Congenital syphilis is one of the manifestations or clinical forms of syphilis.
A child becomes infected with Treponema pallidum during intrauterine development.
This form manifests itself from the prenatal period of the child’s development to the age of 12-18 years.
Congenital syphilis is extremely dangerous.
It can affect almost all connective tissues, the musculoskeletal system, the skin of epithelial tissues, mucous membranes, and tissues of internal organs.
It is especially dangerous when the damage spreads to the central nervous system (CNS).
Neurosyphilis can be fatal.
At the first sign of suspicion of congenital syphilis, various studies are carried out, the most common of which are:
- Examination of spinal fluid (CSF)
- Searching directly for pathogen cells in the blood
- PCR research
- Various serological studies
When treating congenital syphilis, various sets of measures are used.
Drug therapy includes the prescription of bismuth preparations, as well as medications aimed at strengthening and enhancing immunity.
Currently, there are two types of congenital syphilis:
- 1.Late congenital syphilis
- 2.Early congenital syphilis
Late manifestation of congenital syphilis
Occurs in children aged two years and older.
This type of congenital syphilis is most clearly observed in adolescents aged 12-15 years and is somewhat reminiscent of the clinical picture of the type of tertiary syphilis.
In children aged two or five years, the so-called secretive congenital syphilis occurs in a latent form.
Typically, late syphilis develops when early manifestations are not treated properly.
Or it was asymptomatic, i.e. secretly and therefore no appropriate treatment was prescribed.
If we talk about the clinical manifestations of late congenital syphilis, they have a number of specific symptoms:
- Reliable data accurately indicating the presence of late congenital syphilis
- Probable data that is 70% likely to indicate the presence of congenital syphilis in children. Complex signs, or clinical manifestations of other infectious diseases, similar to the symptoms of congenital syphilis, especially in children. They are not accurate indicators of the presence of syphilis, and only indicate confirmation of the disease.
- Dystrophic changes or stigmas.
Now let's talk about these clinical symptoms of congenital late syphilis in more detail.
Let us give an example of which of these manifestations are more accurate and which are not, and which of them carry more reliable information.
Characterized by dystrophic features of the teeth, hearing loss or so-called labyrinthine deafness, parenchymal keratitis.
Also, these data may include so-called tetrad diseases or specific gonitis, triad of congenital syphilis.
Dystrophies (stigmas)
The occurrence of a number of dystrophies in congenital syphilis is not associated with exposure to Treponema pallidum (the causative agent of syphilis) and does not have any diagnostic value. They develop with many infectious diseases and intoxications, for example, with parental alcoholism. Stigmas can indicate that a child may be affected by syphilis and help in making a diagnosis.
Rice. 16. Enlarged and protruding frontal and parietal tubercles without a dividing groove (“Olympic forehead”). The anomaly occurs in 36% of patients.
Rice. 17. A high hard palate (“lancet” or “Gothic”) occurs in 7% of cases.
Rice. 18. Diastema (distance, gap) between the central incisors. Most often found on the upper jaw.
Rice. 19. A thickened sternal end (usually the right) of the clavicle (Ausitidian-Igumenakis symptom) occurs in patients with congenital syphilis in 25% of cases. The cause of the pathology is hyperostosis. In 13 - 20% of cases with congenital syphilis, there is an absence of the xiphoid process (Queir's axiphodia).
Rice. 20. A shortened (infantile) little finger (Dubois symptom) is recorded in 12% of cases with congenital syphilis. The little finger may be curved and turned towards the other fingers (Hissar's symptom).
Rice. 21. Stigmas indicating congenital syphilis may include spider fingers—abnormally long and narrow fingers (arachnodactyly).
Rice. 22. Girls and boys with congenital syphilis may experience hypertrichosis - growth of hair on the forehead (Tarkovsky hypertrichosis).
Possible signs of late congenital syphilis
Some of the most striking manifestations of late congenital syphilis are pathology of dental development, labyrinthine deafness and the manifestation of parenchymal keratitis.
These late manifestations of syphilis were first described by the famous surgeon, dermatologist, and ophthalmologist Jonathan Getchinson and A. Fournier.
The latter proposed calling such manifestations Hutchinson's triads.
He himself discovered the manifestations of late congenital syphilis, the symptom of tabes dorsalis.
Anomalies in congenital syphilis that appear directly on the teeth are described by scientists J. Getchinson, A. Fournier and Pfluger.
In their opinion, Treponema pallidum attacks the rudiments of teeth even during intrauterine development, thereby forming their further pathology in the future.
Each of their discoveries is fundamental:
- D. Getchinson described a special form of pathology of teeth, incisors, which are characterized by a moon-shaped notch. Although at that time two symptoms were needed to confirm his theory: parenchymal keratitis and labyrinthine deafness.
- Another scientist who studied this pathology, Pfluger, described that with the late development of congenital syphilis, damage to large molars or molars is characteristic. With this form of pathology, the tooth takes on a kidney-shaped appearance and significant underdevelopment of the tubercles (Carabelli tubercle) occurs.
Probable findings include changes in the structure of the skull (buttock-shaped skull), scars around the mouth (Robinson-Fournier), changes in the structure of the teeth, syphilitic chorioretinitis, damage to the central nervous system.
Changes in the structure of the legs are characteristic, namely the shins take on a saber-shaped appearance, becoming similar to a saber.
To recognize the likely signs of late congenital syphilis, the doctor must have extensive knowledge in this area.
After all, the symptoms of congenital syphilis are similar to the manifestations of other infectious diseases in their early development, but they do have some features, which will be discussed now.
EARLY CONGENITAL SYPHILIS: CLINIC, PATHOMORPHOLOGY, DIAGNOSIS, TREATMENT, PREVENTION
In connection with the increasing incidence of congenital syphilis in Russia, issues of its diagnosis, treatment and prevention are being discussed. Many forgotten pathomorphological data are presented. The article includes descriptions of problematic cases observed by the authors.
Due to the fact that there is an increase in the incidence of congenital syphilis in Russia, the paper discusses its diagnosis, treatment, and prevention. Many forgotten pathomorphological data are given. The paper includes accounts of the difficult cases observed by the authors.
K.K.
Borisenko - Dr. honey. Sciences, Professor, Head. Department of Syphilidology of the Central Research Dermatovenerological Institute, Moscow. OK. Loseva - Doctor of Medicine. Sciences, senior researcher of the same department, the same institute. O.V. Share - Candidate of Medical Sciences Sciences, researcher at the same department, at the same institute. E.L. Tumanova - Candidate of Medical Sciences Sciences, Associate Professor, Department of Pathological Anatomy, Faculty of Pediatrics, Russian State Medical University, Moscow. KK Borisenko - prof., MD, Head, Department of Syphilisology, Central Research Dermatovenereological Institute, Moscow OK Loseva - MD, Senior Researcher, the same Department, the same Institute OV Dolya - Candidate of Medical Sciences, Researcher, the same Department, the same Institute Ye.L.
