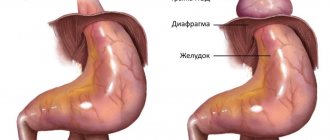
Femoral hernia is a tumor-like protrusion formed when intestinal loops and omentum exit the abdominal cavity through the femoral ring. It is manifested by the presence of a sac-like protrusion in the area of the femoral triangle in a vertical position of the body, pain. If a hernia is strangulated, intestinal obstruction may develop. A femoral hernia is recognized during an examination by a surgeon and additional diagnostics - ultrasound of the hernial protrusion, irrigoscopy, herniography, ultrasound of the pelvis and bladder. If a defect is identified, a hernia repair operation (hernioplasty) is performed.
General information
In this article, we will look at a hernia of the inguinal-femoral zone, namely, a femoral hernia and hernias of other parts of the body that are relatively rare, in particular the knee joint - Baker's hernia (cyst), muscle hernia and coccyx hernia.
Femoral hernia
Femoral hernia in men and women accounts for 5-8% of all abdominal hernias. Significantly more common in females, predominantly mature/elderly (80%), less common in young multiparous women. The female/male sex ratio in various studies varies from 1.8:1 in the USA/European countries to 4:1 (in the Russian Federation), which is due to the greater width of the female pelvis, which is the cause of the relative weakness of the Pupart ligament and the greater severity of the vascular/muscular lacunae. Femoral hernias in women are prone to more frequent parietal strangulation than other hernias (umbilical/inguinal).
A femoral hernia is a protrusion located in the lower abdomen, caused by the exit of internal organs through the femoral canal beyond the abdominal wall.
Anatomically, the femoral canal is normally absent and is formed only during the formation of a hernial protrusion. The weakest point is the area located directly under the inguinal ligament (between the pelvic bones and the inguinal ligament). This space is divided by the iliopectineal fascia into muscular/vascular lacunae. The muscular lacuna contains the femoral nerve/iliopsoas muscle, and the vascular lacuna contains the femoral vein/artery. The space between the lacunar ligament and the femoral vein is filled with fibrous connective tissue and a lymph node . It is through this gap that the femoral hernia emerges and is called the femoral ring . That is, in most cases, a hernia is formed in the area of the vascular lacuna. A strand of the omentum and part of the small/large intestine most often enter the hernial sac. In women, the fallopian tube, bladder and ovary may additionally enter the hernial sac. The formation of protrusions in the anatomical region of the muscle lacuna occurs extremely rarely, since it is limited by a strong fascial layer. The external opening of the femoral canal is the fossa oval, which is located on the lata fascia of the thigh.
Anatomically, a femoral hernia does not differ from other abdominal hernias and includes the hernial orifice, hernial sac, hernial membranes and hernial contents. The development of a femoral hernia includes several stages:
- Initial stage - the hernial protrusion does not protrude beyond the femoral ring and is not clinically manifested.
- Canal stage - the protrusion is already located in the femoral canal, but does not protrude beyond its boundaries.
- Full stage - the hernial sac visually protrudes under the skin from the femoral canal in the area of the inguinal fold of the thigh.
As a rule, a hip hernia is diagnosed in the full stage.
Baker's hernia
According to their shape, cysts are classified as crescent-shaped, grape-shaped, slit-shaped, oval and horseshoe-shaped cysts.
Becker's hernia (below the knee)
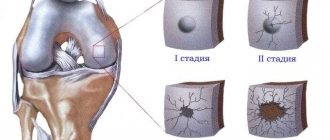
Baker's hernia (synonyms - Baker's cyst, popliteal hernia, popliteal bursitis, synovial cyst of the popliteal region) is an elastic protrusion (formation) in the area of the popliteal fossa, formed as a result of the inflammatory process in the knee joint (photo below).
