Every expectant mother eagerly awaits the birth of her baby. During pregnancy, many people experience various fears. A woman thinks about whether her baby is developing correctly, worries whether he has genetic diseases, whether everything is in order with the internal organs and anatomical structure. Unfortunately, these fears are unfounded. congenital hip dislocation is quite often diagnosed in newborns . This is not a dangerous pathology, it can be corrected and goes away without a trace if the disorder is detected in time and treatment is started, and the parents follow all the doctor’s recommendations.
What is congenital hip dislocation
A hip dislocation is a displacement of the femur relative to the acetabulum. The femoral head is normally located at the time of birth in a practically formed glenoid cavity. The geometry of a newborn's joint is different from that of an adult. It is an immature biomechanical structure with its own characteristics: the head of the femur and the glenoid cavity consist mainly of cartilaginous tissue, they have not ossified (therefore are not clearly visible on x-rays), the cavity still has a flattened shape, the ligaments are weak and overly elastic. Therefore, the joint is not firmly held in the cavity.
With various malformations of the femoral bone and glenoid cavity, the head is displaced vertically or laterally, that is, the joint does not articulate. In this case, instability of the joint occurs, and there may be subluxation or dislocation of the hip.
Why does congenital hip dislocation occur in a child?
Medicine still cannot name the exact reasons for the development of intrauterine dysplasia. But there are known provoking factors that greatly increase the risk of congenital hip dislocation. These include:
- hereditary predisposition;
- complicated pregnancy with toxicosis;
- large fruit;
- breech rather than cephalic presentation;
- female sex of the fetus.
These factors increase the likelihood of joint dysplasia, which leads to congenital hip dislocation in newborns.
The intrauterine developmental defect itself can be expressed in various deviations from the norm:
- acetabular dysplasia - a defect in the acetabulum, in which the head of the femur should be located (the socket is slanted or flattened)
- proximal dysplasia – underdevelopment or abnormal development of the femoral neck, change in the value of the neck-diaphyseal angle (the angle between the central axis of the femoral neck and the midline of the diaphysis)
- rotational dysplasia with various types of violation of joint geometry in the horizontal plane (manifests later as clubfoot)
That is, any underdevelopment, pathology of unformed structures leads to the fact that the head is not held in the articular cavity, the femur is displaced upward or laterally (goes outward), the articular capsule is inverted or deformed, and the joint itself is unstable.
Degree of pathology
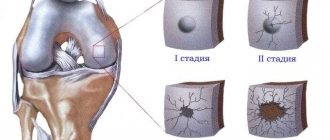
Since joint immaturity can be expressed by various abnormalities, disorders are classified according to severity:
- A – normal joint without disorders;
- B – pre-dislocation: there are non-critical disturbances in the anatomical structure of the joint. The head is in the glenoid cavity, but is held weakly.
- C – subluxation: the femur is displaced, there is a valgus deformation of the glenoid cavity. This is the so-called borderline state, in which there is a high probability of developing pathologies in the future.
- D – congenital dislocation of the hip: the head of the bone is located outside the acetabulum.
How is the disease diagnosed?
To identify congenital anomalies of the hip, the following methods are used:
- examination and comparison with the norm of the location of skin folds and the length of the legs;
- feeling (palpation) of the head of the bone;
- performing hip abduction tests.
Using them, you can independently identify hip dislocation in children. To confirm the diagnosis and establish the stage of the disease, it is necessary to conduct an instrumental examination:
- Ultrasound;
- radiograph;
- CT;
- MRI.
Subluxation and dysplasia can only be determined using radiation methods. The diagnosis is made by an orthopedic surgeon.
