Scleroderma is a systemic progressive lesion of connective tissue with a predominance of fibrosclerotic and vascular disorders of the type of obliterating endarteritis with widespread vasospastic changes developing mainly in the skin and subcutaneous tissue.
As follows from the works of Hippocrates, Galen, and Avicenna, cases of scleroderma were known in ancient times. The first description of this disease was made by Zacutus Lusitanus in 1634.
Scleroderma is the second most common disease, after lupus erythematosus, from the group of diffuse connective tissue diseases.
The pathogenesis of scleroderma is complex. Changes in immune status occur, and autoimmune disorders are of great importance.
In patients with scleroderma, the body produces antibodies to its own cells. The reasons for this are currently unclear. The body begins to perceive a certain type of its own cells as foreign antigens and produce antibodies against them to eliminate them. This is called an autoimmune disorder.
The role of genetic factors, vascular, metabolic, neuroendocrine disorders, as well as disturbances in the functioning of the autonomic nervous system is assumed. There is an infectious hypothesis of its occurrence.
The prevalence of the disease is 32-45 cases per 100,000 population (Dovzhansky S.I. 1979). This disease occurs more often in women (3:1 in relation to men), with 75% of cases occurring between the ages of 40 and 55 years. People of other ages can also get sick, starting from birth and ending with people over 60 years of age.
Scleroderma is divided into two main forms - limited and systemic, each of which has its own clinical varieties.
According to WHO recommendations, only systemic scleroderma is included in the group of diffuse connective tissue diseases, although most researchers consider these forms as manifestations of a single process.
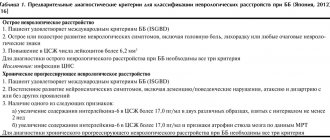
Classification of focal scleroderma (Dovzhansky S.I. 1979)
- Discoid, or plaque, scleroderma:
- superficial “lilac”
- indurative-atrophic
- deep knotty
- bullous
- generalized
- Linear:
- reminiscent of a “saber strike”
- strip-like or ribbon-like
- zosteriform
- Guttate (white spot disease, lichen sclerosus, Tsumbusha's lichen alba).
- Atrophy idiopathic Pasini-Pierini.
There are three stages in the development of the disease (clinical picture):
- Edema
- Seal
- Atrophy
Scleroderma - symptoms and treatment
Scleroderma can manifest itself with a variety of symptoms associated with damage to various internal organs and systems: Raynaud's phenomenon (pain in the fingers and discoloration of the skin), heartburn, swelling, polyarthralgia (joint pain), dysphagia (swallowing disorder), severe skin thickening and joint contracture fingers (inability to bend and straighten them completely).
Skin changes may suggest scleroderma . They go through three stages:
- Dense swelling without pitting, disappearance of skin folds.
- Induration is thickening and hardening of the skin and subcutaneous tissue.
- Atrophy: tension, thinning of the skin, cessation of hair growth, atrophy of sweat glands, hyper- or hypopigmentation: whitish or brown spots and their alternation - a “salt and pepper” sign.
sclerodactyly subsequently develops - damage to the skin of the fingers involving the subcutaneous tissue, ligaments and tendons, leading to impaired movement in the joints of the hands.
Another sign of scleroderma is calcification , a subcutaneous deposition of calcium salts in areas of high pressure, such as the fingertips, buttocks, elbows, knees, and tendons. Sometimes the deposits break open, releasing a white crumb-like mass, after which poorly healing ulcers form.
Facial changes with scleroderma are specific: the red border of the lips becomes thinner, the “purse-string mouth” symptom appears, and opening the mouth causes difficulty. The nose is sharpened, wrinkles are smoothed out. The face becomes motionless, mask-like, and typical facial expressions when expressing emotions disappear.
One of the main and earliest manifestations of the disease is Raynaud's phenomenon - episodic attacks affecting the fingers of the limbs and occurring classically in the form of a sequential change of three phases (white, blue, red):
- pallor (peripheral vasospasm);
- cyanosis (impaired local blood flow);
- the appearance of a burgundy-red color of the skin (dilation of blood vessels and active blood flow through them).
In severe forms of Raynaud's phenomenon, due to prolonged ischemia, ulcers may form on the fingertips, healing with the formation of small scars.