The incidence of synovial cysts among pathologies of the knee joint varies from 3.4% to 20.8% and are most often found in rheumatic diseases , as well as in patients with gonarthrosis at various stages of the degenerative-dystrophic process. Popliteal hernia is much more common in women, accounting for 68.9% of cases. It can exist either for a short period of time due to the resorption of fluid with its reverse development until it completely disappears, or it can be chronic for life in cases of the development of persistent synovitis of the joint .
The size of Baker's cysts varies significantly: in most patients (68.5%) the cyst volume is up to 10 ml; in 25% of cases their volume exceeds 50 ml. As a rule, Baker's cyst is single-chamber; multi-chamber cysts are extremely rare.
Essentially, a Baker's cyst (BC) is a synovial bursa of the popliteal fossa, distended with fluid, which is localized in the medial part of the popliteal fossa between the semimembranosus and the inner head of the gastrocnemius muscle, communicating through the anastomosis with the knee joint.
The number/size of bursae communicating with the cavity of the knee joint varies significantly, of which the most constant are:
- Bursa of the semimembranosus muscle (located in the area of the medial femoral condyle between the medial head of the gastrocnemius and the tendon of the semimembranosus muscle).
- The medial bursa of the gastrocnemius muscle (localized between the capsule of the knee joint and the beginning of the medial head of the gastrocnemius muscle.
- The popliteus muscle bursa is always located at the level of the inferolateral inversion, between the tendon of the femoral muscle and the posterior wall of the inversion.
- The density of the joint capsule of the knee joint is not the same in a number of places, and the space between the ligaments of the posterior part of the joint is especially weakened, which becomes the most common place for a hernia of the synovial membrane of the joint. As cysts grow, they can compress the anatomical formations located in it (neurovascular bundle), causing various neurovascular disorders in the distal parts of the legs.
- Baker's cysts can significantly limit the functions of the knee joint, compress the neurovascular bundle in this area, and less often, their dissection or rupture is observed.
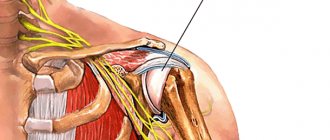
Muscle hernia
It occurs due to a rupture of the muscle fascia, mainly as a result of injuries (sharp jerk, strong blow, dislocation, falling of a heavy object). When it ruptures, muscle fibers protrude into the resulting opening, that is, a muscle hernia is formed, which can have very different localizations. The main manifestation of this type of hernia is a protrusion, which can appear when the muscle is tense or be permanent. Swelling is characteristic at the site of the protrusion and in the immediate area, which can compress the nerve fibers/surrounding tissues.
Patients are concerned about pain in the area of injury, decreased mobility, numbness and tingling in the damaged muscle. For serious fascial tears, surgical treatment is performed; for minor injuries, painkillers, anti-inflammatory drugs are prescribed, and specially selected compression stockings/bandages are worn, which reduce the load on the muscles and adjacent tissues and allow the muscle to take a physiologically normal position.
Coccyx hernia
The coccyx area often becomes a target for the formation of hernial pathology of the spine, the peculiarity of which is that it is formed not due to protrusion of the disc nucleus, as hernias form in other parts of the spinal column, but due to a tear in the fibrous membrane. It manifests itself as pain when sitting on a hard surface, pressing on the tailbone area, during childbirth. The pain may radiate to the groin, anus, or thighs (coccydynia). Diarrhea , constipation , difficulty urinating, cramps in the thighs and calf muscles, and numbness of the legs may also appear Treatment is predominantly conservative, in severe cases - surgical intervention.
Pathogenesis
Femoral hernia
The pathogenesis of a femoral hernia is based on the discrepancy between the strength of the muscular aponeurotic structures of the anterior abdominal wall and the pressure of the internal organs on it, that is, the main factor in hernia formation is the “anatomical prerequisites” that develop against the background of connective tissue pathology, manifested by quantitative changes in the ratio of mature collagen , which is the basis of strength various framework connective tissue elements (tendons, aponeuroses, ligaments).