Diagnosis of congenital hip dislocation
An immature joint that has not yet formed at the time of birth or has an anatomically incorrect shape can be suspected immediately after birth, even in the perinatal center. External manifestations of congenital hip dislocation in newborns and children of the first year of life:
- asymmetrical skin folds on the legs (one inguinal and/or gluteal fold is deeper than the other, located higher or lower)
- shortening of the leg (with straight legs, one knee is higher than the other)
- limited mobility of the joint, in which the hip is not sufficiently abducted to the side (normally, in a newborn, the legs are separated by 80-90°, after six months - by 60-70°. If the hip is abducted by 50° or less, then it is necessary to show the child to an orthopedist and share with him with his observations)
- symptom of a click or slipping (when the child’s hip is abducted to the side, a characteristic click appears - the head is mobile and is not held in the articular cavity, it slips)
However, none of these signs by themselves is sufficient reason to make a diagnosis. For diagnosis, the child is prescribed an x-ray or ultrasound. Since the cartilage tissue in young children has not yet ossified, the picture is “read” using special tests - schematic axes are drawn through certain points of the cartilage and bones, which make it possible to measure two values: h and d. They talk about displacement of the femoral head, which can be used to judge whether it is normal or pathological.
Ultrasound of joints is a safer and no less accurate diagnostic method than x-rays. Therefore, it is now used much more often.
Pathology of the hip joints in children
Congenital hip dislocation is the most common congenital deformity of the musculoskeletal system. This malformation extends to all elements of the hip joint: the acetabulum, the head of the femur with surrounding muscles, ligaments, and capsule and consists in the underdevelopment of these tissues.
PATHOLOGY OF THE HIP JOINTS
Congenital hip dislocation is the most common congenital deformity of the musculoskeletal system. This malformation extends to all elements of the hip joint: the acetabulum, the head of the femur with surrounding muscles, ligaments, and capsule and consists in the underdevelopment of these tissues. Emerging congenital hip dislocation occurs in 5 per 1000 children. The incidence of congenital hip dislocation varies in different countries, as it depends on climatic conditions and national customs. Thus, in Georgia in some areas it reaches 9% per 1000 children due to the traditional tight swaddling of babies and is not found at all among the black population of Africa, in Korea, Vietnam and generally throughout the entire Indochina Peninsula, where, due to the hot climate, children are not swaddled tightly .
Unilateral dislocation is more common than bilateral dislocation. Moreover, according to various authors, the frequency of bilateral dislocation ranges from 20 to 50%. With unilateral dislocation, the left side is 1.5-2 times more common than the right side. In girls, congenital hip dislocation occurs 5 times more often than in boys.
Etiology and pathogenesis
There are a large number of different theories regarding the causes of hip dysplasia. Many of them are of historical interest and cannot explain the entire complex pathological process.
The etiological factors leading to deviations in the normal development of the hip joint and surrounding muscles are called the defect of their primary formation. Some authors see confirmation of this theory in the combination of congenital hip dislocation with other congenital deformities. Other authors consider the cause of congenital hip dislocation to be a delay in the development of the normal hip joint during the intrauterine life of the fetus. These developmental disorders are sometimes explained by fluctuations in vitamin balance, hormonal disorders and other reasons.
Depending on the period of antenatal life, the femoral head and acetabulum begin to develop without close contact with each other, and varying degrees of impairment appear. This assumption does not exclude a true malformation of the acetabulum and head, when a formed dislocation is detected already from the first days of the postnatal period. The extremely rare occurrence of such an anomaly corresponds to the rarity of detecting a true, formed dislocation in newborns.
Studies conducted jointly with the All-Union Institute of Obstetrics and Gynecology (M.V. Volkov, R.L. Gorbunova, I.P. Elizarova, 1966) showed that when examining mothers, most of them had either cardiovascular diseases (rheumatic heart disease), or toxicosis of pregnancy and nephropathy, accompanied by impaired protein and salt metabolism in both the mother and the fetus.
In 50% of all those examined, there was a breech presentation of the fetus. The relative predominance of breech presentation in cases of congenital dislocation of the hip joints makes it necessary to more carefully examine the development of the musculoskeletal system in children with this type of presentation.
The mechanism of the birth act and the nature of the obstetric aid (Tsovyanov's method and the classic manual aid) do not influence the occurrence of congenital joint pathology, since it was observed in 25 children born by cesarean section, subject to all the rules for fetal extraction. In addition, dislocation is also observed with cephalic presentation.
