Osteoarthrosis (deforming arthrosis) is a chronic degenerative disease of the joints. This disease is characterized by damage to articular cartilage and tissues surrounding the joints. As a rule, the inflammatory process in the joints is not pronounced. The main mechanism for the development of the disease is considered to be a disorder in the cartilage tissue (excessive wear) due to various reasons.
This can be either natural aging of the body, or the development of similar changes in joints at a younger age (premature aging) due to malnutrition of cartilage tissue, which leads to faster wear of cartilage tissue. With the development of osteoarthritis, salts accumulate in the tissues surrounding the joint, joint deformation and inflammation of the joint capsule (synovitis). About 10-12% of the population suffers from osteoarthritis, most often these are women over 40-45 years old, and in the older age group (over 60-65 years old) almost 100% suffer from osteoarthritis.
Most often, large joints are affected, such as the hip joint, knee, ankle joint, and somewhat less frequently, the shoulder and elbow joints. Small joints can also be involved in the process (joints of the hands). Osteoarthritis (OA), as a rule, is often combined with other degenerative diseases of the musculoskeletal system such as osteochondrosis and spondylosis deformans. The etiology of osteoarthritis is not fully understood, but factors that contribute to the development of osteoarthritis can be divided into hereditary and acquired.
There are also primary and secondary deforming osteoarthritis. The causes of primary osteoarthritis include:
Excessive or repeated loads that significantly exceed the physical capabilities of the cartilage tissue of the joints. This can be either sports or associated with heavy physical work.
Congenital abnormalities of the geometric shape of the joints, which leads to disruption of the biomechanics of the joint and a change in the correct distribution of load vectors on the articular cartilage. These may be congenital dysplasia of the joints, deforming diseases of the spine, abnormalities of skeletal development, underdevelopment and hypermobility of ligaments.
Changes in the structure of cartilage tissue of joints due to microtraumatization, microcirculation disorders, joint injuries (intra-articular fractures, dislocations, subluxations, hemarthrosis).
The following conditions are most often considered to be the causes of secondary osteoarthritis:
Inflammatory processes caused by infection or injury, congenital dysplasia of the hip and knee joints, developmental disorders of the joint, instability of the joint (including after injury), endocrine diseases (for example, diabetes mellitus), metabolic changes (gout, hemachromatosis), necrotic changes in bone tissue , intoxication with heavy metal salts, rheumatological diseases such as rheumatoid arthritis, SLE, blood diseases (hemophilia). There are three stages in the development of osteoarthritis:
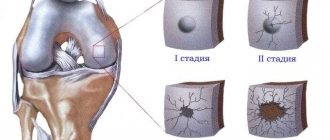
- Stage 1 is characterized by the presence of minor morphological changes in the joint and is manifested by pain during physical activity (radiologically there will only be a narrowing of the joint space). Morphological changes in articular cartilage at stage 1 are manifested by the appearance of roughness and disintegration of the tissue structure.
- Stage 2 is characterized by constant pain in the joints; radiographically, the narrowing of the joint gap is more pronounced; osteophytes appear; morphologically, this stage is characterized by the appearance of tuberosity on the surface of the cartilage and the development of osteophytes.
- Stage 3 osteoarthritis is characterized not only by pain, but also by the appearance of joint dysfunction. Morphologically, stage 3 is manifested by thinning of the cartilage until it disappears, thickening of the intra-articular ligaments, and a sharp decrease in intra-articular fluid.
What is arthrosis
Arthrosis is a disease of the joints of a degenerative-dystrophic nature with the gradual destruction of cartilage and proliferation of bone tissue. The process is accompanied by deformation, impaired joint function and pain. Recently, the term osteoarthritis (OA osteoarthritis) is more often used - a group of diseases that are based not on purely dystrophic, but on dystrophic-inflammatory processes leading to gradual destruction of the joint. More and more experts believe that the causes of arthrosis and osteoarthrosis, the mechanisms of their development are the same, that is, in fact, they are the same disease.
According to statistics, from 10 to 20% of the population suffers from arthrosis in different countries. By the age of 80, almost everyone has age-related disorders in the musculoskeletal system. At the same time, patients do not always consult a doctor on time and take a long time to treat themselves, which leads to disability. Whereas the right treatment can relieve suffering and stop the progression of the disease. Arthrosis codes according to ICD 10: M15-M19.
Consequences and complications
Without timely treatment, osteoarthritis can cause disability, especially with bilateral damage.
It causes:
- severe joint deformation;
- bone curvature;
- loss of mobility;
- shortening of the limb (with coxarthrosis and gonarthrosis).
When the large joints of the legs are affected, a person’s gait and posture change so much that this inevitably leads to problems with the spine, pain in the neck and lower back.
Causes and mechanism of development of arthrosis
The reasons for the development of the articular degenerative-dystrophic process are diverse. Arthrosis is a disease that begins gradually against the background of congenital structural features of connective tissue, as well as prolonged microtrauma, acute joint injuries and diseases. Almost all chronic inflammatory processes (arthritis) eventually turn into degenerative-dystrophic ones with periodic relapses of inflammation. Finally, the largest group of arthrosis is age-related.