Tumanova — Candidate of Medical Sciences, Associate Professor, Department of Pathological Anatomy, Pediatric Faculty, Russian State Medical University, Moscow В
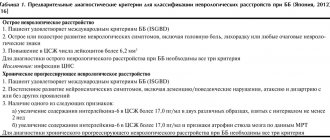
Surveys on the diagnosis, treatment and prevention of congenital syphilis have now acquired particular relevance. Since 1990, the incidence of syphilis in the adult population has gradually increased, and in the last two years its growth has become epidemic. This could not but be followed by an increase in the incidence of congenital syphilis. According to the statistics department of the Ministry of Health of the Russian Federation, in 1992, 31 cases of congenital syphilis were registered in Russia, in 1993 - 46, in 1994 - 118, in 1995 - 221, in 1996 - 469, in 1997 - 714. Today there are three main problems associated with congenital syphilis: prevention, diagnosis and optimization of treatment methods. The basic principles for the prevention of congenital syphilis were proposed in our country back in the 20s by M.G. Mgebrov, G.I. Meshchersky, M.M. Reitz. In subsequent years they underwent changes and additions. Currently, scientifically based comprehensive measures are being carried out for antenatal and postnatal prevention of congenital syphilis. Antenatal prevention consists primarily of timely detection of the disease in a pregnant woman and its adequate treatment. The mandatory three-time serological examination of pregnant women adopted in our country - in the first and second half of pregnancy, as well as upon admission to the maternity hospital - is fully justified. Serological examination of pregnant women in the first and third trimesters of pregnancy is also recognized abroad as necessary [1].
| Gonorrhea. Typical purulent discharge from the urethra | Gonococcal proctitis (photo through a proctoscope) | Gonorrhea. Purulent discharge characteristic of gonococcal cervicitis. |
| Non-gonococcal urethritis. The discharge is more watery than with gonorrhea. | Trichomoniasis vulvovaginitis. | |
| Primary syphilis. Solid tanker. | ||
| Congenital syphilis. Hutchinson's teeth. | Congenital syphilis. Saddle nose. | |
However, at present, these measures are not carried out in some pregnant women due to a number of reasons: instability of social, economic and interpersonal relationships; a sharp increase in migration processes; growth of semi-legal prostitution; early onset of sexual activity, etc. [2]. All this leads to the fact that some pregnant women are not registered with the antenatal clinic and are not examined before birth. That is why children with congenital syphilis are more often born to young mothers, women leading an asocial lifestyle, planning to abandon the child and therefore not registered with the antenatal clinic.
Rice. 1. Classic “senile” appearance of a newborn; malnutrition, hydrocephalus.
Features of the clinical picture
, as well as the influence of syphilitic infection on the course and outcome of pregnancy, a significant number of studies conducted in our country, mainly in the 30–50s, are devoted. It is known that syphilitic infection has a toxic effect on the fetus, being a common cause of miscarriages, premature births, and stillbirths. Syphilis is characterized by late miscarriages and stillbirths in the 6–7th month of pregnancy. Miscarriages at earlier stages are less common, which is confirmed by numerous statistical data from both domestic and foreign authors [3–5]. It is believed that up to 89% of children born to mothers with untreated or inadequately treated syphilis die in utero or shortly after birth [6].
Rice. 2. Syphilitic pemphigus.
It is noted that currently the course and outcome of pregnancy with syphilis are characterized by the predominance of latent forms of the disease, a significant reduction in the frequency of late miscarriages, premature births and stillbirths [7]. Regarding pregnancy outcomes with seroresistance, literature data are contradictory. In women with a persistently positive Wasserman reaction who have received full treatment, there is still a significant number of spontaneous abortions, stillbirths, premature births, and there are also cases of congenital syphilis [8]. Other authors, having monitored pregnancy outcomes in women with persistently positive CSR and examined their children, came to the conclusion that such women can be guaranteed the birth of healthy offspring if they received antisyphilitic treatment during pregnancy [9].
Rice. 3. Massive fibrosis at the porta hepatis, inflammatory infiltrates of plasma cells and lymphocytes. Hematoxylin and eosin staining. Uv. 250.
Rice. 4. Kidney vessel. Fibrinoid necrosis of the vessel wall. Diffuse plasmatic infiltration. Hematoxylin and eosin staining. Uv. 160.
Rice. 5. Diffuse infiltration of the soft meninges by plasma cells. Severe vascular congestion. Hematoxylin and eosin staining. Uv. 63.
Rice. 6. Thymus gland. In the lobules there is no division into the cortical and medulla layers. Proliferation of interlobular connective tissue with diffuse plasmatic infiltrates. Hematoxylin and eosin staining. Uv. 63.
Rice. 7. Pancreas. Diffuse proliferation of connective tissue that walls up the islets of Langerhans. Hematoxylin and eosin staining. Uv. 160.
Rice. 8. Small intestine. Flattening of the villi. In the submucosa and villi there are infiltrates consisting of plasma cells and histiocytes. Hematoxylin and eosin staining. Uv. 160.
Rice. 9. Large intestine. No lint. In the submucosa and villi there are infiltrates consisting of plasma cells and histiocytes. Hematoxylin and eosin staining. Uv. 160.
It is generally accepted that the only way of infection with congenital syphilis is transmission of infection to the fetus by a mother with syphilis through the placenta [10]. It is known that Treponema pallidum does not penetrate the placenta and does not infect the fetus until the 4th month of pregnancy [3]. It is believed that before 16 weeks the fetus is not mature enough to react to the antigen by producing antibodies [11]. The pathogenesis of congenital syphilis depends largely on the immune response of the fetus and, to a lesser extent, on the cytodestructive effect of Treponema pallidum. That is why adequate treatment of syphilis in the mother before 16–19 weeks of pregnancy usually prevents damage to the fetus. For specific treatment
pregnant women are currently using penicillin preparations of varying degrees of duration in accordance with current instructions for the treatment and prevention of syphilis.
However, as can be seen from the example below, treatment, in particular with benzathine-penicillin preparations, carried out in the second half of pregnancy, may not provide the prevention of congenital syphilis. Patient P., 37 years old, was admitted for delivery on May 13, 1996. For latent early seropositive syphilis, from January 29, 1996 (at 25–26 weeks of pregnancy) she received specific and preventive treatment with benzathine penicillin at a dose of 2.4 million ED intramuscularly once a week, 6 injections in total. KSR dated January 29, 1996, 3+ 4 +3+, KSR dated April 2, 1996, neg. 2+ neg. On May 14, 1996, she gave birth to a boy weighing 3,040 g, height 52 cm. The general condition of the child after childbirth was moderate: chin tremor, muscular dystonia, tendency toward muscle hypertonia, liver enlarged by 1.5 cm, spleen at the edge of the costal arch, skin and visible mucous membranes are free from specific rashes.
The child was prescribed preventive treatment for early congenital syphilis. On the 1st day after the start of therapy, an exacerbation reaction was observed: temperature 37.9°C, papular rashes on the skin of the anterior abdominal wall, buttocks and extremities, and copious mucous discharge from the nasal passages. CSR dated May 14, 1996, 1+2+1+, against the background of ongoing therapy, these manifestations of the disease resolved on the 4th – 5th day. Diagnosis: early congenital manifest syphilis. The described case is not the only one in our practice. We recommend using durant penicillin preparations for the specific treatment of pregnant women only until the 18th week of pregnancy. After this period, specific and preventive treatment should be carried out with soluble penicillin or penicillin preparations of medium duration (procaine salt of penicillin, procaine penicillin), which penetrate the placenta in a higher concentration. In difficult conditions of increasing incidence, the role of early clinical and laboratory diagnosis of syphilis increases [12]. Recognition of congenital syphilis in the presence of pronounced clinical manifestations does not present any particular difficulties. Early congenital syphilis, according to the international classification, is usually called an intrauterine infection that manifests itself in a child under 2 years of age.
Features of the clinical picture make it possible to distinguish congenital syphilis in infancy - up to one year [10].