The pathogenesis of congenital hip dislocation is associated with previous pre-dislocation of the joint, characterized by hypoplasia of the acetabulum, its flattening, small size of the femoral head and its delayed ossification, anterior rotation of the upper end of the femur (antetorsion), anomalies in the development of the neuromuscular apparatus of the hip joint area. These changes are confirmed by pathological data: the femoral head in the first months of a child’s life is displaced outward and slightly upward. Gradually, with age, the upward and posterior displacement along the ilium increases, which is accompanied by stretching of the joint capsule. Displacement of the femoral head may be slight with subluxations and more pronounced with dislocations. Changes are observed in the shape and structure of the flattened cavity, reduced head and articular cartilage, articular capsule, ligaments and muscles.
The acetabulum is usually not only flattened, but also elongated, its superoposterior edge is underdeveloped, as a result of which the roof is sloping and there is no bone support for the femoral head on top. The flattening of the acetabulum increases due to the thickening of the cartilaginous layer of the bottom of the acetabulum and the development of connective tissue at the bottom. In older children, with the formation of a dislocation, these changes increase: the upper arch may completely disappear, the cavity takes on a triangular shape and becomes flatter; the femoral neck, which develops in the absence of support, is shortened, its neck-diaphyseal angle remains obtuse (135° instead of the normal 125°); the neck, deprived of support, rotates anteriorly.
The femoral head is smaller, deformed, and appears later. In 25-30% of children, according to F.R. Bogdanov and N.A. Timofeeva, there is a macroscopic change in the cartilage of the femoral head. When the leg is loaded with a dislocated hip, the roof of the acetabulum is even more flattened. Due to the upward sliding of the femoral head, a gliding groove is formed. The articular capsule undergoes dramatic changes; it stretches, following the head moving upward and backward, sometimes the head is soldered to the bag. The joint cavity is divided into three parts and has an hourglass shape. One part - the upper - surrounds the head, the second - a flattened cavity and remains unfilled; connective tissue develops in it. Between them there is a narrowed isthmus of the bursa, which prevents the head from moving from the upper to the lower section. The round ligament is either well or poorly expressed; after 3 years of age, in half of the cases it is absent.
Diagnostics and clinic
The outcome of the disease depends on the time when the diagnosis is made and treatment is started. It gets exponentially worse every month if no treatment is given. The diagnosis of congenital hip dislocation should be made in a maternity hospital. To do this, all children should be examined by the pediatrician of the children's room of the maternity hospital, and if in doubt, by an orthopedic consultant. In the first 3-4 weeks of life, and then again at the age of 3 months, an orthopedist examines all infants in a pediatric consultation.
The importance of diagnosing hip dysplasia in the first weeks of a child’s life is enormous, but recognition is often difficult and requires special experience and knowledge.
It is no coincidence that in recent years in Czechoslovakia, all children under 3 months of age have had an X-ray of their hip joints taken, so as not to miss the difficult-to-diagnose case of dysplasia in the hip joint.
Diagnosis of dysplasia in the first months of life
The group of hip dysplasias in young children includes diseases such as: congenital subluxation, congenital subluxation, congenital dislocation and radiologically immature hip joint.
In recent years, significant progress has been made in the early detection and early treatment of congenital dysplasia in children. A good basis for early diagnosis of diseases is a well-established relationship between orthopedists and obstetricians and pediatricians in maternity hospitals.
The simplest organizational form of early detection of congenital hip dysplasia is a systematic examination of all children born in the maternity hospital. Despite the fact that the clinic of dysplasia in the first days of a child’s life is extremely poor in symptoms, it is quite sufficient for, with a certain skill, to timely diagnose or suspect this disease.
To correctly assess the results of a clinical study, examination of a newborn must be carried out using a special technique.
- The most common symptoms of congenital hip dysplasia are:
- limitation of abduction in the hip joints;
- symptom of sliding or clicking (Marx-Ortolani symptom);
- asymmetry of the folds on the thigh and the posterior gluteal folds;
- visually detectable shortening of the lower limb;
- external rotation of the lower limb.
These symptoms must be looked for and found, since they are not always clearly expressed and to clarify them, certain skills are required in examining the child.
In a child lying on his back, there is limited passive abduction of the legs, bent at right angles at the hip and knee joints. This is the earliest and most permanent sign of congenital pathology. Abduction limitation increases over time. With normal hip joints, hip abduction will be almost complete; in the presence of dislocation or underdevelopment of the hip joint, this symptom always occurs. A sharp limitation of abduction is observed with a mature dislocation and a slight limitation with other dysplasias of the hip joint.