Factors predisposing to the development and progression of this pathological process are:
- sedentary lifestyle;
- heavy professional or sports physical activity;
- professions that involve standing for long periods of time without moving;
- excess weight;
- endocrine diseases and hormonal disorders leading to circulatory and metabolic disorders: diabetes mellitus, atherosclerosis, thyroid disease, obesity;
- venous insufficiency;
- poor irregular diet, bad habits (smoking, alcohol abuse) - increase metabolic disorders;
- hereditary predisposition to diseases of the musculoskeletal system.
Under the influence of all these reasons, the cartilage cells covering the articular surfaces of the bones begin to gradually deteriorate. The cartilage first thins, loses its elasticity, and then cracks. The subchondral bone tissue begins to rub against the same dilapidated bone surface on the other side of the joint and collapse. The reaction of bone tissue to this process is its growth, especially at the edges of the joint, which leads to limited mobility and joint deformation.
Joint deformity due to arthrosis
A feature of articular tissue cells is the ability to respond to any, even minor, injuries. Destroyed cells produce pro-inflammatory (causing and supporting the inflammatory process) cytokines. Therefore, the destruction of cartilage and bones is accompanied by an aseptic inflammatory process in the synovium (synovitis) and the effusion of inflammatory fluid into the joint cavity. Periodically developing inflammation contributes to even more active death of hard tissue cells and progression of the disease.
The process is long, at first it does not manifest itself in any way, since the cartilage tissue does not contain nerve endings, so patients do not experience pain in the early stages. They appear when the periosteum located under the cartilage is injured and during exacerbation of inflammatory processes (the periosteum and synovial membrane are very well innervated).
Arthrosis that develops against the background of chronic inflammatory processes is more severe. Complete destruction of articular tissues occurs with the formation of ankylosis (immobility) and disability. Age-related disorders are not so aggressive and rarely lead to severe disorders.
At risk are women over 50 years of age, men over 40 years of age, persons suffering from endocrine pathology and chronic arthritis, as well as persons engaged in heavy physical labor, professions involving prolonged standing, athletes (weightlifters and those involved in traumatic sports) . For these individuals, prevention of arthrosis is of particular importance.
Causes of the disease
A number of reasons can contribute to the appearance of the disease:
- injury or overstrain of joints due to increased physical activity;
- decrease in the amount of estrogen in women during menopause;
- elderly age;
- joint surgery;
- excess body weight;
- hereditary predisposition;
- disruption of the activity of endocrine organs;
- osteoporosis, etc.
Symptoms of arthrosis
Signs of arthrosis do not appear immediately, but several years after the onset of the degenerative-dystrophic process or when inflammation occurs.
First signs
It begins imperceptibly with pain in the limbs during physical activity. In the morning, after a long stay at rest, so-called “starting pains” appear in the joints, combined with mild stiffness. All this goes away after the start of active movements. The pain is aching, dull, not too intense. All this leads to the fact that patients in the early stages rarely go to the doctor, preferring to be treated with folk remedies. Then at this stage it is easiest to stop the progression of the disease.
Obvious symptoms
The pain intensifies, becomes constant, keeps you awake at night, and increases with weather changes. Often the entire limb hurts. Elderly people report aching bones, aching pain in muscles and joints. Arthrosis of the joints of the lower extremities – the knee and hip – develops especially often. The patient quickly gets tired when walking, joints with arthrosis have difficulty bending, and stiffness develops.
Patients complain of limb instability and the appearance of an unsteady gait. When bending, a rough crunch appears in the knees due to the fact that the articular surfaces, devoid of cartilage, rub against each other. It differs from a slight crunching sound during inflammation - synovitis. The knee is deformed due to marginal growth of bone tissue. As patients try to move less, muscle atrophy (decrease in volume) develops, causing the gait to become even more unstable.
In the upper limb, arthrosis often develops after injuries or against the background of chronic arthritis. The deformation is clearly visible in the interphalangeal joints of the hand. Bone growths form on the fingers - Heberden's and Bouchard's nodes, and the hand itself takes on a square shape.
Heberden's and Bouchard's nodes on the interphalangeal joints with arthrosis
Dangerous signs of arthrosis
Since degenerative-dystrophic processes develop slowly, even dangerous symptoms of arthrosis are not always noticed on time.
Dangerous symptoms include:
- the appearance of swelling and pain in a constantly aching limb is a sign of inflammation that requires treatment;
- development of joint deformation;
- pain in the muscles and bones of the limb;
- unsteady gait, impaired mobility when flexing and extending the limb;
- constant pain that spreads to the entire limb.
Why is arthrosis dangerous?
Arthrosis is a disease that develops slowly and rarely causes severe disability. Periodically developing inflammatory processes pose a danger.
Therefore, in recent years, they have begun to distinguish a disease such as osteoarthritis or osteoarthritis (OA), depending on which process predominates in the joint - degenerative-dystrophic or inflammatory. It is OA that causes severe impairment of limb function.
Stages of arthrosis
Clinical and radiological stages of arthrosis according to the Kellgren-Lawrence classification:
- Zero. The patient feels discomfort, sometimes pain when walking. There are no changes on the x-ray.
- Initial (doubtful). The patient is bothered by moderate dull pain when walking for a long time, sometimes a slight crunch when bending a limb. X-ray: slight narrowing of the joint space, small areas of marginal bone defects.
- Easy. The pain intensifies, appears in the morning along with short-term stiffness, and intensifies with movement. X-rays of grade 2 show: a clear narrowing of the joint space and isolated bone growths (osteophytes) along the edges of the articular surfaces.