It most often appears in the first 2 months of life and is characterized by a number of typical symptoms. In “classical” cases, a newborn (often premature) has a peculiar “senile appearance”, primarily due to severe malnutrition (Fig. 1). The skin is wrinkled, flabby, dirty yellow. The head is enlarged, with a noticeably pronounced subcutaneous venous network, the skin is often covered with seborrheic scales. Children gain weight very slowly, develop poorly, and often cannot suck. They are restless, anxious, sleep poorly, cry almost constantly, and sometimes emit a sharp, piercing cry (Sisto's symptom). A similar condition in children with congenital syphilis is quite rare these days. However, with manifest forms of early congenital syphilis, a number of other characteristic signs are revealed. Skin changes
in children in the first months of life are characterized by unusual forms that are not found in acquired syphilis.
The earliest of them is syphilitic pemphigus (Fig. 2), which can be detected at birth or appear in the first days of life. Blisters with serous-purulent, sometimes bloody contents are most often localized on the palms and soles, and occasionally on other areas of the skin. At the base of the blisters there is a specific infiltrate, so the blisters are surrounded by a reddish-purple rim. They quickly burst, revealing an erosive surface surrounded by fragments of the epidermis. The second “special” symptom is diffuse infiltration of the skin, which most often occurs by the end of the 2nd month of life. It is preceded by diffuse erythema of the affected areas. Infiltration also appears primarily on the palms and soles; in addition, the face (often around the mouth), scalp, buttocks, thighs, and skin on the elbows and knees are also affected. The changed skin is thickened, its surface is shiny, and deep cracks easily form, especially around the mouth. In addition to the described skin changes for early congenital syphilis, specific rhinitis
is pathognomonic, which is detected already at birth: first there is a significant swelling of the mucous membrane, making breathing difficult, then a discharge from the nose appears - mucous, purulent and, finally, bloody, later profuse purulent-bloody fetid discharge is observed from the nose, nosebleeds.
Rhinitis is accompanied by deep ulcerations of the mucous membrane, damage to cartilage and bones. Wegener's osteochondritis
is quite specific - a lesion of long tubular bones at the border of the epiphysis and diaphysis - which is caused by impaired calcium formation and inhibition of the development of osteoblasts.
The second and third stages of osteochondritis (Parro's pseudoparalysis) occur only with congenital syphilis and are diagnosed by radiography of the tubular bones of the forearm and lower leg. In addition to the listed symptoms, other manifestations of the disease may be observed - from the skin (roseolous, papular rash), the central nervous system (convulsions, causeless screaming, meningeal symptoms, hydrocephalus), the organ of vision (chorioretinitis, lesions of the optic nerve), internal organs (hepatosplenomegaly ). Pathomorphological changes in congenital syphilis
are quite typical, but the rarity of such cases in the last 30 years has led to the fact that a qualified pathologist’s conclusion in the event of a child’s death cannot be obtained everywhere.
This makes it urgent to improve the professional level of pathologists and conduct training for specialists in this profile. Taking these circumstances into account, we dwell in some detail on the pathomorphological changes in congenital syphilis. Pathomorphological changes in the skin are manifested by damage to capillaries and small vessels in the form of productive endarteritis and phlebitis. In the early stages of the process, intimal cell proliferation occurs in the vessels, which often leads to narrowing and obliteration of the vessel lumen. At the same time, infiltrative changes in the walls of blood vessels occur, when the membrane itself and perivascular tissue are infiltrated with lymphoid and plasma cells, eosinophils. Such infiltrates are often localized around the sweat glands. In the skin itself, its papillary layer, significantly pronounced swelling, hyperemia, and infiltration of the above cells are found. The skin of the palms and soles is especially characterized by diffuse infiltration of plasmatic and lymphoid cells. Giant cells are rare. Syphilitic rhinitis is based on diffuse infiltration of the anterior part of the nasal mucosa with round cell elements and leukocytes. The process is accompanied by hyperplasia of the mucous membrane and subsequently spreads to cartilage and nasal bones, which leads to deformation of the osteochondral skeleton. Damage to internal organs in congenital syphilis is characterized by an infiltrative-productive process, and occasionally by the presence of gummous formations. According to various authors, syphilitic changes in 100% of cases are found in the liver and spleen, in 94% in the vessels, in 85% in the adrenal glands, the pancreas, kidneys, and bones are very often affected. Changes in the liver
are associated with the fact that the spirochete enters the fetal body through the umbilical vein.
Macroscopically, the liver is enlarged, very dense, yellow-brown or whitish-brown in color - the so-called “flint liver”. Histological changes in the liver are divided into three types. In the first, cellular infiltration of the capsule and periportal connective tissue, the walls of the hepatic veins and bile ducts is determined. The infiltrate consists of histiocytes, plasma and lymphoid cells, eosinophilic leukocytes. There is a slight proliferation of Kupffer cells. The second type of changes includes thickening and infiltration of the Glissonian capsule, proliferation of connective tissue in the lobules, and expansion of the portal tracts. Infiltration of periportal connective tissue is weak. The infiltrative process is sometimes concentrated around the bile ducts, where rings of proliferating connective tissue (syphilitic pericholangitis) and branches of the portal vein are formed (syphilitic periphlebitis; Fig. 3). In rare cases, the liver is reduced in size, dense, with a fine-grained surface. Microscopically, signs of portal cirrhosis are revealed. The connective tissue is infiltrated by lymphoid cells with an admixture of plasma cells, histiocytes and eosinophils. The third type of changes includes cases with the presence of miliary gummas (5% of sectional material). Macroscopically, gummas are defined as grayish dots. Microscopically, small foci of necrosis are detected, as well as diffuse inflammatory infiltrates in the growing connective tissue [13]. to the pancreas
is characterized by a sharp proliferation of intercellular tissue, which penetrates between the acini, ducts and islets.
The gland pattern may be completely erased. Due to the growth of connective tissue, the consistency of the gland sometimes reaches almost cartilaginous density [14]. The spleen
in early congenital syphilis is dense, its weight increases 10 times or more.
Fibrinous deposits on the capsule are often detected (syphilitic perisplenitis). Macroscopically, the thickening of the capsule is determined with the imposition of fibrin on it, sometimes the capsule is hyalinized. Usually the spleen is depleted of cellular elements, sometimes the light centers are sharply hyperplastic. Intrafollicular arteries and larger vessels are thickened with symptoms of productive endarteritis and obliteration of the lumen. The next place in frequency is vascular lesions.
Histological changes are represented by obliterating endarteritis.
These changes are the cause of ischemic necrosis. In the venous vessels there is infiltration of the wall with lymphoid elements with an admixture of plasma cells, neutrophils, and eosinophils (Fig. 4). Often the veins have a thickened adventitia. The vessels of the liver, myocardium, spleen, and kidneys are affected [13]. the kidneys
are also often affected .
The lesion is inflammatory in nature. Focal or diffuse interstitial nephritis occurs. Small round cell infiltration around the glomeruli and vessels and the proliferation of interstitial connective tissue with similar infiltration are specific [13]. Bone damage
in the form of syphilitic osteochondritis is considered one of the permanent manifestations of congenital syphilis.
However, many authors indicate that the presence and severity of Wegener's osteochondritis is variable. Macroscopically, there are 3 degrees of severity of the process. I degree - an uneven, winding strip of gray-yellow color with a reddish tint, 1 - 2 mm wide; II degree – the strip width increases to 5 mm; III degree – the diaphysis is separated from the epiphysis. Osteochondritis is observed in flat bones and phalanges, but more often in tubular bones. With treatment, osteochondritis quickly disappears and does not affect further bone growth. In recent years, grade III osteochondritis has practically never occurred [15]. Syphilitic periostitis can occur as an independent lesion of the periosteum or in combination with osteochondritis. The lungs
are rarely affected.