Telangiectasias are also common vascular lesions - red dots on the skin of the face, torso and limbs associated with dilation of the capillary bed vessels. When pressed they disappear and then reappear.
Joint pain is associated with fibrosis of periarticular tissues. Tendon fibrosis also causes friction noise during movement. The joints of the hands are most often affected. osteolysis is possible - spontaneous resorption of the nail phalanges, leading to shortening and deformation of the fingers.
Muscle weakness or muscle pain is also common with scleroderma, as is muscle atrophy and hardening—muscle fibrosis.
Lesions of the gastrointestinal tract begin in the oral cavity. Patients may develop “dry syndrome ,” in which the amount of saliva decreases and its viscosity increases. This leads, on the one hand, to disruption of the initial stages of food digestion with the participation of salivary enzymes, and on the other hand, to the development of caries and stomatitis due to the loss of the bactericidal properties of saliva.
Serious changes affect the esophagus with scleroderma, which is manifested impaired swallowing due to the replacement of the muscular layer of the esophagus with fibrous connective tissue and the difficulty of “pushing” the bolus of food towards the stomach. Patients may also experience reflux esophagitis , in which stomach contents are refluxed into the esophagus, which leads to the formation of erosions and ulcers of the mucous membrane of the lower third of the esophagus. In this case, the main complaint may be heartburn and chest pain . Due to deterioration of blood flow in the small vessels of the stomach, damage to its mucous membrane can form - erosions and ulcers, characterized by “hunger pains” , pain an hour after eating, nausea. Some patients develop watermelon stomach syndrome, when the risk of bleeding and associated anemia increases due to dilation of the veins in the antrum of the stomach.
Damage to the small intestine is manifested by malabsorption syndrome - impaired absorption. Because of this, a deficiency of vitamins, minerals and microelements occurs, and the patient loses body weight. Possible bloating and overgrowth of bacteria in the intestines.
Decreased colonic motility due to atrophy of the muscle layer leads to persistent constipation .
Dysfunction of the pancreas and liver is manifested by flatulence, pain, food intolerance, etc.
Some patients with scleroderma develop biliary cirrhosis, the manifestations of which are jaundice, itching, and increased bleeding .
Lung damage ranks second after pathologies of the gastrointestinal tract in terms of frequency of occurrence in scleroderma. Pulmonary fibrosis leads to a decrease in the area of gas exchange in the lungs and provokes compression of blood vessels. Due to a decrease in the elasticity of the walls of the lung vessels and a decrease in their lumen, pulmonary arterial hypertension (PAH) is formed, that is, the pressure in the vessels of the lungs increases. Due to these pathological processes, arterial blood is less saturated with oxygen. The main complaint of patients with vascular lung disease is shortness of breath , and with the development of pulmonary fibrosis, shortness of breath is combined with a non-productive cough without sputum production.
Heart damage can manifest itself as arrhythmias , attacks of chest pain similar to angina pectoris.
Kidney damage in scleroderma is of a vascular nature. Hypertensive renal crises are typical, when blood pressure reaches 200-220 mm Hg. Art. and there is a risk of severe complications (heart attacks, strokes, acute renal failure). A renal crisis is an emergency condition, and care is provided in a medical hospital. Sometimes kidney damage develops asymptomatically and leads to progressive renal failure.
The organ of vision also suffers, and “dry eye syndrome” may develop, associated with a decrease in tear production, which leads to drying out of the cornea and the occurrence of infections [1][2][3][4][5][10][11].
Diagnostics
Scleroderma can often be difficult to diagnose because it can be similar to many other diseases. Changes in skin thickness, the presence of certain antibodies in the blood, or early changes in blood vessels can be helpful in diagnosing the disease. If necessary, a biopsy can be taken to analyze the tissue, which also helps make the diagnosis.
One useful test is nail capillary analysis. It is based on the early manifestation of scleroderma and is manifested by the disappearance of capillaries in the skin of the arms and legs. For this analysis, a microscope or magnifying glass is used and the skin in the nail area is viewed. For an accurate diagnosis, it is necessary to compare both laboratory research methods, clinical data, and medical history.
Causes
The exact causes of scleroderma have not yet been determined. Experts identify predisposing factors, the presence of which increases the risk of autoimmune disease. These include:
- Genetic predisposition. The presence of scleroderma in relatives significantly increases the likelihood of developing the disease in future generations. There is a theory according to which a defect in the HLA-9QA1 gene is responsible for the formation of an autoimmune disease. Genome mutations can be congenital or acquired. The following factors contribute to the development of a genetic defect:
- Radiation exposure.
