Quick transition Treatment of cutaneous lupus erythematosus
Systemic lupus erythematosus is treated by a rheumatologist. During therapy with antimalarial drugs (hydroxychloroquine, chloroquine), observation by an ophthalmologist is necessary. If you suspect the development of squamous cell skin cancer against the background of discoid lupus erythematosus, consultation with an oncologist is necessary.
Lupus erythematosus rashes on the skin and/or mucous membranes can be an independent disease or a manifestation of systemic lupus erythematosus, a chronic disease associated with the formation of antibodies to components of cell nuclei. Antibodies cause damage and inflammation of various tissues, including the skin.
Forms and complications
Skin manifestations of lupus erythematosus include three groups, each including specific skin manifestations:
- acute cutaneous lupus erythematosus (localized, generalized and toxic epidermal necrolysis-like);
- subacute cutaneous lupus erythematosus (ring-shaped, papulosquamous, drug-induced, erythrodermic, poikilodermic, vesiclobulous, Rowell syndrome);
- chronic cutaneous lupus erythematosus (discoid, edematous, panniculitis, pernioid, lichenoid).
The identification of these forms is due not only to the duration of the skin disease, but also reflects the connection with systemic lupus erythematosus.
Most often, the manifestation of systemic disease is acute forms, while the discoid form is observed only in 5-15% of all cases. The longer skin manifestations exist in isolation, the lower the risk of developing a systemic form of the disease. The risk of systemic disease in the presence of cutaneous manifestations is higher in women and children.
Lupus erythematosus rashes can occur in children (antibodies are passed on to the fetus) from mothers with systemic lupus erythematosus. This form is called neonatal lupus, occurs during the first two months of a child’s life and may be the first sign of systemic lupus erythematosus in the mother.
The systemic lupus erythematosus complex may also include other changes in the skin and its appendages that are not specific exclusively to this disease.
Case history of systemic lupus erythematosus
Despite the fact that people have been suffering from lupus erythematosus for a long time, it was only in 1828 that the French dermatologist Laurent Biett drew attention to a peculiar pathology of the facial skin “in the shape of a butterfly” and described some of its symptoms.
After 45 years, the Hungarian dermatologist Moritz Kaposi noted that lupus erythematosus leads not only to skin damage, but also to inflammation of internal organs .
Then in 1890, the English physician William Osler made the important observation that sometimes SLE can occur without skin manifestations.
In 1948, so-called Le-cells were discovered - specific cells of lupus erythematosus, and 6 years later antibodies were discovered that were directed at the cells of one’s own body. This discovery formed the basis for the development of sensitive tests for diagnosing SLE.
Symptoms
The skin manifestations of lupus erythematosus are diverse. A significant manifestation, almost always associated with a systemic disease, is a rash on the face, shaped like a butterfly: with wings on the cheekbones and cheeks and a body on the bridge of the nose and bridge of the nose. The rash may appear as raised or deep-lying elements of pink and bluish-red color. There is a tendency to form ring-shaped lesions covered with very dense scales that are painful when removed. In some cases, the so-called lupus erythematosus pernio is formed, in which painful bright red bluish nodules appear on the toes, hands, nose, and ears in cold weather. Damage to blood vessels is accompanied by the appearance of rashes resembling bruises; dilated vessels can be visible in the nail beds. Some patients with SLE have symptoms resembling lichen planus.
There are also severe lesions with the formation of blisters and peeling of the skin, which is more typical for the onset of a systemic disease. Changes can affect the mucous membranes, especially often the mucous membranes of the lips and oral cavity. Lupus lesions on the scalp may result in hair loss. Diffuse hair loss and hair thinning are also possible.
Causes of systemic lupus erythematosus
The exact reason why some people get systemic lupus erythematosus and others do not is unknown. But scientists suggest that this disease has a genetic predisposition. For example, it is not uncommon for members of the same family to become ill with lupus erythematosus.