- Moderate (degenerative). Night pain syndrome appears. Bones and muscles hurt. Sometimes the joint swells slightly and the pain intensifies (a sign of inflammation). On X-ray: even greater narrowing of the joint space and proliferation of osteophytes; bone density increases (osteosclerosis).
- Heavy (deforming). The pain is constant, aching, intensifies with movement, a rough crunching sound when bending the limb, muscle atrophy and deformation. On the x-ray: the joint space is sharply narrowed, the edges of the articular surface have grown significantly, which has led to a change in the structure and deformation of the joint. Read more about deforming arthrosis in this article.
Stages of arthrosis
Possible complications
Arthrosis is a disease complicated by:
- chronic pain syndrome that increases from physical activity;
- joint deformity;
- dysfunction of the limb - stiffness, alternating with complete or partial immobility;
- loss of ability to work and disability.
Exacerbations of arthrosis
Degenerative diseases are characterized by a slow progressive course. Increased pain occurs in damp, cold and windy weather, as well as when inflammation occurs. Inflammatory processes occur with slight swelling and moderate pain. As a rule, the inflammatory process is aseptic in nature, but in the presence of foci of infection and chronic diseases, infection is possible. Therefore, if symptoms of inflammation appear during arthrosis, it is better to consult a doctor. You can do the following yourself:
- take any painkiller - Analgin, Nise, Paracetamol;
- apply anesthetic ointment or gel to the skin over the affected joint - Voltaren, Bystrumgel, Pentalgin, etc.;
- provide rest to the sore limb.
What is the prognosis for osteoarthritis of the joints?
It is literally impossible to make unambiguous predictions in the situation under consideration.
The chances of recovery and the success of the upcoming treatment are largely determined by the timeliness of seeking professional help.
It can be noted that, considering the issue of predicting the situation from the point of eliminating morphological changes, the conclusions are not comforting, which is due to the impossibility of complete restoration of the affected tissues.
The presence of pathology in old age indicates the complexity of the course of the disease, relative to the clinical picture of younger patients.
To summarize, we can come to the conclusion that, regardless of the situation, the most positive prognosis (elimination of complaints and full/partial restoration of motor function) is possible only if you contact your doctor in a timely manner, as well as if all recommendations and prescriptions are followed.
Localizations and clinical forms
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Arthrosis develops mainly in the most loaded joints – the knee and hip. But after an injury or against the background of arthritis, degradation-dystrophic processes can progress in any joint.
Classification of osteoarthritis
There are several classifications. The most famous are:
- Classification by etiology (reasons for development):
- primary – the causes of development have not been established;
- secondary – develop against the background of injuries and diseases.
- Classification by clinical forms:
- polyosteoarthrosis – multiple joint damage; divided into nodular (Heberden's and Bouchard's nodes) and nodular;
- oligoosteoarthrosis – the number of affected joints is no more than two;
- monoosteoarthrosis – damage to one joint;
- in combination with osteochondrosis or osteoarthritis of the spine.
- Classification by localization:
- interphalangeal;
- hip;
- knee;
- other.
Arthrosis of the lower extremities
Due to the high load, the legs suffer first of all:
- Arthrosis of the hip joint (coxarthrosis) is the most severe. The structural features of the hip joint (deep joint cavity, narrow joint space) contribute to the rapid development of degenerative disorders involving muscles and ligaments. If inflammation occurs, the effect of partial or complete immobility develops. Often develops against the background of congenital dysplasia, dislocations, subluxations of the hip, osteochondropathy (aseptic necrosis of the femoral head - Perthes disease). Symptoms of arthrosis: pain initially appears only towards the end of the day, but gradually increases, worries all day, radiates to the groin and buttock area. To reduce pain during coxarthrosis, the patient holds the leg in a forced position, which makes it seem shorter than the healthy one. The pain syndrome is very strong, so patients often agree to endoprosthetics.
- Arthrosis of the knee joint (gonarthrosis) - the most common. The knee withstands the highest loads and is injured, so gonarthrosis develops most often. Arthrosis of two joints is distinguished:
- patellofemoral - develops after injuries to the patellofemoral joint and is initially characterized by an inconspicuous course, since the joint has a lot of shock absorber cartilage that does not allow injury to the bone for a long time; but pain gradually appears after physical exertion, long walking or standing, when going up or down stairs; Over time, they become constant, dull, aching, and intensify when the weather changes; inflammation of the synovial membrane (synovitis) often develops, causing the pain to become acute;
- tibiofemoral arthrosis (femoral-tibial joint) - develops less frequently and is easier. The pain radiates down to the area of the lower leg and foot; Complete immobility with gonarthrosis rarely occurs. Prevention and timely treatment of arthrosis of the knee joint are very important - this will allow a person to live without pain. But even with an advanced disease, it is quite possible to relieve the patient from pain.
- Ankle – a large load also falls on the ankle, which is why arthrosis often develops in it. He is also often injured and the degenerative process is post-traumatic in nature. It is also affected in reactive arthritis. Symptoms: the disease is asymptomatic for a long time, but then pain appears. First, during physical activity, and then constant, aching pain. Stiffness of movement after a long rest is also characteristic, which goes away within half an hour. Complete immobility of the ankle is rare and only if the underlying cause of the disease is a long-term inflammatory process.
- Heel - arthrosis can develop in the area of the subtalar or talocalcaneal-navicular joints after injuries and diseases. They do not manifest themselves for a long time, then painful sensations in the heel begin to appear, gradually acquiring a constant painful character. Disability is rare.