Changes can occur in the process of collagen “maturation” in the form of slowing down the process or increasing the process/rate of its breakdown. Such processes lead to the prevalence of relatively thin/less strong collagen in connective tissue structures, which leads to a decrease in the resistance (resistance) of the abdominal wall structures. Such processes are the basis for the formation of a hernia. Increased collagen breakdown and a shift in balance towards immature forms can be facilitated by significant physical activity, alcohol, smoking and some toxins, and the process can also be congenital.
Becker's hernia
There are different views on the mechanism of cyst formation. Today, the most recognized by scientists is the valve mechanism of penetration of articular fluid from the cavity of the knee joint into the articular joint through the anastomosis, while the reverse flow of fluid into the joint cavity from the articular cavity is difficult. The immediate causes of unidirectional fluid flow can be:
- compression of the anastomosis directly by the enlarged knee joint itself or by the tendons of adjacent muscles at the moment of extension in the knee;
- compression of the anastomosis by a fold of the articular capsule, which can act as a valve flap;
- obstruction of the anastomosis with cellular detritus/fibrin masses;
- less often, the cause of obstruction of the anastomosis can be chondromic bodies that are located in the cyst cavity.
Classification
Femoral hernia
Based on the location of the exit gate, several types of femoral hernia are distinguished:
- Typical femoral hernia (exits through the inner part of the vascular lacuna, which turns into the femoral canal).
- Femoral lacunar ligament hernia (exits directly through a defect in the lacunar ligament).
- Femoral-total hernia of the vascular lacuna (the protrusion occupies the entire vascular lacuna).
- Femoro-intravaginal hernia of the vascular lacuna (exits in the area of the vagina itself).
- Femoral-lateral hernia of the vascular lacuna (exits between the artery of the iliac and pectineal ligament on the lateral side).
- Hesselbach's hernia (femoral hernia of the muscle lacuna) is formed in the area of the femoral nerve.
Based on the location of hernial protrusions, they are divided into:
- unilateral femoral hernias, 60% of which are hernias on the right and 30% on the left;
- bilateral femoral hernias account for about 10%.
Taking into account the clinic, the following are distinguished:
- reducible (retracts into place at rest on its own);
- irreducible (does not disappear when changing body position);
- disadvantaged.
Becker's hernia
Highlight:
- Primary Baker cysts, the formation of which occurs in the absence of any intra-articular pathology (found in children/adolescents).
- Secondary Baker cysts (formed due to damage to intra-articular structures).
According to their shape, cysts are classified as slit-shaped, crescent-shaped, oval, grape-shaped and horseshoe-shaped cysts.
Surgeries for femoral hernias
The essence of the intervention is that the surgeon excises the hernial sac, returns the displaced organs to their normal anatomical position and closes the hernial orifice. Femoral canal plastic surgery is performed using two techniques:
- The defect is sutured with a special material using the patient’s own tissue.
- The femoral canal is closed with a mesh implant (tension-free hernioplasty).
Specialists at the GMS Hospital Hernia Treatment Center prefer a low-traumatic, gentle surgical technology, which is tension-free hernioplasty.
Causes
Femoral hernia
The reasons for the weakening of the muscular-ligamentous frame of the inguinal-femoral zone and the formation of femoral hernias are:
- Weakening of the structural elements of the abdominal wall, caused by excess body weight, rapid loss of body weight, multiple pregnancies, injuries to the abdominal wall, and failure of the surgical suture.
- Connective tissue dysplasia with a pronounced decrease in the strength of the ligamentous apparatus due to a congenital defect.
- Atrophy of abdominal wall structures due to low motor activity/neurological diseases.
- Weakness of the ligaments of the abdominal wall caused by heavy physical work/sports.
- The occurrence of protrusion itself is associated with an increase in intra-abdominal pressure, which is caused by chronic constipation , persistent cough, and single/systematic excessive physical effort.
