diseases that provoke limited mobility of the hip joint.
Causes of osteoarthritis of the hip joint
Healthy cartilage has the ability to regenerate, but daily stereotypic loads lead to constant wear and tear of certain areas of the articular surface. This leads to joint deformation, increased load on the ligaments and other pathological consequences. The causes of this condition can be divided into two categories: insufficient regeneration (for example, due to insufficient nutrition or excessive abrasion) and breakdown of cartilage tissue (aging, inflammatory processes). In most cases, both of these processes go hand in hand.
Among the common causes of osteoarthritis of the hip joint, one cannot fail to mention:
- congenital abnormalities of the structure of the joint or cartilage tissue (flat feet, excessive joint mobility, intrauterine hip dislocation);
- advanced age;
- menopause in women and endocrine disorders;
- overweight;
- professional or sports loads;
- hip injuries and other pathologies associated with subchondral bone defects;
- pre-existing arthritis and other inflammatory diseases;
- genetic predisposition, including to joint dysplasia;
- metabolic disorders (for example, diabetes mellitus);
- sedentary lifestyle and insufficient muscle mass;
- belonging to the Asian race;
- diet poor in vitamins C, D and K.
Features of the development of the disease
Treatment is selected by the doctor depending on the degree of neglect and symptoms of the lesion and has a degenerative course. The disease is characterized by the proliferation of bone tissue at the edges of the diseased joint (osteophytes). The joints themselves have significant deforming deviations.
This is what the head of a joint looks like, affected by grade 3 osteoarthritis.
Comparison of the surfaces of two joints: on the left - healthy, on the right - affected by the disease.
People over 45 years of age are most susceptible to grade 1 and 2 osteoarthritis. At increased risk are athletes, as well as those men whose musculoskeletal system regularly experiences excessive physical stress.
Treatment of osteoarthritis cannot ensure a complete recovery of a person, especially if the disease is in the second or third form of neglect.
Timely initiation of therapy significantly reduces the risk of developing dangerous complications, relieves the patient of a number of unpleasant symptoms of the disease, and stops the destruction process. The sooner the examination is carried out and therapy is selected, the higher the chance of complete restoration of mobility.
Symptoms of osteoarthritis of the hip joint
The first symptom that patients usually pay attention to is gradually increasing pain at the junction of the pelvis and thigh. Increased pain is observed during physical activity, especially overly active or static exercise, in damp weather. Patients often complain that they need to “disperse” - there is stiffness in the morning or after a working day in one position. Long, not too intense walking or gymnastics usually alleviates the condition.
Often the pain is of a reflected nature, as if “bouncing” from the joint to the groin, buttock and even knee. The appearance of pain at night or its continuity, acute pain when trying to make the slightest movement - all this indicates coxarthrosis in the last stages.
When moving, a crunching and unpleasant clicking sensation often occurs in the hip joint. The length of the step is reduced. Contracture gradually increases - the amplitude of “passive” movements that do not require physical effort narrows. The muscles begin to thin out, spasms and cramps often appear.
The joint begins to swell after a day of work or other, even household, activity. At the same time, the adjacent tissues seem to fill up, harden, and the skin becomes hot. As the joint wears down, a shortening of the limb or both is observed, resulting in a characteristic “wobbly” gait.
Only a doctor - an osteopath, rheumatologist, orthopedist or radiologist - can reliably determine the presence of the disease and its degree. The test is carried out both through hardware research methods and using a checklist of 5 criteria, which includes monitoring the joint during flexion, internal rotation, abduction and adduction of the hip.
It is important to understand that the process takes place secretly for a long time. Even in the absence of complaints and the patient’s completely stable condition, an increase in osteophytes may occur. It is completely impossible to cure hip osteoarthritis, and remission, even long-term, does not mean that the disease does not progress. Therefore, it is extremely important to undergo preventive examinations and regular examinations.
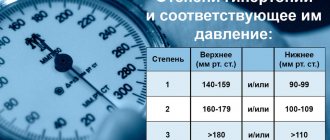
Depending on the symptoms and hidden pathological changes, three stages of coxarthrosis are distinguished:
- Osteoarthritis of the hip joint, grade 1.
In the initial stage, the disease is difficult to diagnose. The pain is mild and is more of a mild but noticeable discomfort, which patients ignore or attribute to fatigue. Sometimes there is dry clicking in the joint, pain when running, carrying heavy objects, or climbing stairs. It becomes difficult or painful to swing the leg during gymnastics. At rest, the pain completely subsides. Pathological changes in the joints are minor and mostly reversible.
- Osteoarthritis of the hip joint, grade 2.
The pain is observed even when walking, and actively “spreads” from the hip joint, occupying the area between the groin and knee joint. Feeling the affected area and standing in line can be painful. X-ray examination shows a narrowing of the joint space by almost half, and active formation of osteophytes. Patients complain of limited movement and joint stiffness.
- Osteoarthritis of the hip joint, grade 3.