Arthrosis of the upper extremities
Arthrosis in the joints of the hands develops less frequently. Main features of localizations in individual joints:
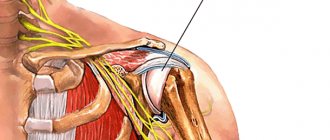
- Arthrosis of the shoulder joint. It usually develops after injuries and against the background of microtrauma in weightlifters, as well as in people engaged in heavy physical work. Acromial (acromio-clavicular) arthrosis is a consequence of trauma and inflammatory processes. At first it goes unnoticed, but then pain appears in the upper part of the shoulder, radiating to the elbow and neck, stiffness of movements and crunching when moving. The pain can be permanent and debilitating. Sometimes accompanied by inflammation, which contributes to the progression of the disease. If left untreated, partial ankylosis develops. Read more about shoulder arthrosis here.
- Elbow arthrosis - occurs rarely, mainly in miners, blacksmiths and workers of some other professions who deal with vibrating tools. Symptoms: pain in the elbow when bending and straightening the arm, stiffness after a long rest. If left untreated, there will be persistent dysfunction.
- Arthrosis of the joints of the hand. Most often, the degenerative process develops in the carpometacarpal joint of the first finger, since it is usually subject to trauma during household work. It manifests itself as a periodically appearing dull soreness in the outer side of the palm, radiating to the thumb.
- Arthrosis of the finger joints. Develops when performing small tasks (knitting, embroidery, sewing). In the distal (uppermost) interphalangeal joints, the pathological process manifests itself in the form of growths of bone tissue - Heberden's nodes; joint pain usually does not occur or they appear only occasionally, for example, when the weather changes. In the proximal interphalangeal joints, the disease manifests itself in the form of the same bone growths on the joints of the fingers located below - Bouchard's nodes.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Arthrosis of the spine (vertebral)
In different parts of the spinal column, arthrosis manifests itself in the form of different symptoms:
- Cervical uncovertebral arthrosis (cervical facet spondyloarthrosis) . Degenerative-dystrophic changes in small facet joints of the cervical vertebrae. Arthrosis of the joints of the cervical spine develops mainly in the second half of life in people who work for a long time in a stationary state with their heads bowed. It can also develop after injuries and against the background of chronic arthritis. It manifests itself in the form of headaches, dizziness, pain in the neck, radiating to the shoulder and crunching when moving. Decreased vision, hearing, and the appearance of high blood pressure (BP) are also possible. Since overgrown bone tissue can compress the vessels supplying the brain, the disease sometimes threatens the patient’s life. Requires long-term rehabilitation treatment.
- Thoracic spondyloarthrosis (arthrosis of the joints of the thoracic spine). It is much less common than the cervical one. First, moderate and then quite severe pain in the spine appears, intensifying with coughing, sneezing and deep breathing. Sometimes the symptoms are similar to manifestations of diseases of the cardiovascular and respiratory systems. To correctly establish the diagnosis, additional examination is required. In the thoracic region there are also costovertebral joints, 2 of them on each rib (rib head and costotransverse). They can also develop degenerative-dystrophic processes, mainly in older women. The disease manifests itself as pain in the chest. If it lasts for a long time, it can cause severe complications from the cardiovascular and respiratory systems.
- Lumbar spondyloarthrosis. It is a consequence of heavy physical labor and spinal injuries. Arthrosis of the joints of the lumbar spine manifests itself in the form of aching pain, aggravated by bending the body. Characterized by stiffness of movement after a long rest, a crunch in the back when bending over.
- Sacrococcygeal spondyloarthrosis. Most often develops after injuries, for example, after a fall and injury to the tailbone. It manifests itself as pain, aggravated by sitting and prolonged walking. Requires long-term rehabilitation treatment.
Tissue changes in spondyloarthrosis
Arthrosis of the temporomandibular joint (TMJ)
The disease develops with chronic arthritis of the TMJ, malocclusion, absence of lateral teeth, and problems with prosthetics. There is a violation of blood circulation and metabolism in the TMJ area with the development of degenerative-dystrophic processes in it. Symptoms of arthrosis of this joint: aching pain in the lower jaw, stiffness and crunching when opening the mouth and chewing. The pain increases with changes in weather, as well as with the development of synovitis. The long course of the disease leads to the appearance of asymmetry: displacement of the jaw tissue to the affected side.
Read more about the disease here.
Pharmacotherapy of OA, recommendations of the International Society for the Study of OA (OARSI), 2014
The following drugs are used to treat osteoarthritis:
Paracetamol
Inflammatory mediators can stimulate angiogenesis. Thus, hypoxia, which often occurs during the inflammatory process, stimulates the synthesis of vascular endothelial growth factor (VEGF). Vascular growth can also be stimulated by fibrinogen and inflammatory cells: macrophages, lymphocytes, mast cells and fibroblasts.
A 2010 meta-analysis confirmed the effectiveness of paracetamol as a moderate pain reliever for OA [8]. However, studies have shown an increased risk of side effects associated with paracetamol use, including gastrointestinal (GI) manifestations and multiorgan disorders [8]. In connection with these data, OARSI recommends using the drug strictly in accordance with the dosage and duration of the course.