Limitation of hip abduction is possible with spastic paralysis, muscle contracture observed in newborns and in other joints, as well as with congenital varus deformity of the femoral neck. All these diseases must be excluded by examining the condition of all muscles and using x-rays of the hip joints. It is important to note that physiological muscle rigidity in a newborn is not permanent. At certain moments, it is possible to abduct the hips, which does not happen with dysplasia before the head is reduced.
A very important, earliest, but inconsistent symptom is the clicking symptom, or the symptom of sliding, described for the first time in 1934 by the Soviet orthopedist V.O. Marx, and independently of him the Italian orthopedist Ortolani. It is also called a symptom of instability (A.P. Biezin and K.A. Krumin). The essence of the symptom is that when the legs are abducted, the dislocation is reduced, which is accompanied by a click felt by the hand of the examining doctor. Sometimes this click can be heard from a distance. When the legs are brought to the midline, the femoral head re-dislocates, also accompanied by a clicking and shuddering of the leg. To identify this symptom, there is a special technique for examining a newborn, in which the doctor, bending both legs at the hip and knee joints, places the thumbs on the inner and the other fingers on the outer surfaces of the thighs. Slowly, avoiding forced movements, the doctor moves the hips evenly in both directions.
It should be noted that the Marx-Ortolani symptom usually disappears by the 5-7th day of a child’s life, but in some children, if muscle hypotonia is present, it may persist during the first months of life.
Asymmetry of folds on the thigh or an uneven number of folds may also indicate the presence of dysplasia. There are more folds on the dysplasia side, they are deeper than on the healthy side, and are located more proximally.
This symptom is not absolute and alone, without other data, cannot be taken into account, since it is observed only in 2/3 of patients and can occur in healthy children. When viewed from behind, the gluteal folds are not at the same level. This symptom is characteristic of unilateral hip dislocation. In addition, healthy children have deep symmetrical folds between the hips and torso at the back. The asymmetry of these folds or their absence indicates the presence of unilateral or bilateral dislocation.
One of the symptoms of hip dysplasia may be external rotation of the leg on the side of the dislocation.
It is clearly visible when the child is sleeping - mothers themselves pay attention to this symptom. Visible shortening of the lower limb, characteristic of high dislocations, can be observed not only with an obvious unilateral dislocation, but also with various dysplasias, even bilateral, but with different locations of the hips in height. It is difficult to determine the length and shortening of legs in infants using a measuring tape. The difference in leg length is judged by the different locations of the levels of the knee joints, bent and close to the stomach.
All of the listed symptoms may be observed together or only part of the symptoms may occur; in the latter case, it is better to suspect a congenital pathology of the hip joint and take an x-ray. A suspected but unconfirmed hip dislocation will only indicate the attentiveness of the doctor and will not cause harm to the child. The same disease can make a child severely disabled for life.
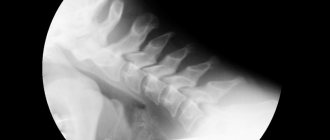
The X-ray method of examination plays a significant role in the diagnosis of hip dysplasia in newborns. During radiography, the child lies on his back with his legs extended and adducted in a position of some inward rotation, strictly symmetrically. The pelvis should fit snugly against the cassette. It is necessary to protect the genitals with a lead plate, which, if positioned correctly, does not interfere with radiography.
When X-ray diagnosing diseases of the hip joints, it should be taken into account that newborns do not have ossification nuclei of the femoral heads, and it must be remembered that the height of the femoral head is equal to the width of the femoral neck. The acetabulum is also cartilaginous and does not provide a contrasting shadow. When reading a radiograph, particular importance is attached to the condition of the upper edge of the acetabulum, the relationship of the upper end of the femur and the acetabulum. It is also important to take into account the location of the cartilaginous head - how much higher and lateral it is than its normal position.