Baker's hernia
The main causes of Baker's cyst development are injuries/diseases of the knee joint:
- traumatic damage to the structures of the knee joint (cartilage, menisci, ligaments);
- meniscus degeneration;
- chronic synovitis (inflammation of the synovial membrane);
- osteoarthritis / arthrosis / osteoarthrosis ;
- rheumatoid arthritis;
- as a complication after diseases ( psoriasis , hemophilia , lupus , bursitis , etc.).
Symptoms
Symptoms of a femoral hernia
The symptoms of a femoral hernia in men and the symptoms of a femoral hernia in women are identical. Symptoms are determined by the stage of development of the hernia, size, reducibility of the protrusion, the presence of complications and the nature of the prolapsed tissues/organs. The main symptom of a complete femoral hernia in men and women is a small hemispherical protrusion located in the femoral-inguinal flexion area (inward of the femoral vessels under the inguinal ligament). Hernial protrusion is clearly visible visually when the body is in an upright position, and especially when straining (photo below).
In uncomplicated cases, it disappears upon self-reduction, sometimes with rumbling. Percussion over the protrusion - a tympanic sound, a characteristic positive symptom is a cough impulse, dysuria . The occurrence of pain is usually associated with partial short-term strangulation of the contents of the hernia.
Baker's hernia
With a small size of Baker's cyst, it is not visually detectable, painless, palpation is difficult, and against the background of symptoms of diseases of the knee joint, the specific clinical picture of KB is practically absent. As it reaches a larger size, it is clearly visually defined and palpated in the form of an oblong-ovoid, densely elastic tumor-like formation, localized mainly in the medial parts of the popliteal region (up to 90% of cases).
Due to the presence of a mechanical obstacle to the function of flexion in the knee joint, patients complain of discomfort, pain during physical activity along the posterior surface of the joint and the presence of a tumor-like formation in the popliteal fossa. The main symptoms, besides pain, are:
- feeling of pressure in the popliteal fossa;
- presence of swelling;
- difficulty moving in the knee joint, less commonly - periodic blockades of the joint.
Also, the symptom complex may additionally include pain in the calf muscles and impaired sensitivity of the back of the lower leg, which manifests itself more often after going up and down stairs/long walking. Symptoms can be either isolated or combined with symptoms of diseases of the knee joint or intra-articular pathology (damage to intra-articular structures, rheumatoid arthritis , osteoarthritis ).
Femoral hernia repair with mesh
The operation is carried out in two ways:
- Open hernioplasty is performed through a small incision in the inguinal-femoral fold. The surgeon opens the inguinal canal, isolates and drains the defect, and then strengthens the canal with a mesh endoprosthesis.
- Laparoscopic hernioplasty - the intervention is carried out using endoscopic equipment through small punctures into which surgical instruments are inserted.
The surgeon determines the method of intervention after examination. How the operation will be performed depends on the stage of the disease, the size of the hernial sac, the severity of clinical symptoms, the presence of complications and other factors.
Tests and diagnostics
Femoral hernia
Early forms of femoral hernias present difficulties for their diagnosis, but diagnosing a complete hernia based on patient complaints and physical examination data does not cause significant difficulties. Of the instrumental methods, the most informative and mandatory is ultrasound, which makes it possible to identify their contents.
If necessary, the following may be prescribed: cystography , colonoscopy , cystoscopy , irrigography , CT . Differential diagnosis includes inguinal hernia , femoral artery aneurysm , abscess / tumor , thrombophlebitis .
Baker's hernia
The diagnosis is made on the basis of complaints, visual examination and palpation of the knee joint. Ultrasound/MRI are used as instrumental methods.
Treatment of femoral hernias at GMS Hospital
The minimally invasive surgery technologies used by surgeons at the Hernia Treatment Center at GMS Hospital will help quickly and safely eliminate the defect, eliminating the risk of postoperative complications. The use of mesh (including three-dimensional) endoprostheses from well-known manufacturers allows us to eliminate the risk of relapse of the disease, and the use of microsurgical techniques reduces the length of hospital stay to 1 day.