With lupus erythematosus, the immune system fails, it ceases to distinguish between “self” and “foreign cells” and begins to produce antibodies against the DNA of the cells of its own body. The appearance of a large number of antibodies leads to the formation of inflammatory processes throughout the body.
The trigger for the onset of the disease can be several factors:
- taking certain medications: antibiotics, sulfonamides, vaccines;
- change in the ratio of hormone levels (androgens and estrogens);
- prolonged exposure to the sun;
- hypothermia of the body;
- endocrine system disorders;
- long-term stress.
In addition, there is an assumption that the disease may be triggered by a viral infection.
Treatment of cutaneous lupus erythematosus
The basis of treatment is corticosteroid hormones. With this disease, they can be applied to the lesions in the form of ointments, or injected directly into the lesion of the affected skin. In severe cases, systemic corticosteroids may be prescribed. As an alternative or to enhance therapy, it is possible to apply calcineurin inhibitors to the lesions.
In cases of severe skin damage and insufficient effect of external treatment, systemic therapy is carried out using antimalarial drugs (chloroquine, hydroxychloroquine), anti-inflammatory drugs (methotrexate, mycophenolate, dapsone, azathioprine, etc.).
Features of the treatment method
The first line of treatment is topical corticosteroids and hydroxychloroquine.
To reduce the total dose and side effects of topical corticosteroids, calcineurin inhibitors are included in treatment.
During treatment with hydroxychloroquine, regular medical supervision is necessary. The condition of the retina must be monitored, since the drug can impair vision with long-term (more than 5 years) use. This side effect is uncommon, but signs of retinal damage may require discontinuation of the drug.
Intralesional administration of drugs (corticosteroid hormones) using multiple superficial injections directly into the lesion of the affected skin allows you to create a high concentration of the drug in the lesion, while reducing the risks of systemic side effects. The medicine is administered by a doctor in a dressing room to a depth of 2-3 mm. The procedure is painful, but the pain is not sharp and largely depends on the sensitivity of the patient’s receptors. To reduce pain, a thin needle is used, and an anesthetic ointment may be used.
All patients must be prescribed skin protection against ultraviolet radiation.
How is lupus erythematosus treated at the Rassvet clinic?
The dermatologist will ask you to talk about the course of the disease and the treatment that was carried out previously. The doctor will examine the skin (including the scalp) and mucous membranes. Dermatoscopy and trichoscopy can be informative. With this disease, to establish a diagnosis in most cases, a skin biopsy will be required with an additional immunofluorescence reaction.
If cutaneous lupus erythematosus is suspected, it will be necessary to discuss the possibility of systemic manifestations and assess the condition of other organs and systems of the body. Additional studies may be required to identify a systemic process (blood tests, urine tests, etc.).
Lupus erythematosus: skin lesions
Lupus erythematosus (LE) is a multifactorial autoimmune inflammatory disease of connective tissue that affects various organs and systems and has a wide range of clinical manifestations.
The incidence of cutaneous forms of LE is 3.0–4.2 cases per 100,000 population per year, while patients with discoid LE account for 70–80%. The onset of the disease is most often observed between the ages of 20 and 40; women are affected more often than men.
There are specific and nonspecific skin lesions with LE. Among specific skin lesions, chronic, subacute and acute forms of the disease are distinguished.
Clinical picture
Discoid LE is characterized by a triad of symptoms: erythema, hyperkeratosis and atrophy. Lesions can be localized (affecting mainly the facial area (cheekbones, cheeks and wings of the nose), ears, scalp) or widespread. Hyperemic spots appear on the skin, which slowly increase in size, infiltrate and turn into raised plaques. On their surface in the central part, first follicular and then continuous hyperkeratosis appears. Along the periphery of the lesions, a zone of active inflammation remains and there is hyperpigmentation. The plaques slowly increase in size; in the central part, resolution of the elements is observed with the formation of rough sinking disfiguring cicatricial atrophy of the skin, against which telangiectasia may appear.