- Prolonged exposure to ultraviolet rays.
- Taking certain medications. For example, cytostatics.
- Viral or bacterial infection.
- Exposure to high and low temperatures.
- Inflammatory process. Biologically active substances produced during the inflammatory reaction can provoke tissue and vascular changes. Vascular permeability increases, and the inflammatory process intensifies. As a result, the prerequisites are created for the formation of chronic inflammation. The risk of scleroderma increases with the addition of other provoking factors.
- Immune disorders. Scleroderma is an autoimmune disease in which the body's own cells are perceived as foreign. Immune reactions are triggered by connective tissue growth factor.
- Infectious diseases. There is no consensus regarding the involvement of infectious agents in the development of scleroderma. Experts do not identify a specific pathogen that provokes autoimmune processes. It was noticed that in some patients with diagnosed scleroderma, cytomegalovirus fragments were detected.
- Environmental factors. Experts highlight a theory according to which there is a relationship between exposure to environmental factors and the occurrence of scleroderma. If there is a genetic predisposition, exposure to environmental factors increases the risk of developing an autoimmune disease. The main provoking factors include:
- Chemical compounds. For example, silicon, mercury, benzene, toluene, epoxy resin.
- Nutritional supplements. Among them are L-tryptophan, mazindol, fenfluramine.
The mechanism of scleroderma occurrence is associated with the development of an immune response against the body's own cells. As a result, an inflammatory process is formed, thinning the skin and blood vessels. Circulating complexes settle on internal organs, causing their damage. Scleroderma is accompanied by the formation of sclerotic changes with the formation of scar tissue.
Forecast
Life expectancy and prognosis for scleroderma are determined by the nature of its course. In accordance with this, the following types of disease are distinguished:
- Spicy. Scleroderma is characterized by rapid development and early onset of severe clinical symptoms. In this case, the prognosis for recovery and life is considered unfavorable. As a rule, the acute course of the pathology leads to multiple organ damage a year after the onset of the disease. Acute scleroderma is considered the most dangerous and severe form of the disease.
- Subacute. The autoimmune disease develops quickly, however, tissue sclerosis occurs more slowly than in the acute course. This provides a more favorable prognosis. The success of therapy depends on the degree of activity of scleroderma.
- Chronic. The development of the disease occurs slowly. In this regard, the prognosis becomes favorable.
Scleroderma is an incurable disease. Compliance with treatment and lifestyle recommendations allows you to maintain long-term remission. Preventive measures include:
- Regular medical examination. This is necessary when signs of exacerbation appear, as well as in the case of a stable condition to control the disease over time.
- Taking medications. Self-adjustment of the dose of prescribed medications is not allowed without consultation with your doctor.
- Avoiding hypothermia and fatigue. A prolonged stressful situation can provoke an exacerbation of scleroderma. Therefore, it is necessary to observe a work schedule with rest breaks.
- Maintaining a rational and balanced diet. There is no specific diet for scleroderma. However, it is recommended to include foods rich in vitamins, minerals, and microelements in your daily diet. The menu limits the amount of salt and water, as well as vitamin C due to its stimulating effect on the growth of connective tissue.
Compliance with the above recommendations will help minimize the number of exacerbations of scleroderma. When the first signs of the disease appear, you must seek medical help for diagnostic measures. In this way, the development of complications and severe scleroderma can be prevented.
Discussion
The presented patients demonstrate the difficulties of the diagnostic search due to the clinical picture atypical for scleroderma. In patient G., the skin rashes were distinguished by an annular shape, unusual for plaque scleroderma, and were similar to the atrophic form of lichen planus or granuloma annulare. In addition, these rashes turned out to be resistant to the prescribed standard therapy.
Other clinical cases of deep scleroderma show us the peculiarities of the scleroderma process in the lower extremities, which in their debut simulated the clinical manifestations of vasculitis, lupus erythematosus or toxicoderma, which led to a delayed correct diagnosis. Treatment prescribed to patients without taking into account data from previously performed pathohistological studies led to a pronounced spread of the pathological process into the deeper layers of the dermis and subcutaneous fat.