In the presence of congenital dislocation of the hip, an oblique position of the upper edge of the acetabulum is noted, and the upper end of the femur, including the cartilaginous head of the femur, which is supposed but not yet visible on the radiograph, is located more outward, but in some cases (even if the child is not yet standing) higher than on the healthy side. Naturally, with bilateral dislocation, X-ray diagnosis can be difficult due to the inability to make a comparison with a healthy joint.
In these cases, special schemes proposed by Ombredan, Hilgenreiner, Erlacher, Putti, S.A. are used. Reinberg and others. Such diagrams, using certain lines, establish the normal arrangement of the elements of the hip joint and, accordingly, make it possible to determine the displacement of the femur in relation to the acetabulum and determine the degree of this displacement. Early radiographic symptoms of congenital hip dislocation were first identified by the eminent Bolognese orthopedist Putti. In 1927 he proposed the classic "Putti triad":
1) increased bevel of the roof of the acetabulum;
2) displacement of the proximal end of the femur outward and upward relative to the acetabulum;
3) late appearance and hypoplasia of the ossification nucleus.
These symptoms were later supplemented by other researchers. Putti's scheme for reading radiographs is of well-known interest.
Since the ossification nucleus of the femoral head appears normally at 4-6 months of age, and in case of dysplasia - later, by 9-10 months, then in children of the first months of life, when the head, in addition, is only lateral, but not above the cavity , it is advisable to use the Hilgenreiner scheme to evaluate the radiograph. A horizontal line is drawn through both Y-shaped cartilages (Keller's line); From the highest point of the femoral diaphysis, a perpendicular h is drawn until it intersects with the horizontal line. The distance from the base of the Y-shaped cartilage to the perpendicular h is called the d value. The length of the horizontal segment d is normally equal to 1.2-1.5 cm, as well as the length of the perpendicular h. With dislocation, the value of h decreases, ad increases. From the bottom of the acetabulum, a line is drawn tangent to the most peripheral part of the roof of the acetabulum; the resulting angle (index) is normally 27-30° in a newborn and approaches 20° in a 2-year-old child. In the presence of joint dysplasia and delayed development of the acetabulum, the index increases.
Hip dysplasia is characterized not so much by an absolute increase in this angle, but by the presence of a difference in the angles on both sides, clearly indicating a malformation of the pelvis.
The scheme proposed by S.A. Reinberg, used in older children. Three vertical lines are drawn: along the midline of the body, through the superolateral edge (roof protrusion) of the healthy acetabulum and at an equal distance from the midline on the side of the dislocation. Normally, the vertical line passes through the diaphysis of the femur, and in case of dislocation, it passes more medially. A horizontal line is also drawn through the Y-shaped cartilages. Normally, the femoral head is located medial to the vertical and below the horizontal line; in case of dislocation, it is located laterally and above these lines. In children in the second half of life, attention is paid to the Shenton line. Normally, the lower contour of the femoral neck passes into the upper semicircle of the obturator foramen, but with dislocation, the arcuate line is absent, since a ledge appears due to the higher location of the lower contour of the femoral neck.
The most widely used is the Ombredant scheme, which takes into account the position of the head in relation to the horizontal line (Keller line) and the location of the femoral diaphysis (Ombredant line) in relation to the vertical line.
Thus, certain skills make it possible to give a clinical and radiological assessment of the condition of the hip joints in children in the first weeks of life.
Diagnosis and clinic of congenital hip dislocation in children older than one year
When a child begins to stand and walk, diagnosing congenital hip dislocation is less difficult.
In children after one year, one of the first symptoms that makes one think about the presence of a congenital dislocation of the hip is a late onset of walking, although this is not an absolute symptom, but is more common in the presence of bilateral dislocation, when children take their first steps at 14-15 months. The gait is characteristic: there is either some kind of instability or lameness when walking in the case of a unilateral dislocation, or a waddling, duck-like gait in the case of a bilateral dislocation. However, patients do not experience pain - the child remains cheerful and spends the whole day on his feet. Children of this age retain some of the symptoms that are important for early diagnosis, only they manifest themselves more clearly. The limb where there is a dislocation is in a position of external rotation, which is also visible during sleep. There is a relative shortening of the limb on the side of the dislocation in the absence of absolute shortening.