In the area of the red border of the lips, the rashes are represented by slightly infiltrated cherry-red spots, covered with a small number of difficult-to-remove scales. When the scalp is affected, erythema of various shapes develops with peeling on the surface, upon resolution of which cicatricial atrophy, telangiectasia and areas of hypo- and hyperpigmentation remain. A zone of cicatricial alopecia is formed in the center of the lesions; the presence of areas with preserved hair in the lesions of baldness is characteristic.
Deep LE (lupus panniculitis) is clinically manifested by one or more deeply located dense nodes, mobile, clearly contoured and not fused to the surrounding tissues. The skin over the nodes has a stagnant cherry coloration; there are often foci of erythema and hyperkeratosis, characteristic of discoid LE (a combination of deep and discoid LE). After the nodes resolve, areas of subcutaneous tissue atrophy remain, manifested by deep recesses. In some cases, the nodes may ulcerate, forming rough, retracted scars during healing. Deposition of calcium salts in the skin with the formation of calcifications is possible. The rash is usually localized asymmetrically on the face, neck, shoulders, mammary glands (lupus mastitis), thighs and buttocks.
With verrucous (hypertrophic) LE, the development of single, sharply protruding plaques above the skin level with pronounced hyperkeratosis and a warty surface is noted. The most common localization of this form of CV is the face, the dorsum of the hands, and the extensor surfaces of the forearms and shoulders. Verrucous LE can be combined with discoid LE, which facilitates the diagnosis of the disease. Resistance of the rash to the therapy is noted.
Tumor-like LE is considered by a number of authors as a chronic cutaneous form of LE, while others classify it as an intermediate form of the disease. The clinical picture is represented by skin rashes in the form of dense urticaria-like papules and plaques of red color (from pink to bluish), round, irregular or ring-shaped, with clear boundaries, with a shiny surface, which are localized in areas exposed to insolation - in the upper chest area , back, shoulders, neck, face. Sometimes elements can merge to form polycyclic figures. Exacerbations of the disease are more often observed in the spring and summer. The rash may resolve spontaneously without a trace after a few weeks or persist for a long time. Annual exacerbations of the disease are often observed after exposure to the sun with the reappearance of elements in the same places.
LE of the mucous membranes can develop simultaneously or precede skin lesions. This form of the disease is rarely diagnosed in a timely manner (in 10–50% of cases). Rashes are most often observed on the mucous membrane of the oral cavity, but can be localized in the nasal cavity, on the genitals, and conjunctiva. The elements are represented by hyperemic spots, bluish-red papules, covered with whitish layers, and rarely - blisters. Painful erosions and ulcers may develop. Resolution of the rash is often accompanied by the formation of scars or cicatricial atrophy.
Subacute cutaneous LE has a transitional clinical picture between acute and chronic LE. This form is manifested by the development of papulo-squamous or ring-shaped erythematous rashes. In psoriasiform LE, the elements are represented by hyperemic papules and small plaques in the area of the shoulders, upper chest and back, rarely on the skin of the face, ears, and scalp, which can merge with each other. On the surface of the spots and plaques there are tightly packed scales and slight hyperkeratosis, which intensifies in the area of the mouths of the hair follicles. The ring-shaped form of the disease is characterized by the formation of hyperemic spots and erythema in the form of rings and polycyclic figures with hyperkeratosis and peeling on the surface, which are located mainly in areas of the skin exposed to insolation. A combination of papulo-squamous and ring-shaped forms in one patient is possible. Rashes with subacute cutaneous LE can resolve without scars, forming long-term foci of hypopigmentation with telangiectasia on the surface, or form very superficial cicatricial atrophy. This category of patients often has relatively mild systemic manifestations of CV: arthralgia, arthritis and other symptoms of damage to the musculoskeletal system without involving the kidneys, central nervous system, or serous membranes in the pathological process.