Capsaicin
A 2011 comparative, double-blind, randomized study of 100 patients with knee OA found that the topical analgesic capsaicin was 50% more effective as an analgesic for osteoarthritis than placebo [9].
Corticosteroids (intra-articular injections)
Recent studies demonstrate a clinically significant short-term analgesic effect [10]. There are several other recommended medications for the treatment of osteoarthritis.
Chondroitin
Four studies examining the use of chondroitin in OA showed mixed results. Some trials showed some analgesic effects, while others showed chondroitin's effect was no different from placebo [11]. In addition, specialists from the International Society for the Study of OA - OARSI note a high degree of heterogeneity of studies and their low quality, and therefore a final assessment of the effectiveness of chondroitin is extremely difficult. Thus, the effect of chondroitin as a symptomatic remedy is considered questionable, and it is not recommended as a drug for the treatment of OA.
Diacerein
A 2010 meta-analysis examining data from six studies involving 1533 patients found a relatively modest but statistically significant analgesic effect of the non-narcotic analgesic diacerein compared with placebo [12]. The meta-analysis also noted a significant increase in the risk of diarrhea among volunteers taking diacerein. However, diacerein is considered safer than NSAIDs.
Duloxetine
Studies have proven that the inhibitor of neuronal reuptake of serotonin and norepinephrine, the third generation antidepressant duloxetine, is more effective than placebo in relieving pain in OA [13]. However, 16.3% of patients receiving duloxetine experienced side effects (compared to 5.6% in the placebo group). These include nausea, dry mouth, drowsiness, fatigue, decreased appetite, and hyperhidrosis. In this regard, the need for the use of duloxetine for the treatment of OA in persons with concomitant diseases (diabetes mellitus, arterial hypertension and other cardiovascular diseases, renal failure, gastrointestinal bleeding, depression, limitation of physical activity, including due to obesity) is recognized doubtful*.
Glucosamine
A meta-analysis of three randomized controlled trials found a beneficial effect of rosehip powder (5 g/day) as an analgesic for OA compared with placebo, but these data require further study.
Two large studies evaluating the effectiveness of glucosamine in the treatment of OA yielded conflicting results [6]. One study showed a statistically significant analgesic effect, while another showed no effect. The latest meta-analysis, which included a large-scale study, did not prove the effectiveness of glucosamine at all. Based on these data, OARSI experts came to the conclusion that the effectiveness of glucosamine as a symptomatic agent for OA is questionable. It is not recommended as a treatment for OA [6].
Hyaluronic acid (intra-articular injections)
The results of clinical trials (CTs) examining the effectiveness of intra-articular injection of hyaluronic acid (HA) have been controversial [6]. Conflicting data from meta-analyses and individual studies cast doubt on the advisability of using hyaluronic acid preparations for OA of the knee and hip joints. For OA of several joints, GC is not recommended.
Oral NSAIDs
Taking these drugs is included in recommendations for the treatment of osteoarthritis for patients without concomitant diseases. For concomitant gastrointestinal diseases, it is necessary to prescribe proton pump inhibitors along with NSAIDs. For patients at high risk (GI bleeding, myocardial infarction, history of chronic renal failure), oral NSAIDs are strictly not recommended.
Risedronic acid
A review of the literature conducted by Japanese scientists in 2010 suggests that high doses of risedronic acid do not reduce the severity of OA symptoms, but may help reduce the progression of OA by maintaining the structural integrity of the subchondral bone [14]. Laboratoryly, this effect is manifested by a decrease in the level of the cartilage degradation marker CTX-II. Thus, the effectiveness of residronic acid requires further study.
Opioids
Studies have shown moderate effectiveness of codeine and morphine for OA of the knee and hip. A 2006 Cochrane meta-analysis of placebo-controlled trials involving 1019 patients found statistically significant benefits for tramadol compared with placebo [15].
List of sources
- Folomeeva O. M., Erdes Sh. F. Prevalence and social significance of rheumatic diseases in the Russian Federation // Doctor (rheumatology). 2007. No. 10. P. 3–12.
- Poole AR. An introduction to the pathophysiology of osteoarthritis. Front Biosci. 1999 Oct 15. 4: D662–70.
- van Baarsen LG et al. Heterogeneous expression pattern of interleukin 17A (IL-17A), IL-17F and their receptors in synovium of rheumatoid arthritis, psoriatic arthritis and osteoarthritis… Arthritis Res Ther. 2014. 16 (4):426.
- Brandt KD. A pessimistic view of serologic markers for diagnosis and management of osteoarthritis. Biochemical, immunologic and clinicopathologic barriers. J Rheumatol Suppl. 1989 Aug. 18:39–42.
- Recht MP et al. Abnormalities of articular cartilage in the knee: analysis of available MR techniques. Radiology. 1993 May. 187(2):473–8.
- Zhang W et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage. 2007 Sep. 15(9):981–1000.
- Felson DT et al. Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study. Ann Intern Med. 1992 Apr 1. 116 (7):535–9.
- Bannuru RRDU, McAlindon TE. Reassessing the role of acetaminophen in osteoarthritis: systematic review and meta-analysis. Osteoarthritis Research Society International World Congress; 2010 Sep 23–26; Brussels, Belgium. Osteoarthritis Cartilage 2010; 18 (Suppl 2):P 250.
- Kosuwon W et al. Efficacy of symptomatic control of knee osteoarthritis with 0.0125% of capsaicin versus placebo. J Med Assoc Thai¼Chotmaihet Thangphaet 2010; 93(10):118e95. Epub 2010/10/27.