There is syphilitic, so-called white, Virchow's pneumonia. The process involves a lobe, sometimes the entire lung. Macroscopically, the lung is dense, airless, light gray in color. Microscopically, thickening of the interalveolar septa, peribronchial, and perivascular tissue, which are infiltrated with lymphoid, plasma, and epithelioid cells, is observed. In the lumen of the alveoli there is exudate consisting of neutrophils and alveolar macrophages. In the vessels, growth of the intima and narrowing of the lumen are noted. Damage to the central nervous system
in children with congenital syphilis is characterized by internal hydrocephalus and chronic syphilitic leptomeningitis.
With leptomeningitis, thickening of the soft meninges is observed, mainly at the base of the brain, extending to the cerebral hemispheres. Histological examination of the pia mater reveals infiltration of lymphoid, histiocytic, plasma cells, and fibroblasts (Fig. 5). In the walls of the vessels of the membranes, the same infiltration is observed, the lumen of the vessels is narrowed to the point of obliteration. The inflammatory process along the vessels spreads to the substance of the brain. Pathomorphological changes in syphilitic encephalitis are manifested by sclerosis of blood vessels with infiltration of their walls by plasma and lymphoid cells, proliferation of glia, formation of glial nodules, and perivascular infiltrates. Of the endocrine glands, the adrenal glands
.
Microscopically, capsule fibrosis is detected, the zona glomerulosa is destroyed in the cortex, and the zona fasciculata becomes fibrotic [16]. In the thymus gland,
there is a proliferation of interlobular connective tissue infiltrated with lymphohistoplasmocytes.
The lobules are small, they lack division into the cortical and medulla layers (Fig. 6). The number of lymphocytes is reduced in both layers. Hassall's corpuscles are small, some of them layered, located in both the cortical and medulla layers. Heart disease
with early congenital syphilis is very rare.
There is no convincing evidence of syphilitic intestinal lesions in infants [15]. Since congenital syphilis is transmitted to the fetus through the placental route, the placenta
is often involved in the pathological process. However, many authors indicate that with obvious syphilis in the mother and fetus, changes in the placenta may be absent. When the placenta is damaged, its weight increases 2–3 times. Macroscopically, the placenta is fleshy, with large lobules of grayish-yellow or pinkish color. Microscopically, villous hyperplasia is observed; villous sclerosis is often combined with vascular sclerosis and obliteration of their lumen. Thrombosis of the intervillous spaces, inflammatory infiltrates from round cell elements and leukocytes in the membranes are not specific to congenital syphilis. Treponemas are found very rarely in the placenta. It should be noted that the examination and visual assessment of the placenta is usually not given due attention, while the description of the placenta in congenital syphilis has diagnostic value. In the context of a syphilis epidemic, obstetrician-gynecologists who deliver babies and do not yet know the results of a serological examination of the mother should more carefully examine and describe the placenta. This is important for both clinical and pathological diagnosis of congenital syphilis. We present two cases of early congenital syphilis that resulted in death.
One child (A) died during the intrapartum period, the second (B) lived for 90 hours. The mothers were 27 and 20 years old, respectively; they were practically not examined during pregnancy and were not registered with the antenatal clinic. Upon admission to the maternity hospital, they underwent a DCS study, and positive results were obtained after delivery. During pregnancy, one woman was diagnosed with colpitis and vaginal condylomatosis, for which she was treated with Tsiprolet. Child A. was born at the 32nd week of pregnancy, birth weight 2250 g. Child B. was born at the 29th week of pregnancy, birth weight 1270 g. In both cases, polyhydramnios was noted from 1.5 to 2.0 l , the waters are cloudy and light brown in color. Child B. had an Apgar score of 4/4 points at birth; from the 5th minute of life he was intubated and transferred to artificial ventilation. At birth, a mild roseola rash was noted on the chest and abdomen, which disappeared on the 2nd day of life. From the 3rd day of life, the child released a large amount of light yellow sputum through the endotracheal tube. Bradycardia developed. There was an admixture of greenery in the stool. A general blood test revealed anemia and leukocytosis with a shift to the left.
The pathological examination revealed the following changes. Macroscopic examination. The skin of both children was slightly jaundiced and acrocyanosis was pronounced. The ossification nucleus of the femur is absent in both. Child B. has a small amount of dark liquid blood in the umbilical vein, and in the Arancia duct there is a red thrombus of dense consistency attached to the wall of the vessel. In both children, examination of the brain revealed expansion of the posterior horns of the lateral ventricles, and the ependyma was smooth and shiny. In one child, a softening focus measuring 1.0 x 0.5 cm was found in the periventricular zone, in the occipital region. In both children, macroscopic changes were noted in the lungs. The lungs are dense, completely occupy the pleural cavities; sections reveal multiple small and merging foci of light gray color. When examining the heart, fibromyxomatous growths on the tricuspid valve leaflets were discovered in one child. In both children, the liver is dense, its mass is increased by 1.5 - 2 times; in one child, a gray lesion with a hemorrhagic rim was found in the left lobe. The mass of the spleen was increased 5–6 times; perisplenitis was observed in one child. The pancreas in both children is dense, especially in the head area. In one child, a Wegener's strip was detected in the femurs. Microscopic examination. In the liver, vacuolar degeneration of hepatocytes, cholestasis, inflammatory infiltrates consisting of histiocytes, plasma cells and lymphoid cells, which are located along the portal tracts, penetrating into the lobules. Fibrosis is pronounced, especially at the porta hepatis. The liver capsule is thickened due to sclerosis and inflammatory infiltration. In the pancreas there is a diffuse proliferation of connective tissue with the accumulation of infiltrates in it, consisting of plasma cells, histiocytes and lymphocytes (Fig. 7). The lungs in both cases are immature - the bronchi are located under the pleura. Interstitial pneumonia is expressed with thickening of the interalveolar septa due to their infiltration by lymphocytes and plasma cells. Perivascular and peribronchial focal plasmacytic infiltrates are noted. In the adrenal glands - fibrosis of the capsule, disappearance of the glomerular and fibrosis of the zona fasciculata. In the substance of the brain there are perivascular infiltrates of plasma cells and mononuclear cells, the walls of the vessels are sclerotic. Diffuse gliosis of the brain substance is pronounced. The soft meninges are sclerotic, and there are plasma-histiocytic infiltrates. In both cases, damage to the cardiovascular system is noted. Perivascular sclerosis, as well as histioplasmacytic infiltrates with an admixture of lymphocytes, are observed in the Arancia duct and the vessels of all internal organs. Interstitial myocarditis was detected in the heart. In both cases, the small and large intestines were affected: there was a sharp flattening of the villi, sclerosis of the vessels of the submucosal membrane with the accumulation of plasma-histiocytic infiltrates in it (Fig. 8, 9).
Thus, as a result of a morphological study, we identified some features of pathomorphological changes in various organs (damages of the intestine, pancreas, cardiovascular system, thymus), which are poorly described in the literature.