The rehabilitation period is easy, and full recovery takes only 3-6 weeks. You can learn more about the operation and the need for one or another diagnostic procedure at a consultation with a surgeon. You can make an appointment with a doctor by phone or by leaving an online application on the website.
Diet
There is no diet as such for a femoral hernia, however, such patients need a diet correction that ensures normal daily bowel movements without constipation and flatulence , which contribute to increased pressure inside the abdominal cavity and an increase in protrusion. For this purpose, foods high in fiber (vegetables/fruits) that enhance intestinal motility are introduced into the diet: seaweed, beets, pumpkin, apricots, plums, peaches, figs, prunes, and the consumption of cabbage, yeast baked goods, kvass, and legumes that cause flatulence is reduced. (diet for constipation). If you are overweight, a rational diet for weight loss .
Cost of treatment for femoral hernia
The prices indicated in the price list may differ from the actual prices. Please check the current cost by calling +7 495 104 8605 (24 hours a day) or at the GMS Hospital clinic at the address: Moscow, st. Kalanchevskaya, 45.
| Name | Price |
| Hernia repair for femoral hernia | 100,002 rub. |
| Laparoscopic repair of inguinal, umbilical or femoral hernia | 120,001 rub. |
Dear Clients! Each case is individual and the final cost of your treatment can only be found out after an in-person visit to a GMS Hospital doctor. Prices for the most popular services are indicated with a 30% discount, which is valid when paying in cash or by credit card. You can be served under a VHI policy, pay separately for each visit, sign an agreement for an annual medical program, or make a deposit and receive services at a discount. On weekends and holidays, the clinic reserves the right to charge additional payments according to the current price list. Services are provided on the basis of a concluded contract.
Plastic cards MasterCard, VISA, Maestro, MIR are accepted for payment. Contactless payment with Apple Pay, Google Pay and Android Pay cards is also available.
Western standards of treatment (evidence-based medicine)
Continuous staff development
Regular interaction with leading Russian and foreign medical institutions
Modern medical equipment and advanced diagnostic and treatment methods
Unified standard of service
We work around the clock 24/7/365
Make an appointment We will be happy to answer any questions Coordinator Oksana
Prevention
Nonspecific preventive measures to reduce the risk of developing a femoral hernia include: maintaining the muscles of the lower abdomen in proper shape (training the abdominal muscles), wearing bandages during significant physical activity/pregnancy, balanced nutrition, timely/adequate treatment of diseases of the genitourinary tract/intestines, refusal smoking to prevent chronic cough.
Prevention of Baker's cyst comes down to:
- Timely/adequate treatment of knee joint diseases.
- Monitoring body weight and correcting it if necessary.
- Controlling the load on the knee joint.
- Regular exercises for joints.
Preparing for surgery
During the consultation, the surgeon will prescribe a set of necessary examinations:
- ECG.
- X-ray of the lungs or fluorography.
- Blood and urine tests - general, biochemical.
- Blood tests for hepatitis, HIV, syphilis, coagulation, blood group and Rh factor.
You should definitely tell your doctor about the medications you are taking; you may have to stop them for a while. Your doctor will tell you more about preparing for surgery during your consultation. You can undergo a comprehensive examination at GMS Clinic in 1 day.
Consequences and complications
Femoral hernia
The main complications of a femoral hernia include: inflammation of the serous/purulent type, coprostasis and strangulation of the hernia. The inflammatory process most often begins with the contents of the hernial sac (part of the intestine, appendix, uterine appendages, etc.), much less often the inflammatory process passes to the hernial sac directly from the skin. skin hyperemia occurs , the inflamed hernia becomes swollen, pain appears/intensifies, and body temperature may rise. An extremely dangerous complication is the development of peritonitis .