The acute cutaneous form of LE is always a manifestation of systemic LE, which manifests itself with skin lesions in 70–85% of cases. The acute form of CV is characterized by the development of erythema on the skin of the face in the area of the cheekbones, cheeks and nose (“butterfly wings”) with a cyanotic tint in the center and swelling. Less common are common maculopapular rashes. Elements of the rash usually appear after sun exposure, last a few days and resolve, leaving minor hyperpigmented spots. A peculiar equivalent of the “butterfly” is centrifugal erythema of Biette, which occurs in the cheek area in the form of slightly swollen, bright hyperemic spots, slowly increasing in size due to peripheral growth and simultaneously resolving in the central part. Possible damage to the red border of the lips, development of facial swelling, and the appearance of widespread maculopapular rashes on symmetrical areas of the skin. Damage to the mucous membrane of the oral cavity, hard palate, and nose can occur with the formation of erosions and ulcers. In rare cases, the clinical picture of the acute cutaneous form of LE may be similar to toxic epidermal necrolysis.
Patients with cutaneous forms of LE often experience overlapping manifestations of skin lesions. Two or more clinical forms of cutaneous LE are observed in 35% of patients, acute cutaneous LE associated with discoid LE – in 30%, with subacute cutaneous LE – in 14%, with discoid and subacute cutaneous LE – in 15% of patients.
The probability of developing SLE is up to 90% in acute LE, 35–50% in subacute LE, about 20% in common forms of chronic LE and no more than 5% in localized discoid LE.
Complaints and anamnesis
Patients complain of rashes, usually not accompanied by subjective sensations.
The appearance of rashes can be promoted by solar or ultraviolet radiation. Exacerbations of the disease are more often observed in the spring and summer.
Treatment
Topical glucocorticosteroid drugs and systemic antimalarial drugs are used as first-line treatment for CV with skin lesions.
Rehabilitation of patients with CV is achieved in local resorts. Physiotherapy and spa treatment in the south of the country with insolation are contraindicated for patients with CV. They need to refrain from swimming in hot baths, steam rooms, saunas, and it is undesirable to stay near a hot stove for a long time. Optimal working conditions for patients are to work in dry, warm industrial premises
All patients with CV are recommended to take measures to protect their skin from sun rays: wearing hats, long-sleeved clothing with a closed neckline, trousers and long skirts, regular applications of photoprotective creams with a high SPF index (>50).
It is recommended that patients with lupus erythematosus be monitored by a dermatovenerologist, rheumatologist, general practitioner, endocrinologist, neurologist, gynecologist with a comprehensive clinical and laboratory examination. Clinical observation of these patients can significantly improve the prognosis of the disease. Clinical examination of patients with lupus erythematosus provides a full examination, timely treatment of concomitant diseases, chronic foci of infection, and implementation of health-improving measures.
Kikot I.V.
Discoid lupus erythematosus in men
According to statistics, this type of lupus erythematosus occurs more often in women than in men. Out of 200 cases of the disease, only 3 affect men. It is also known that this disease is found in blondes more often than in brunettes. The disease often occurs in countries with a cool maritime climate and high humidity. In tropical climates, discoid lupus is not as common, although there is active ultraviolet radiation. Researchers attribute this phenomenon to the darker skin of local residents.
The prevalence of the disease among women is explained by the fact that females have thinner and more delicate skin, and they also have much more active hormonal processes in the body. Among the causes of female CV incidence are also pregnancy and the first time after childbirth.
Discoid lupus erythematosus occurs mainly in women aged 20 to 40 years. And among men, children and the elderly, only 3% of cases of the disease.
Glucocorticosteroids
They are among the most common and effective drugs for the treatment of systemic lupus erythematosus. Long courses of taking glucocorticosteroids significantly alleviate the general condition and reduce the severity of clinical signs. There are several ways to take medications. One of them is pulse therapy, in which a large dose of the drug is administered simultaneously. The dosage is individual and depends on body weight. The combined use of glucocorticosteroids and cytostatics is recommended. Indications for pulse therapy are:
- Rapidly developing lupus nephritis.
- Damage to the central nervous system.
- High disease activity.