It should be noted that congenital syphilis is most severe in premature infants, as well as in children with early clinical manifestations (from the 1st week of life); There is a high mortality rate in this group. Diagnosis of congenital syphilis,
compatible with life, or occurring in a latent or asymptomatic form, has its own characteristics.
| Currently, congenital syphilis is usually diagnosed on the basis of positive serological reactions (KSR, RIF, RIT), the presence of skin manifestations, bone changes (osteochondritis, periostitis), initial changes in the choroid of the eye (chorioretinitis), rhinitis, enlarged liver and spleen, pathology cerebrospinal fluid. |
Diagnosis of early latent congenital syphilis is difficult during 3 months of life, when it is difficult to determine whether the disease occurs in the child or transplacental transfer of antibodies from the mother. In these cases, it is necessary to take into account the mother’s medical history (the stage of syphilis, which characterizes how long ago the child was infected; incomplete, late treatment of the mother or its absence); the degree of positivity of serological reactions in the child in comparison with the results in the mother (more pronounced positivity in the child indicates his illness); positivity of serological tests for IgM (domestic test systems of this series are still unreliable, imported ones are at the testing stage). It is necessary to emphasize the importance of timely dynamic examination of the child, starting from the 1st month of life, otherwise the diagnosis of latent congenital syphilis may be late. Let's give an example.
Patient V., 27 years old.
She was admitted with a child aged 6 months on 03/04/96 for a clinical and serological examination. For early latent seropositive syphilis, detected on May 5, 1994, the woman received specific treatment with retarpen at a dose of 2.4 million units intramuscularly once a week, a total of 4 injections. Before the onset of this pregnancy, there was a persistent tendency towards negative CSR (DSR from 06.94: 2+3+ e/m 4+; DSR from 12.94: + neg. e/m 2+) – this was not observed further. During pregnancy, she did not receive preventive treatment and was not registered with the antenatal clinic. Weakly positive DSR results remained (DSR dated 04.10.95: e/m 3+ during labor). On 10/04/95 she gave birth to a boy weighing 3.200 g, length 52 cm. During examination of the woman on 03/04/96, seroresistance was determined (KSR dated 03/04/96 neg. 2+ e/m 4+, RIF 4+/3+, RIT 70%) and additional treatment was prescribed. The child was not examined after birth. Upon admission to the hospital in a child: CSR dated 03/04/96 2+ 2+ e/m 3+, RIF abs 4+, RIT 65%.
Objectively: the skin of the torso, limbs, scalp, visible mucous membranes are free from specific rashes. The liver is at the edge of the costal arch, the spleen is not enlarged. For organs and systems without pathology. The general condition of the child is satisfactory. Based on the positivity of serological reactions and test results of the mother, the child was diagnosed with early latent seropositive syphilis. Specific treatment with penicillin was carried out at the rate of 100,000 units per 1 kg of body weight 6 times a day for 28 days. Diagnosis of early congenital syphilis can be difficult in the presence of nonspecific clinical symptoms (enlarged liver, spleen, postnatal encephalopathy), when it is necessary to differentiate latent and manifest congenital syphilis. In these cases, in addition to the above factors, the therapeutic effect of the specific treatment is also of diagnostic value. In such situations, a somewhat “delayed” diagnosis is possible, taking into account the dynamics of clinical and serological data. Serological diagnostic methods
congenital syphilis are represented by non-treponemal and treponemal tests.
Abroad, to diagnose early congenital syphilis, the following serological examination is carried out: • RPGA [17]; • VDRL [18]; • RIFabs. In children with positive VDRL, RPGA and RIFabs, a 19S – IgM – RIFabs test is performed to confirm the diagnosis and decide on the need for treatment [19]. Recently, enzyme-linked immunosorbent assay (ELISA) has become one of the most common methods in various fields of medicine.
One of the reasons for the widespread use of ELISA for diagnostic purposes is the possibility of test automation [8].
ELISA refers to treponemal specific tests and is designed to detect specific antibodies in the blood serum and cerebrospinal fluid of patients with syphilis, as well as to differentiate false-positive results obtained in standard serological tests for syphilis [20]. Theoretically, antibodies against IgM are detected in the serum of a newborn, provided that Treponema pallidum is present in his tissues [21, 22]. According to various authors, IgM antibodies are detected in the patient’s body within 2 weeks after infection. Since, due to their large molecular weight, these antibodies do not penetrate the normal placenta from mother to fetus, the formation of treponeme-specific IgM antibodies in the child’s blood indicates the presence of infection in the newborn [17]. Methods for specific and preventive treatment of children
are constantly being improved.
According to the current instructions for the treatment and prevention of syphilis, preventive treatment for children born to mothers with syphilis, poorly or insufficiently treated, is carried out with penicillin preparations for 2–4 weeks
Damage to the lower leg areas (saber shins)
The pathology typically manifests itself in the child’s infancy.
It accounts for 70% of all pathologies associated with late syphilitic manifestations.
A large proportion of the damage occurs in the periosteum and tibia - osteoperiostitis, osteochondritis (damage to the cartilage itself involving a small area of the bone itself),
Due to the weight of the child, the bones simply bend forward.
The child grows and learns to walk, his legs resemble a saber blade.
The bones become thicker and longer.
At the same time, the child begins to sleep restlessly, as he is bothered by night pain in his legs.
In this case, damage to the bones of the forearm is not observed.
To confirm this diagnosis, an x-ray examination is necessary.
In addition to the saber-shaped manifestation of syphilis, there is a similar symptom with Paget's disease or rickets, when the bones bend outward.
Syphilitic drives
Initially, the lesion occurs on one joint, and after some time the lesion occurs on the second.
There is usually no increase in temperature, and there is practically no pain.
Despite the fact that the joints significantly increase in volume, the skin over them does not change color and remains physiological in color.
But in the joints themselves, or rather in their cavities, a significant amount of fluid accumulates, which can sometimes be purulent in nature.
It is during this course of the disease that the Wasserman reaction (WRR) always gives a positive result.
Another manifestation of syphilis is a saddle nose.
Usually manifests itself in cases where syphilitic rhinitis has been suffered in the past.
There is a change in the structure of the nose itself, the nostrils begin to protrude forward when the nose itself sinks inside the skull.
Due to changes in its mucous membrane, the manifestation of the so-called goat and lorgnette nose is observed.
In the very first months of life, the so-called buttock-shaped skull can form.
When the flat bones of the skull itself are damaged, due to osteoperiostitis and periostitis, respectively, the frontal lobes, namely their right and left tubercles, begin to protrude forward.
At the same time, they are separated by a small groove, reminiscent of a child’s buttock (hence the name).
It is during this period of a child’s life that manifestations of mental retardation due to congenital syphilis begin.
This should not be confused with the disease hydrocephalus of newborns, in which the entire skull increases in size.
The share of these manifestations of late congenital syphilis in children is 20%.
Here, small scars appear on the chin, frontal area, around the lips, including the corners of the mouth.
If a child suffers pyoderma, candidiasis or a burn in this area in childhood, the scars remain forever and do not heal.
The cause of this manifestation of the disease is usually diffuse papular infiltration of Hochsinger.
Complex data include mainly dystrophies and stigmas.
Characteristic changes in the structure of the little fingers of the hands.
They become short and thick, with no xiphoid process.
Thickening occurs at the end of the clavicle and other pathologies change the structure of the body during late congenital syphilis.
In most cases, complex data do not include lesions that directly involve the Treponema pallidum itself.
This is mainly due to pathologies that arose due to gross violations by future parents during pregnancy or when conceiving a child (dystrophy).
For example, if parents are alcoholic or if a child is conceived while drunk.
This may also be due to various intoxications or any infectious diseases.