- Bannuru RR et al. Therapeutic trajectory of hyaluronic acid versus corticosteroids in the treatment of knee osteoarthritis: a systematic review and meta-analysis. Arthritis Rheum 2009; 61 (12):1704–11.
- McAlindon TE et al. OARSI guidelines for the non-surgical management of knee osteoarthritis //Osteoarthritis and Cartilage. - 2014. - T. 22. - No. 3. - pp. 363–388.
- Bartels EM et al. Symptomatic efficacy and safety of diacerein in the treatment of osteoarthritis: a meta-analysis of randomized placebo-controlled trials. Osteoarthritis and Cartilage/OARS. Osteoarthritis Research Society 2010; 18(3):289–96.
- Citrome L, Weiss-Citrome A. A systematic review of duloxetine for osteoarthritic pain: what is the number needed to treat, number needed to harm, and likelihood to be helped or harmed? Postgrad Med 2012; 124(1):83.
- Iwamoto J. et al. Effects of risedronate on osteoarthritis of the knee //Yonsei medical journal. 2010. No. 2. 164–170 pp.
- Cepeda MS, Camargo F, Zea C, Valencia L. Tramadol for osteoarthritis. Cochrane Database Syst Rev 2006; (3):CD005 522. Epub 2006/07/21.
Types of secondary arthrosis
The causes of secondary arthrosis are various diseases and injuries. The most common types of arthrosis are:
- Post-traumatic – develops after injuries . A very common cause of the development of articular degenerative-dystrophic changes. The pathological process begins with inflammation and gradually turns into an exchange process with the development of joint deformation, persistent dysfunction and pain.
- Metabolic and endocrine arthrosis:
- gouty - develops slowly against the background of gout. In the first years, attacks of gout do not lead to changes in the joints, but then degenerative = dystrophic changes gradually develop in them, leading to dysfunction;
- against the background of hormonal disorders.
- Arthrosis against the background of congenital and acquired orthopedic pathology:
- congenital hip dislocation;
- thickening of the acetabulum (congenital);
- dysplasia (impaired formation) of the joint;
- osteochondropathy – aseptic necrosis of the femoral head (Perthes disease), etc.
- Arthrosis as an outcome of chronic arthritis:
- reactive – is a consequence of a previous urogenital or intestinal infection; joint tissues react to infection - an inflammatory reaction develops; with proper examination and treatment, complete recovery occurs, but if left untreated, the inflammatory process becomes chronic with exacerbations and remissions; then gradually becomes degenerative with the development of arthrosis;
- rheumatoid – develops against the background of an autoimmune inflammatory process, which over time turns into a degenerative process with joint deformation; Mainly the small joints of the hand and foot are deformed;
- psoriatic – the cause of the lesion is psoriasis; At first it is an inflammatory process, which after a few years turns into arthrosis-arthritis with degenerative processes and deformation.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
Therapy
Treatment of osteoarthritis is aimed at relieving pain and improving the functional state of the joint. Optimally, patients should receive a combination of non-pharmacological techniques and pharmacotherapy [6].
The inflammatory reaction in the joint is catalyzed by cyclooxygenase (COX) and lipoxygenase (LOX), producing mediators of inflammation and pain (prostaglandins, including prostaglandin E2 and leukotrienes). The latter, in addition to direct participation in the pathogenesis of inflammation, reduce the threshold for pain perception in the affected joint, thereby increasing pain sensations
Non-drug ways to control OA:
- weight normalization [7]
- physiotherapy
- physiotherapy
- occupational therapy
- unloading of some joints (for example, knee, hip)
Diagnosis of arthrosis
The diagnosis is made based on a doctor’s examination and is confirmed by laboratory and instrumental studies:
- Laboratory tests - general clinical, biochemical, immunological blood tests. Signs of inflammation, causes of arthrosis (metabolic disorders, autoimmune processes) are revealed. If necessary, intra-articular fluid is taken for examination to identify infection and its sensitivity to antibiotics.
- Instrumental diagnostics:
- Ultrasound, MRI - changes in soft articular and periarticular tissues are detected;
- X-ray, CT – changes in bone tissue; these are the main methods for confirming the presence of arthrosis;
- arthroscopy – according to indications, if there is a suspicion of an inflammatory process.
Treatment of arthrosis
Based on the results of the diagnosis of arthrosis, individually selected complex treatment is prescribed, including drug and non-drug therapy. Equally important is a healthy active lifestyle with the exception of heavy physical activity and proper nutrition.
Drug therapy
To eliminate the symptoms of the disease and suppress its progression, the following medications are prescribed:
- To relieve pain, pain therapy is carried out:
- painkillers from the group of non-steroidal anti-inflammatory drugs (NSAIDs); depending on the severity of the pain syndrome, the complex treatment includes medications such as Ibuprofen, Diclofenac, Ketorol, etc.; they are prescribed in the form of tablets for oral administration, injections or ointments (gels);
- muscle relaxants - medications that relieve spasm from the periarticular muscles (spasm increases pain and impairs blood circulation) - Mydocalm;
- neurotropic B vitamins (Neuromultivit, Milgamma) – restore the function of the peripheral nervous system, reduce pain;
- anesthetic blockades - solutions of Novocaine or Lidocaine are injected into the most painful points.