Cytostatics
A group of anticancer drugs whose mechanism of action is to disrupt cell division. The main indications for the use of this group of drugs for systemic lupus erythematosus include:
- Ineffectiveness of taking glucocorticosteroids.
- High disease activity.
- Vasculitis.
- Presence of acute lupus nephritis.
- Carrying out pulse therapy in combination with glucocorticosteroids.
Nonsteroidal anti-inflammatory drugs
To reduce the activity of the inflammatory process and relieve pain, NSAIDs are prescribed. When body temperature rises, anti-inflammatory drugs are used as antipyretic therapy.
Aminoquinoline drugs
Systemic lupus erythematosus occurs with the development of photosensitivity. To reduce the severity of this symptom, aminoquinoline drugs are used. They have anti-inflammatory and immunosuppressive effects.
Biological products
Biological drugs are considered a promising development in the treatment of systemic lupus erythematosus. Medicines in this group have fewer side effects compared to glucocorticosteroids. Mass use of biological drugs is difficult due to their high cost.
In case of severe disease, extracorporeal therapy is performed. Her methods include:
- Plasmapheresis. The method of blood purification involves partial removal of plasma from the body. This reduces the number of antibodies that cause SLE.
- Hemosorption. Specific sorbents used in hemosorption purify blood outside the body.
The choice of treatment method depends on the stage of development of systemic lupus erythematosus. Specialists at the Yusupov Hospital provide a full course of therapy for autoimmune diseases, taking into account the individual characteristics of the pathology, as well as concomitant diseases. The clinic's rheumatologists have many years of experience in dealing with the manifestations of systemic lupus erythematosus, which helps to alleviate the condition and reduce the severity of clinical symptoms in the shortest possible time.
Prevention
Specific prevention of DLE has not been developed today because the causes and pathogenesis remain a mystery to researchers. To prevent recurrence of the disease after recovery, preventive courses are carried out in spring and summer. Prevention includes the use of antimalarials. First, 1 tablet is given per day, then the number of tablets per week should be 2-3.
Other methods of prevention: tablets and injections of nicotinic acid, as well as photoprotective drugs. A person should spend a minimum amount of time in cold and too hot rooms. It is not recommended for him to be exposed to the wind or frost in winter, or to be in direct sunlight during the hot season.
If possible, operations, vaccinations and vaccinations, as well as injury should be avoided. You need to do physical exercise, walk in the park, forest or other places in the fresh air. The patient's diet should be complete, with a small amount of salt and sugar, without alcoholic beverages.
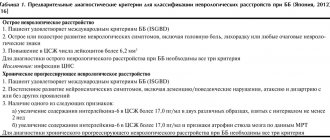
Diagnosis of systemic lupus erythematosus
Diagnosis of systemic lupus erythematosus is a complex sequential process consisting of several stages. First, a detailed collection of symptoms and signs in the chronological order of their occurrence is required. Secondly, a set of specific tests is required to confirm the diagnosis. Each case history of systemic lupus erythematosus is individual, as is the treatment mechanism for each patient.
Making a diagnosis requires a highly qualified rheumatologist and a responsible attitude on the part of the patient - he needs to be constantly observed by the same specialist, regularly take tests and conduct the necessary research.
Unfortunately, there is no single specific test to make the diagnosis of SLE. The doctor has to evaluate the totality of signs and test results.
In addition to collecting a medical history (including family history) and a complete examination of the patient (from head to toe), the doctor requires the following laboratory tests to make a diagnosis:
- general blood test with determination of leukocytes, erythrocytes, platelets;
- blood chemistry;
- study of autoantibodies (antinuclear antibodies, antibodies to double-stranded DNA, anti-ribonucleoprotein (RNP), anti-RO, anti-La antibodies);
- Wasserman reaction - a blood test for syphilis, which can be false positive;
- sometimes a skin and or kidney biopsy is required.
It is mandatory to perform an analysis for antinuclear antibodies and antibodies to DNA, a general and biochemical blood test, a urine test, and an ESR. This data allows the specialist to monitor the course of the disease.