Possible signs of the disease
Possible signs of the disease require additional confirmation of the diagnosis from the doctor, as they can also occur in other diseases. When diagnosing, it is also necessary to take into account other specific manifestations of syphilis, anamnesis data and the results of an examination of the child’s family. Chorioretinitis, nasal deformities and buttock-shaped skull, dental dystrophies, radial scars on the chin and around the lips, saber shins and gonitis are the main probable signs of congenital syphilis.
Saber shins
This pathology develops in infancy and accounts for about 60% of all lesions in late congenital syphilis. The disease affects the periosteum and bone tissue of the tibia (osteoperiostitis), as well as the cartilage with the underlying portion of the bone (osteochondritis), which gradually bend under the weight of the child. The bend is formed at the front and resembles a saber blade. The bones themselves lengthen and thicken. The child is bothered by night pain. The bones of the forearm are somewhat less commonly affected. The diagnosis is confirmed by x-ray. A similar picture is observed in Paget's disease. With rickets, the bones bend outward.
Rice. 8. X-ray of saber-shaped shins (left) and ridge-shaped periostitis (right).
Rice. 9. In the photo there are saber-shaped shins of a child.
Syphilitic drives
Syphilitic drive was first described in 1886 by Cletton. Of all lesions in congenital syphilis, gonitis accounts for 9.5%. The disease affects the synovial membrane and bursa of the knees, and less commonly the elbow and ankle joints. Cartilage and bone epiphyses are not affected. The process is often bilateral, but first one joint becomes ill. Syphilitic drive occurs without fever, sharp pain and dysfunction. The joints increase in volume, the skin over them does not change color. Liquid accumulates in the cavities. The course is chronic. Resistance to specific therapy is noted. The Wasserman reaction always gives a positive result.
Rice. 10. Syphilitic drive is a probable sign of late congenital syphilis. In the photo on the left, protrusions of the inversions of the synovial membranes of the articular capsules of the knee joints are visible.
Saddle nose
Deformation of the nose with congenital syphilis is recorded in 15 - 20% of cases and is a consequence of syphilitic rhinitis suffered at an early age. The nose acquires a saddle shape as a result of the destruction of the nasal bones and nasal septum. The nose is sunken and the nostrils protrude. Small cell diffuse infiltration and atrophy of the nasal mucosa and cartilage lead to the formation of a goatee or lorgnette nose.
Rice. 11. Consequences of late congenital syphilis - saddle nose.
Buttock-shaped skull
The buttock-shaped skull is formed in the first months of a child’s life. Periostitis and osteoperiostitis of the flat bones of the skull leads to a change in its configuration - the frontal tuberosities stand forward, with a groove (buttock-shaped skull) located between them. With hydrocephalus, all sizes of the skull increase.
Rice. 12. The photo on the left shows enlarged frontal tuberosities, the photo on the right shows a view of the skull with hydrocephalus
Robinson-Fournier scars
Robinson-Fournier scars are recorded in 19% of children with late congenital syphilis. Their cause is diffuse papular infiltration of Hochsinger suffered in infancy. Radial scars are located on the chin, forehead, around the lips and corners of the mouth. Scars remain on the child’s skin after suffering from pyoderma, candidiasis and burns.
Rice. 13. The photo shows diffuse infiltration of Hochsinger’s skin in early congenital syphilis.
Dystrophic lesions of teeth
Pflueger's teeth (read above), an additional cusp on the side of the tongue on the first molars (Carabelli cusp), thinning of the free edge of the canine (Fournier's pike tooth), purse-shaped canines, widely spaced upper teeth, dwarf teeth and tooth growth on the hard palate are probable signs congenital syphilis.
Rice. 14. Carabelli tubercle is an additional tubercle located on the chewing surface of the first molar of the upper jaw (No. 5 in the figure). The anomaly is often bilateral.
Rice. 15. The photo shows widely spaced teeth and “Fournier pike teeth” in late congenital syphilis.
Early congenital syphilis
Now let's look directly at the clinic of early congenital syphilis.
According to the XXIX World Health Assembly, it is divided into several periods:
- 1. Early congenital syphilis, which is characterized by the manifestation of syphilitic symptoms. In this case, symptoms can appear either as those that first appeared in children under the age of two years, or as those that already occur before this age:
- Syphilitic pathologies of the skin and mucous membranes
- Syphilitic symptom associated with visceral lesions of the internal organs
- Syphilitic manifestations such as laryngitis, pharyngitis, pneumonia, etc.
- 2. The clinical syphilitic picture does not manifest itself in any way, but the serological reaction gives positive results. Repeated examinations of cerebrospinal fluid do not give a positive effect.
- 3. Positive results of early syphilis can be judged only on the basis of histological and bacteriological examinations.
Syphilis in children
Early congenital syphilis (before 1 year) manifests itself in the first 3 months. life in children whose mothers had secondary active syphilis. With congenital syphilis, there is general damage to internal organs, primarily the central nervous system, changes in the skin and mucous membranes (syphilitic pemphigus, diffuse Hochsinger infiltration, syphilitic rhinitis). The disease is accompanied by Parrot's pseudoparalysis - the formation of gummas (soft tumors) in the epimetaphyses of long tubular bones. Syphilitic damage to the nervous system is often represented by specific meningitis with convulsive syndrome, anisocoria and paralysis. Syphilitic meningitis develops gradually, without a pronounced temperature reaction. In the first weeks of life, hyperexcitability syndrome and seizures are observed. Meningeal syndrome is mild. The involvement of cranial nerves in the process is typical, since the pathological focus is localized at the base of the brain. A common complication is hydrocephalus. In its occurrence, the leading role is played by hypersecretion of cerebrospinal fluid and occlusion of cerebrospinal fluid spaces, which is associated with syphilitic damage to the membranes and ependyma of the ventricles.
In children from 3 months. distal peripheral paralysis of the upper limbs (Perthes palsy) occurs.
Syphilis in early childhood (from 1 year to 4 years) is accompanied by neurological disorders, represented by specific endarteritis, with vascular obliteration and cerebral ischemia. Central hemiparesis is characteristic, often with focal or secondary generalized seizures. In the vascular form, Argyll-Robertson sign, anisocoria, ptosis, strabismus and optic atrophy are possible. This form is characterized by delayed intellectual development.
Signs of late congenital syphilis (from 4 years of age) are divided into absolute (Hutchinson's triad - Hutchinson's teeth, keratitis, labyrinthine deafness) and relative (syphilitic chorioretinitis, saber-shaped shins, Robinson-Fournier scars, syphilitic drive, buttock-shaped skull, saddle-shaped deformation of the nose, dental dystrophy - Moon's tooth and Fournier's pike tooth).
Characteristic developmental defects in congenital syphilis are the Ausitidian sign (thickening of the sternal end of the clavicle), Gothic palate, Olympic forehead, infantile (shortened) Dubois-Hissar little finger, widely spaced upper incisors, absence of the xiphoid process of the sternum. Late (parenchymal) forms of neurosyphilis (damage to the brain and bone marrow) can be represented by Jacksonian epilepsy, ataxia, and a sharp lag in psychomotor development. Taste of the spinal cord occurs in children extremely rarely, mainly from 10 years of age. Among the early symptoms, it is necessary to note pelvic disorders (imperative urges with further development of urinary incontinence).
Progressive paralysis in children is observed from the age of 12 and is characterized by a slow increase in neurological symptoms in the form of mental retardation and behavioral disorders. In the absence of therapy, the duration of the disease is 5 years.