- To restore joint function:
- chondroprotectors - medications that restore cartilage tissue in the form of tablets, injections, ointments (Dona, Structum);
- hyaluronic acid - the introduction of drugs based on it into the joint cavity, for example, in the treatment of arthrosis of the knee joint; this helps improve the viscosity of the synovial fluid and reduce injury to the articular surfaces of the bones.
Drugs for the treatment of arthrosis
Traditional methods
It is better to learn how to treat arthrosis with these methods by consulting your doctor. The most popular methods:
- inclusion of gelatin in the diet; every day you need to eat soup (borscht) with bone broth, jellied meat, jelly - this helps restore bone tissue;
- externally: compresses based on kefir, chalk and oatmeal; mix all components in equal volumes; put the mushy mass on a napkin, apply it to the knee joint when treating it, cover the top with polyethylene, insulate it and leave it overnight; relieves pain, stimulates the turnover of cartilage tissue.
Non-drug treatments
These methods are no less important. Physical therapy (physical therapy) helps. One of the main recommendations of experts is physical activity. In this case, the correct balance between light physical activity and rest must be maintained. This is achieved by daily performing a complex of therapeutic exercises prescribed by a doctor. In order to perform exercises correctly with a gradually increasing load, they begin to be done under the supervision of a physical therapy instructor and only then proceed to be performed at home. It is better to entrust the choice of exercises to a physical therapy instructor.
Basic training rules:
- classes should be held daily;
- all movements are carried out smoothly, without sharp turns;
- If the pain intensifies, stop the exercises.
You cannot: run, jump, play football, basketball, volleyball and other outdoor sports games, lift weights, stand for a long time or be in any other static position.
Sports activities include swimming classes, yoga and Pilates exercises specially selected by the instructor.
If pain bothers you: limit physical activity for a while, provide rest to the sore limb several times a day for 20-30 minutes, but you should not rest for a long time. Rest should be replaced by light physical activity that does not cause increased pain. If the pain is severe, then it is better to move with a cane or on crutches.
Massage courses are prescribed in the absence of an inflammatory process. Massage allows you to restore blood circulation, innervation and metabolic processes, promotes the regeneration of damaged joint tissues. The tissues are warmed up, muscle spasms and associated pain are relieved.
Physiotherapy is prescribed depending on the patient’s condition and the causes of arthrosis:
- for severe pain - electrophoresis or phonophoresis with solutions of painkillers (Novocaine);
- in the absence of inflammation - warming procedures - applications with paraffin, ozokerite;
- to improve blood circulation, eliminate muscle spasms - darsonvalization - exposure to pulsed currents of high frequency and low strength;
- for the regeneration of articular tissues – laser and magnetic therapy;
- to restore muscle volume and strength - electrical myostimulation.
Hirudotherapy is the treatment of arthrosis with leeches. Leech saliva contains enzymes that help dilate blood vessels, which leads to increased metabolism. In addition, enzymes in the saliva of leeches are able to dissolve necrotic tissue and cleanse the joint cavity.
Various methods of fixing joints - the correct functioning of the limb depends on this. Patients with severe pain and joint instability are prescribed:
- wearing orthoses - special devices that support the limb in the correct position;
- the use of taping - fixing the joint in the desired position using adhesive tapes;
- wearing elastic knee pads in the treatment of arthrosis of the knee joint, fixing the knee and protecting it from injury;
- use of walking aids such as canes and crutches.
Taping procedure for arthrosis of the knee joint
Operation
In case of persistent loss of function and severe pain that is not amenable to conservative treatment, an endoprosthetic operation is performed - replacing the destroyed joint with an artificial one.
How is osteoarthritis of the joints treated?
The treatment plan is determined individually, taking into account factors such as:
- collected anamnesis;
- existing complaints;
- results of diagnostic examination;
- individual characteristics of the patient.
In order to achieve the most effective result, complex treatment is used, involving procedures such as:
- drug therapy (taking drugs from groups: analgesics, glucocorticosteroids, muscle relaxants, chondroprotectors) – aimed at preventing the development of pathological and activating regenerative processes;
- physiotherapeutic methods (massage, physical therapy, exposure to electric current/magnetic field, etc.) - play the role of supportive therapy, providing the opportunity to accelerate conservative treatment and activate regenerative processes;
- surgical intervention (endoprosthetics, etc.) is important when diagnosing advanced cases. Such a radical method involves removing the source of pathological processes followed by plastic surgery of the affected fragment of the joint.
It is worth noting that drug therapy plays a vital role in the treatment of osteoarthritis, because by taking drugs it is possible not only to get rid of symptoms, but to literally eradicate the problem/its consequences.
One of the most significant groups of drugs is considered to be chondroprotectors, which help joint tissues regenerate. The most commonly prescribed drug is considered to be Artracam.
Approach to treating the disease in our clinic
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis
The Paramita clinic uses an individual approach to the treatment of arthrosis. After a preliminary examination, the most appropriate course of treatment is selected for the patient, including:
- the most modern methods of drug and non-drug therapy, based on the achievements of Western medicine;
- traditional oriental methods, successfully used for centuries by doctors of Ancient China and Tibet to treat diseases of the musculoskeletal system; treatment is based on restoring the energy balance of the entire body, leading to suppression of the pathological process.
Medical doctors successfully use all the necessary methods for treating arthrosis, achieving complete relief of patients from pain and stopping the progression of the disease.