The articular gap is practically indistinguishable in the image. The affected joint is significantly deformed in comparison with the healthy one, and the limb is shortened. The pain is constant. There is thinning of the limb or both, associated with muscle atrophy. Due to the pathological tilt of the pelvis, posture changes; patients seem to “fall” forward onto the cane. The load on the back increases, which often leads to problems with the spine.
Diagnostics
A traumatologist-orthopedist or rheumatologist can make the correct diagnosis. At the first appointment, the patient is examined, the degree of joint mobility, the severity of the pain syndrome are determined, and they are asked about the time and nature of the initial manifestations of the disease.
After this, a set of examinations is prescribed:
- X-ray of the hip joint. The gold standard in the diagnosis of hip joint pathologies. The picture clearly shows the condition of the joint space and the presence of osteophytes.
- Ultrasound of the joint. The procedure is prescribed to assess the volume and nature of synovial fluid.
- General blood test. The data shows the patient's health status.
- Biochemical blood test. Patients with suspected arthrosis of the hip joint are tested for markers of rheumatological diseases.
- General urine analysis. Important indicators are the level of protein, bilirubin, glucose, as well as the density and transparency of the material.
- CT or MRI. The pictures show in detail the condition of bone tissue, joints, and adjacent structures.
- Osteoscintigraphy. The patient is administered an osteotropic pharmaceutical drug that acts as a contrast agent. The study determines the intensity of metabolic processes (osteoporosis) in the diseased area and evaluates the state of blood flow.
Treatment of osteoarthritis of the hip joint
How to treat osteoarthritis of the hip joint? Coxarthrosis cannot be overcome without changing your lifestyle - increasing physical activity, giving up bad habits, changing your diet and, in some cases, your place of work. The therapeutic approach requires a combination of drug and non-drug methods, incl. teaching patients about primary prevention. A course of anti-inflammatory drugs is prescribed to induce remission, supportive treatment with chondroprotectors, a strict or non-strict diet, hirudotherapy and hardware physiotherapy, and mud therapy. Occasionally, manual therapy is used to improve mobility in the joint and alleviate the psychological state of patients (when there is a fear of movement, so-called kinesiophobia). The patient is required to go on sick leave during an exacerbation of the disease, and to do daily therapeutic exercises during the period of remission. At the third stage, as a rule, surgical intervention is indicated - joint replacement with titanium and other medical alloys, surgical reconstruction, arthroscopic sanitation and others as indicated.
Treatment is carried out in several directions: pain relief, treatment of concomitant diseases, ensuring independent movement, normalizing metabolism, stimulating blood circulation and lymphatic drainage, preventing pathologies arising from coxarthrosis, as well as eliminating conditions for the progression of the disease. The main goal of therapy is to maintain the patient's physical activity, positive emotional state and ability to work as much as possible.
Drug treatment is also divided into two areas: emergency care for the patient (analgesics, NSAIDs and glucocorticosteroids in the form of tablets and injections) and long-term therapy aimed at strengthening and regenerating cartilage (chondroitin, glucosamine, hyaluronic acid, vitamin-mineral complexes, rehydration drugs in courses up to 6 months a year), improving blood microcirculation. Injection replacement of synovial fluid is allowed, which combines immediate relief with long-term protection of cartilage.
The leading role is given to physiotherapy - acupuncture, magnetic therapy, electrophoresis, ultrasonophoresis, electromyostimulation, laser, UV and heat treatment. Positive effects are also demonstrated by ergotherapy, massage, and swimming.
Diet for osteoarthritis of the hip joint
Since cartilage tissue is devoid of blood vessels, its nutrition occurs through the synovial membrane, from which it very slowly absorbs the necessary substances. Therefore, to prevent osteoarthritis of the hip joint, it is so necessary to have a balanced diet rich in proteins, vitamins and minerals, as well as a period of rest sufficient for the restoration of cartilage.
The main emphasis should be on dishes that contain gelling elements (fruit jellies, aspic, jellied meat, recipes from pig ears, legs, tails and skin, as well as whole sea fish). Also useful are eggs, legumes, all types of boiled, stewed or baked meat, fermented milk products, sources of polyunsaturated fatty acids and plant collagen. It is extremely important to drink at least 2.5 liters of purified or mineral water to maintain the elasticity of cartilage.
Folk remedies
After the main treatment, orthopedists allow the use of folk remedies. They are used to eliminate mild pain and morning stiffness.
Burdock root
Large young burdock root is peeled and crushed. A tablespoon of plant material is placed in a ceramic teapot and poured with a glass of boiling water. After an hour, filter, take 70 ml (about a third of a glass) 3 times a day after meals.
Purslane grass
A tablespoon of fresh purslane herb (stems and leaves) is poured into a glass of hot water and simmered for 10 minutes. Infuse, wrapped, for 2 hours, filter, take 1-2 tablespoons 3-4 times a day after meals.
Herbal collection
Pour a teaspoon of dried calendula and chamomile flowers into a thermos, add a tablespoon of birch buds. Pour in a liter of boiling water and leave for 3 hours. Cool, filter, take 100 ml before bed.