Diagnostics
Diagnosing discoid lupus erythematosus generally does not cause difficulties. Doctors pay attention to the typical clinical picture of the patient. It is worth noting that diagnostic laboratory research methods do not reveal changes in indicators; deviations from the norm are often not observed.
Histological and other methods for making a diagnosis are mainly used to distinguish the disease from similar ones. Differential diagnosis is carried out with the following pathologies:
- eczema
- psoriasis
- pseudopelada
- lymphoplasia
- favus
- sarcoidosis
Experienced specialists easily distinguish lupus erythematosus from psoriasis. In cases of CV, the majority of rashes are on the face. Psoriasis does not typically affect the face, except in cases of children. In case of psoriasis, scales are removed easily and painlessly, but in case of lupus they are difficult to separate, and painful discomfort occurs when removed. Seborrheic eczema differs from discoid lupus erythematosus by itching of the affected areas. The scales are fatty, they do not have the typical “spikes” mentioned above.
To clarify the diagnosis, the following studies may be needed:
- histological examination of tissues (they take a piece of skin or other affected tissue and conduct a microscopic analysis of it to learn about external changes, cellular composition and condition)
- microscopic examination of hair and scales (makes it possible to identify the pathogen)
- immunofluorescence study (immunological method)
SLE symptoms, complaints and clinical manifestations
Redness (erythema) of the facial skin in the cheeks and nose
This is the most characteristic symptom of systemic lupus, which occurs or worsens when exposed to direct sunlight. Because of its characteristic shape, this erythema became known as “lupus butterfly.” Similar skin rashes may also occur in other areas. The skin of the fingers often changes color under the influence of cold from white to purple-bluish ( Raynaud's phenomenon ). of ulcers on the oral mucosa is possible alopecia ) and brittleness of the nail plates.
Pain and inflammation (swelling) of the joints
They occur frequently, but do not lead to the destruction of joint structures, as happens with rheumatoid arthritis. The small joints of the hands are most often affected, but arthritis of the large joints is also possible. Characteristic signs of inflammatory joint pain are morning stiffness (> 1 hour), increasing pain at rest and weakening with movement.
Pleurisy and pericarditis
A common symptom of lupus is inflammation of the pleural membranes lining the inside of the chest (pleurisy) and the heart sac (pericarditis), which can manifest as pain in the chest during breathing movements.
Kidney damage
When internal organs are involved in the process, kidney damage most often occurs, usually occurring unnoticed in SLE. Edema and a persistent increase in blood pressure are indirect signs of this serious complication.
Inflammatory changes in the nervous system. They can manifest themselves in a wide variety of ways (from headaches and psycho-emotional disorders to convulsive seizures).
Antiphospholipid syndrome. Also, with systemic lupus erythematosus, the formation of “immune agents” (antibodies) to the components of the blood coagulation system is possible. This condition is called antiphospholipid syndrome and is dangerous for the development of various thrombotic complications (vein thrombosis, heart attack, stroke). The presence of these manifestations in a patient at a young age requires the exclusion of SLE and antiphospholipid syndrome.
Nonspecific complaints. Many patients at the onset of the disease notice only nonspecific symptoms of the disease, such as general weakness, increased body temperature, weight loss, and lack of appetite.
Forecast
In chronic discoid LE, the prognosis is generally favorable. An adequate treatment regimen must be developed to induce long periods of remission (when symptoms subside). But in some cases, the cutaneous form of lupus becomes systemic. And this is already a serious illness with serious complications. Often this transition is preceded by a violation of certain prohibitions: prolonged exposure to the sun, treatment with sulfonamide medications and streptomycin, hypothermia and other factors that should be avoided.
The patient must be under constant medical supervision, clinical and laboratory tests are carried out in order to detect degeneration into a systemic process in time. It is important to monitor the function and condition of the urinary organs, heart, and respiratory system. The functioning of these organs directly affects the prognosis of discoid lupus erythematosus.