Prevention of osteoarthritis
To prevent osteoarthritis, you need to lead a healthy lifestyle. Compliance with an orthopedic regimen, physical therapy, proper nutrition, rest and sleep patterns - all this will help keep your joints healthy for many years.
The MedicCity clinic pays special attention to the diagnosis and treatment of osteoarthritis, gout, osteoporosis, lupus erythematosus and other rheumatoid diseases.
We take a comprehensive approach to maintaining the health of patients: after treating the underlying disease, you can take courses in massage, manual therapy, physical therapy, etc.
Easy movement for you and your joints!
Clinical recommendations for arthrosis
To get rid of pain and maintain normal condition of the musculoskeletal system, you need to:
- monitor your body weight – extra pounds significantly increase the risk of disease progression;
- get rid of heavy physical activity: heavy lifting, long walking, and especially long periods of standing;
- regularly perform physical therapy exercises;
- avoid injury; To do this, during training, gradually increase the load on the muscles, and also use special protective devices (knee pads, etc.);
- use special devices and techniques to restore impaired limb biomechanics (orthoses, taping);
- regularly visit your doctor and conduct courses of anti-relapse treatment.
Prognosis for arthrosis
With proper treatment of arthrosis and the patient following all the doctor’s recommendations, the progression of the disease and impairment of joint function can be stopped. It is also quite possible to completely relieve the patient of pain.
Prevention of arthrosis
To prevent arthrosis, you need to move more, avoid heavy physical activity and stick to a low-calorie diet so as not to gain weight.
2. Causes of arthritis (osteoarthritis)
There are several factors that increase your chance of developing arthritis:
- Heredity
. Some people have an inherited defect in one of the genes responsible for the formation of cartilage. This can cause rapid wear and tear on the joints. Those who were born with spinal curvature or scoliosis are prone to developing spinal osteoarthritis. - Obesity
. Obesity increases the risk of developing arthritis in the knee, hip and spine due to the excess stress of body weight on the joints. - Injuries
. Injuries can also affect the development of the disease. For example, athletes who have had a knee injury often develop knee arthritis. People who have had serious back injuries may be predisposed to developing osteoarthritis of the spine. A bone fracture can cause arthritis in the joint near the fracture site. - Excessive load on the joint
. Increased stress on a joint increases the risk of arthritis. For example, people whose jobs require constant bending of the knee are more likely to suffer from osteoarthritis of the knee. - Other diseases
. People with rheumatoid arthritis, the second most common form of the disease, are also prone to developing osteoarthritis. In addition, certain conditions, such as too much iron in the body or excess growth hormones, contribute to the development of osteoarthritis.
Visit our Rheumatology page
Frequently asked questions about the disease
Arthritis and arthrosis – what is the difference?
The difference is that arthritis is an inflammatory process in the joint, and arthrosis is degenerative-dystrophic (metabolic) with gradual “drying out” and cracking of cartilage, compensatory growth of bone tissue. Chronic arthritis gradually turns into arthrosis-arthritis and arthrosis.
Is it possible to warm joints in a sauna/bath if you have arthrosis?
It is possible and it will be beneficial. But arthrosis is often complicated by inflammation (arthritis), in which warming water procedures are contraindicated. Therefore, before you start treating arthrosis with water procedures, it is better to visit a doctor.
Do they take you into the army with arthrosis?
It depends on how pronounced it is. If the function of the joint is impaired, then no.
Is it possible to develop arthrosis after coronavirus infection? If not, why not?
It is unlikely that anyone will answer this question now, there is simply no data. The development of arthrosis is a slow process.
Which doctor should I contact for arthrosis?
To a therapist. He will conduct an examination, a preliminary examination and, depending on the type of arthrosis, will refer the patient to an orthopedic traumatologist or rheumatologist.
Does arthrosis occur in children?
It happens after injuries and joint diseases.
Arthrosis is not a death sentence. It cannot be completely cured, but it can and should be treated - this will save patients from suffering. Moscow medical specialists successfully cope with the treatment of arthrosis.
Literature:
- Karateev A.E., Barskova V.G. Criteria for choosing a non-steroidal anti-inflammatory drug. Handbook of a practical doctor, 2007.- T. 5.- No. 5.- P. 13-17.
- Povoroznyuk V.V. Osteoarthritis: modern principles of treatment // News of medicine and pharmacy. - 2004. - T. 144, No. 4. - P. 10-11.
- Raisz LG Prostaglandins and ione: physiology and pathophysiology. Osteoarthritis Cartilage, 1999.- V. 79.- P. 83-94.
- Peyron JC, Altman RD Osteoarthritis: diagnosis and medical surgical management. — 2nd ed. - Philadelfia, Pa: WBSauders Company, 1992. - P. 15-37.
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 04/22/2021 Date of update: 04/11/2021
Reader rating
Rating: 4.29 / 5 (7)
Diet
Proper nutrition is not the main factor in the prevention of osteoarthritis, but it will also make its contribution to maintaining healthy joints. Recommended:
- a diet balanced in calories, macro- and micronutrients;
- sufficient amounts of vitamins and minerals;
- exclusion of spicy, canned, excessively fatty foods, alcohol, as well as products with artificial flavors and dyes;
- minimizing fast carbohydrates.
Collagen and omega-3 acids have a good effect on the condition of cartilage, which is why aspic and sea fish and olive oil should always be present in the diet.