Untreated disease leads to miscarriage, premature birth, development of pathologies, stillbirth, or death in the first months of life.
What happens during the period of early congenital syphilis in the child’s body
According to research by many scientists, early congenital syphilis begins to form in the cells of the fetus.
Such a violation in the chromosomal apparatus leads to a genetic shift in development.
Depending on which gene chain was disrupted, different degrees of syphilitic manifestation are distinguished:
- Before the child is conceived
- Blastopathy – damage to the embryo during blastogenesis (formation of the embryo)
- Syphilitic embryopathy - damage to the fetus from four to five months of pregnancy
Syphilis of the brain
With syphilis of the brain, all vessels of the brain are damaged, with the capture of its mesodermal membranes.
It is this group that is characterized by the manifestation of meningism.
It occurs in the form of severe headaches, irritability, affective effects and constantly changing and fluctuating moods.
Hearing damage is also typical; deformation of the optic nerve occurs (deformation of the pupils), etc.
When diagnosing the Wasserman reaction (WRR), it is sharply positive, even when it is repeated.
Diagnosis of congenital syphilis
It is worth noting that congenital syphilis in 90% of cases can manifest itself in the form of blisters or so-called syphilitic pemphigus and ulcers.
Diagnosis can be made on the basis of biomaterial taken from these blisters and the detection of pale treponema in them.
However, this syphilitic manifestation may not always “show itself.”
Therefore, this type of diagnosis is not of particular value.
To confirm the diagnosis of congenital syphilis, they resort to the so-called lumbar puncture.
The cerebrospinal fluid is taken and examined using a microscope.
But if congenital syphilis has a hidden course, this method may not be successful.
Serological examination methods occupy a special place in congenital syphilis.
Namely, a blood test using the Wasserman method, now MRP, which can give false positive results in 50% of cases.
When examining for congenital syphilis, studies such as RIF, RIBT, RPGA (highly specific, highly sensitive reactions to syphilis) are important.
With congenital syphilis, almost 98% accuracy is obtained by examining the blood plus scraping the skin elements of the patient.
If there is any doubt about the presence of congenital syphilis, a diagnosis can be made using a complex of serological reactions (CSR).
It includes the complement bundle of RSC with Treponema pallidum antigens.
This type of analysis today is called ELISA and RPGA in combination with MRP (blood microreaction to syphilis).
Despite all its advantages, it can be a false negative if the collection or preparation for blood collection was incorrect.
If you have congenital syphilis or suspect it, you should contact more than just one venereologist.
The examination may involve a number of specialists.
Since the damage occurs not only from the skin, but also from internal organs, bones, brain (pulmonologist, surgeon, traumatologist, general practitioner, nephrologist, hepatologist, neurologist, etc.)
Primary syphilis: what you might not know about
From horror stories from Soviet propaganda, we know that syphilis is such a terrible disease in which the nose falls off. In addition to being properly intimidating, these ideas also had a downside. Like, if nothing hurts and your nose is still there, then it’s not syphilis... you can tolerate it.
Judging by the comments, including in my journal, many are still in such misconceptions to this day.
A little history
The science of syphilidology arose due to the enormous incidence of syphilis and its social significance. The experimental basis of syphilidology was often completely unethical experiments on people.
To understand how this terrible infection proceeds, healthy people were infected with syphilis (France, Russian Empire) or those infected were deliberately left without treatment (USA, Sweden, Norway). These absolutely inhumane experiments, however, brought a clear understanding of the stages of the infectious process and its patterns.
Onset of the disease. "Chancre"
Treponema pallidum, penetrating the body, spreads quite quickly through the lymphatic system and can enter any organs and tissues. However, the first manifestations of the disease should not be expected immediately, but after the incubation period, which averages one month. This period can vary from 9 to 90 days depending on many factors: taking antibiotics at this time, the presence of other diseases, alcohol or drug addiction; Also, the incubation period may change for those people who have encountered this infection more than once, etc.
You should know that syphilis infection can occur not only through sexual contact. And although there have been few such cases lately, they still occur.
So, after about a month, primary syphiloma (hard chancre) forms exactly in the place where the treponema was introduced. Dermatologists have a saying: “Syphilis is the first to punish the organ that sinned.”
So if the lesion is still on the genitals, and not in some other place, the “everyday” version of infection looks doubtful, although it is not excluded (and who said that medicine is easy?).
A chancre is an ulcer or erosion that, depending on its location, can look different, but, as a rule, it has a regular, round shape and clearly defined boundaries. Actually, the term “chancre” is not entirely adequate; it is more correct to say “primary syphiloma.”
The hard base of syphiloma, which gives the name to the symptom, is not always pronounced, and only a doctor can distinguish a specific ulcer from others. In most cases, chancre is completely painless, which misleads those suffering. 8 out of 10 victims, proudly entering my office and showing skin lesions, refer to very, very violent sex, sports, tight trousers and use the word “rubbed”... I have to disappoint them and send them for tests. And, on the contrary, patients who come with huge round eyes and shouts “Doctor, I think I have syphilis - it hurts so much that I can’t walk” more often find solace in some other diagnosis.
There are also atypical chancre. A chancre-felon (it is very painful), a chancre-amygdalitis (in the tonsils), a chancre-crack (in the folds of the skin, for example in the corner of the lips or the anus) and indurative edema, when the affected area swells, can develop on the fingers. But they are rare.
...And other symptoms
Other symptoms of infection include enlarged lymph nodes and lymphatic ducts. These appear as small, firm balls under the skin near the original lesion. If the primary lesion occurred on the genitals, then, accordingly, the lymph nodes will be enlarged in the groin area. The affected lymph nodes have a hard-elastic consistency, are not fused with the surrounding tissue, are not “hot”, and are painless.
The lymphatic duct may also be enlarged. It looks like a fairly dense, painless cord, reminiscent of a ballpoint pen refill that has gotten under the skin.
Attention! If you only have the last symptom, do not be alarmed, this may be a variant of the norm.
In general, the “troika” - primary syphiloma (chancroid), syphilitic lymphadenitis and syphilitic lymphangitis - makes up ALL the symptoms of primary syphilis. As you can see, syphilis already exists, but there are no falling noses yet, and not everyone will have them soon. But you need to be examined and treated, because there are no shameful diseases!
By the way, about analyzes
It is important to know that blood tests may be negative throughout the incubation period and as long as two weeks after the onset of symptoms. So if you took tests somewhere anonymously and you received a negative (good) result, but no one examined you, do not rush to rejoice. It’s better to have courage and go to a dermatovenerologist, because after the primary period (if left untreated), the secondary and tertiary periods may begin, and this is much worse.
But what about the USSR?
In the USSR there was syphilis. Both after the Civil War and after the Patriotic War. But really punitive Soviet venereology, grossly trampling on the rights of the sick in favor of the healthy, dealt with it. Only isolated cases remained, so students at that time had to see the above-described symptoms only on dummies. However, perestroika put everything in its place, now there is enough syphilis, and, of course, it is better to prevent it (read the article “
Prevention of sexually transmitted infections
"), than treatment.
If you are interested in what the secondary and tertiary periods of this disease look like (this is where the horror-horrors accumulate), what latent syphilis is, how this infection affects the nervous system and internal organs, and how dangerous this disease is for pregnant women, write questions in the comments, and I will try to answer them in the next article.
Leonid Shchebotansky
Photo istockphoto.com
Treatment of congenital syphilis, reasons for treatment failures
Syphilis is a very dangerous disease that has a very negative effect on an unborn or already born baby.