The relative length of the limb is measured from the anterior superior iliac spine to the medial malleolus, the absolute length is measured from the greater trochanter. The tip of the greater trochanter is located above the Roser-Nelaton line, which connects the anterior superior iliac spine to the ischial tuberosity. On the side of the dislocation, abduction of the hip is also limited, but rotational movements in the hip joint are possible to a greater extent than normal (Chassignac's symptom).
An important classic sign of a mature dislocation is a positive Trendelenburg sign. Normally, when you lean on your healthy leg, the buttock on the other side rises; in the case of congenital dislocation, when supporting the dislocated leg, the buttock of the other side drops (regardless of whether there is a dislocation on this side or not).
Trendelenburg's symptom is a reflection of the condition of the gluteal muscles of the limb on the side on which the child is standing. With normal tone of these muscles, they tense and to create balance when standing on one leg, the opposite half of the pelvis rises (a negative symptom of an elevated buttock). When standing on a leg with a congenital dislocation of the hip, as in the first case, the torso also tilts to maintain balance in the same direction, but the gluteal muscles are not able to bring their attachment points closer together (the greater trochanter - the crest and wing of the ilium), the opposite half of the pelvis sinks under the weight of the body (a positive symptom of a drooping buttock). Thus, a positive Trendelenburg sign is a sign not only of congenital hip dislocation, but also of any pathology associated with weakened tone of the gluteal muscles on the standing side. Their tone is reduced with paresis or paralysis of the muscles (consequences of poliomyelitis), with the points of attachment of these muscles approaching each other (acquired dislocations and varus deformity of the femoral neck with a high position of the greater trochanter).
When the child is positioned on his back with his legs extended, it is easy to determine Dupuytren's symptom - when pressure is applied to the heel area, the mobility of the leg along the axis and its upward displacement are determined.
One of the clinical prognostic symptoms in children over 1 year of age is the symptom of hip reduction. In a horizontal position, lying on his back, the patient is pulled with one hand by the lower third of the thigh, the pelvis is fixed with the other hand and the descent of the greater trochanter is observed. This symptom makes it possible to judge the degree of fixation of the head and joint capsule in children who have not been treated for several years and have been loading a dislocated leg, and to decide on the choice of treatment method.
With a unilateral dislocation, the normal femoral head, being in the socket, is palpable at the level of the pulsation of the femoral artery, but on the sore side the head in this place is not palpable.
The final diagnosis in children over 1 year of age is made on the basis of radiographs of the hip joints. The image not only confirms the diagnosis, but also allows you to more accurately judge the degree of dislocation and the prognosis of treatment, as it gives an idea of the changes that have occurred in the head, neck, cavity and its roof.
The radiography method for this disease has not only diagnostic, but also prognostic significance. In children 2-3 years old, when the question of choosing an open or closed method of reduction is being decided, it is advisable to take a photo while standing, lying down, and also when pulling the hip down with countertraction. With a deliberately chosen surgical method of treatment, these images make it possible to understand the choice of the surgical method and the types of techniques (for example, with pelvic osteotomy, you can decide which is more appropriate: the Hiari, Salter or Degas operation; when performing hip resection, you can clarify the size, level and shape of the resected section of bone etc.). Radiographs taken simultaneously in the midposition and in internal rotation are better than other methods in determining the presence of antetorsion and the degree of anteversion - anterior rotation of the neck.
It is important to note that in children older than one year and especially in adolescents, there is a pronounced deformity of the femoral neck with anterior rotation - anteversion, therefore, on direct radiographs of the joint in the middle position of the lower extremities, when in the supine position the patella is facing upward, the femoral neck has a false appearance in the shadow of the radiograph valgus form. An image in internal rotation usually reveals a well-defined, sometimes elongated femoral neck with a normal neck-diaphyseal angle. In this position, the head approaches the cavity and from its strictly profile picture one can see defects that are not visible on a direct radiograph - its true size, flattening, depressions on the head in the middle as a result of cartilage degeneration (often bicornuate form) due to unsuccessful attempts at reduction.
The atrography of the joint undertaken by some authors with oxygen or contrast liquids has only scientific significance, as it confirms morphological changes in the stretched bursa and joint cavity.