In cases of strangulation of the femoral hernia, an acute disruption of the innervation/blood supply to the organs/tissues of the hernial contents develops extremely quickly. The hernia sharply increases in size, becomes dense, unreducible, and sharply painful on palpation. Severe pain occurs in the pinched area, and there is retention of stool and gases. With prolonged strangulation there is a high risk of developing intestinal obstruction .
Baker's hernia
Baker's cyst, in the absence of timely/adequate treatment, can provoke:
- compression of the neurovascular bundle (tibial nerve, lymphatic/blood vessels, which appears as numbness, muscle weakness in the knee joint, swelling/pain of the lower leg;
- deep vein thrombosis and thrombophlebitis of the vessels of the leg , the development of varicose veins of the saphenous veins of the leg;
- rupture of the cyst, caused by high pressure as the tumor increases, with the contents of the cyst spilling into the intermuscular space of the upper third of the leg, which is manifested by swelling, pain, redness and increased temperature.
Forecast
Femoral hernia
With a non-strangulated femoral hernia, in most cases the prognosis is favorable and after suturing the hernia the patient returns to his usual lifestyle. In the absence of timely treatment, there is a risk of the formation of an irreducible hernia, and in 80-90% of cases strangulation occurs.
Baker's hernia
Cysts that have formed recently (usually after excessive physical strain on the knee joints) are characterized by a benign outcome. In the presence of persistent synovitis of the joint, the cyst becomes chronic and its contents are joint fluid. In chronic cases, the fluid in the joint capsule is partially resorbed, which leads to its thickening. With a long course, daughter cysts, synechiae and septa can form. In cases of rapid accumulation of effusion, rupture of the cyst is possible with the spread of articular fluid through the interfascial spaces of the lower leg.
Why surgery is needed
- A conservative approach to the treatment of femoral hernias is not effective.
- The hernial sac that slips through the femoral ring enlarges over time and ceases to be reduced.
- Even the smallest protrusion is often complicated by pinching.
At the GMS Hospital Hernia Treatment Center, treatment of femoral hernias is carried out using hernioplasty, which provides the following advantages:
- The use of microsurgical techniques and modern mesh devices allows minimizing trauma to the patient’s tissues.
- Stay in the hospital for no more than 1-3 days (depending on the scope of the intervention).
- Full recovery after surgery takes only 3-6 weeks.
List of sources
- Zatsarinny V.V., Muravyov S.Yu., Uspensky I.I. Morphological changes in the abdominal muscles in hernia patients. Current issues of clinical and experimental medicine: collection. abstract conf. young scientists. St. Petersburg; 2011:164-166.
- Styazhkina S.N. Abdominal hernia: textbook / comp. S.N. Styazhkina, V.A. Sitnikov, M.N. Klimentov et al. Izhevsk, 2011. 86 p.
- Makushin V.D., Danilova I.M. Backer cyst (review of the problem according to the literature) // Genius of Orthopedics. - 2000. - No. 1. - P. 110-113.
- Kamshilov B.V. Types of synovial cysts in the popliteal region // New Horizons: IV Trans-Ural. festival of scientific research, technical and applied creativity of youth: Abstracts. report region scientific-practical conf. - Kurgan, 2002. - Part 2. - P. 95-96.
- Mironov S.P., Orletsky A.K., Nikolaev K.A. Modern approaches to the diagnosis and treatment of popliteal cysts. Kremlin Medicine 2005; 2:33–6.
Advantages of tension-free hernioplasty
Modern medicine has improved many surgical techniques for hernia repair, and one of the most minimally traumatic options is tension-free hernioplasty. This technique has undeniable advantages:
- Mild pain syndrome
- Fast rehabilitation (hospital stay is reduced to 1 day)
- No risk of relapse
- 2-3 weeks are enough for complete recovery
The entire operation lasts less than an hour and has an excellent cosmetic effect.