Therefore, all children must be preventively protected from this dangerous and formidable disease.
If suddenly this disease nevertheless overtakes your child, by order of the WHO there is a certain treatment regimen for congenital syphilis.
Attention! All recommendations and treatment regimens should be taken only after consultation with your doctor. This scheme is recommended for educational purposes only and is not intended to guide you and apply it in 100% of cases.
- 1. In most cases, penicillin, included in subgroup G (water-soluble), is used, 100,000-150,000 IU / kg / day (administer 50,000 IU / kg intravenously every 12 hours during the first seven days of life and then every nine hours). If this treatment was interrupted, the course is repeated again from the beginning.
- 2. The child is also prescribed benzathine penicillin G 50,000 units/kg intramuscularly once.
In general, treatment includes a whole series and complex of measures.
The doctor will tell you about them, who will prescribe the correct regimen, on which the effectiveness of the treatment itself will depend if you are suddenly overtaken by this disease.
Treatment of syphilis
Syphilis is perhaps the most feared disease. It is caused by a bacterial pathogen - a spirochete. Syphilis is transmitted from person to person through sexual contact. The possibility of becoming infected through everyday life - through a handshake, contact with a towel, door handle, etc. – practically equal to zero.
- Story
It is believed that syphilis arrived in Europe from America. It was brought by the sailors of Christopher Columbus, and at the turn of the 15th – 16th centuries the first pandemic of this disease broke out in Europe; you can read more about it in this historical essay
. Today, when personal protective equipment is available to everyone, and everyone knows about the dangers of STDs, syphilis still affects 3-4 people out of 1000 people.
- First stage
Approximately 3-4 weeks after unprotected sexual intercourse, a man develops an ulcer on his penis. It's called chancre - if you touch it, it's hard at the base. Sometimes it looks like a pimple, sometimes like a sore with a crater. It is painless and does not bother you. Usually a person thinks that it is a rub, or a bite, or an allergy. Classically, sexual contact is considered vaginal. But besides it, there can be anal contact and oral. With oral infection, a chancre forms on the lip or palate. Patients often confuse chancre in the anus with an acute form of hemorrhoids and do not always realize to get tested. Following the appearance of chancre, the lymph nodes enlarge, but the person may not feel this. If the patient discovers a chancre and consults a doctor, syphilis can be cured at the first stage.
- Second stage
After some time, the chancre goes away on its own, and the lymph nodes become smaller. But after about six months - and given the widespread use of antibiotics, it can take a year or a year and a half - a person develops nonspecific skin rashes. Even doctors can sometimes mistake them for an allergic reaction, and by that time the patient had already forgotten about that ulcer (chancre), which did not bother him at all. Papules appear on the palms - red nodules. Leucoderma appears around the neck - what was previously called the “necklace of Venus”. Today, there are many erased forms of secondary syphilis; instead of the classic “necklace of Venus”, 2-3 incomprehensible spots appear, which even a doctor cannot always identify. If the diagnosis has not been made, syphilis develops further.
- Third stage
Tertiary syphilis is characterized by gummous changes in tissues. Gumma (syphilitic granuloma) is a tissue node in which spirochetes are concentrated. Most often, gummas occur in the liver, soft tissues, and in the wall of the aorta. The tissues are irreversibly destroyed and rough knots are formed. If the spirochete enters the trunks of the nervous system, an extremely dangerous condition develops - neurophysilis. However, tabes dorsalis (a form of late neurosyphilis characterized by damage to the central nervous system) now practically does not occur. The artist Mikhail Vrubel suffered from tabes dorsalis - this is where his demons came from. more about the tragedy of Vrubel and his doctors in this article.
- Condylomas lata
Lata condylomas should not be confused with genital warts, which occur with the human papillomavirus. Previously, broad-pointed condylomas occurred at stages 2 and 3 of syphilis. But now, either due to the widespread use of antibiotics, or for some other reasons, condylomas can occur in the first stage. Due to the difference in the anatomy of the genital organs, men find condylomas more easily than women. If you see or feel that a condyloma has appeared on the genitals, do not try to determine on the Internet whether it is wide-ended or not, go to the doctor immediately.
- Test for syphilis
3 weeks after casual unprotected sexual intercourse (including oral and anal intercourse), it is necessary to take a specific RW test (Wassermann reaction, or simply “syphilis test”). There is no point in getting tested earlier, since the body’s immune response has not yet developed, and the test may give a false negative answer. A test for syphilis can be taken in any private laboratory, but it is best to go to a dispensary at your place of residence.
It is important to understand that if syphilis infection has occurred, the RW test will always be positive. In only 1 out of 10 patients, the syphilis marker disappears after treatment. The presence of a marker (positive RW analysis) may raise unnecessary questions during hospitalization, obstetrics, and professional examinations at work. Therefore, a sick person needs to undergo only legal treatment in a government medical institution licensed to treat syphilis. Such an institution will issue the patient a certificate stating that there was syphilis, the patient completed a course of treatment, was registered and deregistered, and is healthy. No private clinic has the right to treat syphilis and issue such certificates! A private clinic can only make a diagnosis and refer the patient to a public medical institution.
- Treatment of syphilis
Today, all over the world, syphilis is easily treated with long-acting penicillin antibiotics, which until recently were available in Russia. Treatment of syphilis with long-acting antibiotics is only 4 injections of extencillin. But now this drug is not available in Russia, and bicillin or penicillin is used in the treatment of syphilis - 6 injections daily for 10 days, the treatment is complex. The task of the state is to make the patient not infectious to society. Everywhere in the world, when syphilis is detected, the patient is given the first injection of the long-acting antibiotic extencillin - after which he is no longer contagious. Treatment with bicillin or penicillin does not give such a quick effect and the person continues to pose a danger to sexual partners until the end of the course of treatment with bicillin. If you are allergic to penicillin, treatment with second-line drugs, such as tetracyclines, is possible.
- What to do if accidental unprotected sexual intercourse occurs
Specific antibodies to syphilis and HIV appear in the blood 3 to 4 weeks after infection. But you should consult a doctor 1 week after suspicious sexual contact. You should not take any medications before consulting a doctor. The doctor will prescribe a special laboratory test called immunoblot. This is a highly specific and highly sensitive method that allows you to detect traces of developing antibodies to the causative agent of syphilis.
For patients who have had syphilis in the past, it is important to understand the difference between a total test for immunoglobulins M and G and their determination in the blood separately. Their total analysis will always be positive, because immunoglobulin G remains in the blood of those who have previously had syphilis. Only immunoglobulin M indicates a new infection. This is a rather complex question; you should not solve it yourself using the Internet.
After suspicious unprotected sexual intercourse, a blood test is required for syphilis, an HIV test (this is also taken no earlier than 3-4 weeks after contact) and hepatitis C, which is easily transmitted through sexual contact. At the same time, a scraping is taken from the urethra or from the vagina and cervix for markers of diseases that are predominantly sexually transmitted. Their pathogens include gonococcus, trichomonas, ureaplasma, metaplasma, chlamydia, candida, gardnerella. The only correct approach to suspicious unprotected sexual intercourse is to take the entire set of tests.
- How to protect yourself from sexually transmitted diseases
A good condom guarantees protection against STDs, provided that it is put on correctly, that it does not burst, and that extragenital contacts - oral and anal - were also carried out in a condom. Today, there is no better protection against STDs than a condom. Treating the genitals with drugs like Miramistin is not effective!