Differential diagnosis
Congenital dislocation of the hip in infants should be differentiated only from congenital shortening of the hip or some other rare developmental anomaly (complete underdevelopment of the proximal end of the femur), as well as from physiological or spastic muscle hypertension, which disappears or is overcome after a certain period of muscle tension.
Differential diagnosis in children over one year of age is carried out with all diseases accompanied by Trendelenburg's symptom, duck-like gait or limping gait. Among these diseases, two groups can be distinguished: 1) diseases that also cause dislocation syndrome (pathological dislocations of the hip after infantile paralysis, osteomyelitis and trauma), 2) diseases accompanied by varus deformity of the femoral neck (rickets, chondrodystrophy, deformity after Perthes disease, congenital varus cervical deformity, osteomyelitis and tumors of the femoral neck, chondrodysplasia and epiphysiolysis of the femoral head of various etiologies).
Paralytic dislocation of the hip after poliomyelitis is accompanied by a characteristic history, atrophy of the gluteal and femoral muscles, and on the radiograph is distinguished by osteoporotic bones without flattening of the acetabulum. Pathological dislocation of the hip after epiphyseal osteomyelitis is observed only in infants due to the accumulation of pus, and more often reactive fluid in the hip joint. A history of high septic temperature, the presence of fistula scars, and possible destructive changes in the head are characteristic of this disease. Diagnosis of rickets in cases of bilateral congenital dislocation of the hip is most common, since rickets also causes a duck's gait in cases of developing bilateral varus deformity of the femoral neck with a positive Trendelenburg sign, limited abduction of the hips and the location of the greater trochanter above the Roser-Nelaton line. The only clinical symptom indicating the absence of dislocation is the presence of the femoral heads at the level of the pulsation of the femoral artery and, of course, the presence of other signs of rickets. X-ray examination clarifies the diagnosis.
Source of information: https://www.orthoped.ru
The article was published on the website https://www.medafarm.ru
What to do if your child is diagnosed with congenital hip dislocation
Treatment of congenital hip dislocation is based on methods that allow the head of the bone and the acetabulum to form and take an anatomically correct position. To do this, it is necessary to hold the legs for a long time in an open position, but not fix them rigidly, and do not deprive the child of the opportunity to move. Under no circumstances should you tightly swaddle a baby with his legs together and straightened. On the contrary, it is recommended to use disposable diapers and wide swaddling (helps with mild forms of joint dysplasia), soft orthopedic devices (special pillows, splints, elastic stirrups).
The orthopedist also prescribes massage and exercise therapy for the baby. These procedures help strengthen muscles, stabilize the joint apparatus, and after removing the dilating leg of the orthopedic structure, restore full range of motion and accelerate the child’s physical development.
If congenital hip dislocation is diagnosed too late, at the age of 2-5 years, then a rigid plaster cast is used for treatment. Reduction of a dislocation with this treatment brings much more inconvenience and psychological discomfort to the child and parents (the child is in a cast for up to 6 months), but it is possible to do without surgery.
In the most complex and advanced cases, congenital dislocation is treated only with surgical methods (corrective osteotomy of the pelvic bones with derotation of the deformity).
If congenital hip dislocation is diagnosed and treated in a child under 1 year of age (maximum 2 years), then it is almost always possible to stabilize the joint using gentle non-surgical methods. All elements of the joint, although with a slight delay, are correctly formed. Therefore, the main thing is to pay attention to the developmental defect, not to miss this severe orthopedic pathology, to start treatment as early as possible and complete it to the end, in no case to interrupt it without permission.
How does hip dysplasia manifest - symptoms and signs
Parents of an infant are able to themselves suspect the presence of hip dysplasia. Typical signs:
- shortening of the thigh;
- restrictions in hip abduction (in the supine position, the child’s legs, bent at the knee and hip joints, are moved apart, if an angle of less than 160° is formed between them, the likelihood of dysplasia is very high);
- “click” symptom (scientifically called the Marx-Ortolani symptom) - when you slowly open your bent legs, you may hear a click on the affected side. At the same time, the affected leg twitches a little.
- asymmetry of the skin inguinal, gluteal and popliteal folds - asymmetry is most pronounced in children older than 2 months.
Asymmetry of skin folds may be absent with bilateral lesions.