According to WHO, endocrine disorders are most often detected in women, if a blood test shows that TSH is elevated - does this mean that a disease is developing in the body? Detection of deviations in values from values accepted as normal may indicate a dysfunction of the endocrine glands, mental, somatic disease, tumor lesion or other pathological process.
It may also indicate lead intoxication, be a consequence of surgery, a blood purification procedure, drug poisoning, or physical overload.
When interpreting the results of a hormonal blood test, many factors are taken into account - the magnitude of the shift, the presence of concomitant clinical symptoms, and the physiological characteristics of the patient. Independent interpretation of a laboratory test will not replace a woman’s medical consultation, but will help her suspect something is wrong, not waste time and take appropriate measures.
What is TSH in a blood test?
TSH, in its chemical structure, is a representative of the family of glycoprotein hormones and belongs to the group of protein-peptide compounds. For its role in the body it is called regulating. Synthesized by the pituitary gland. Its full name is thyroid-stimulating hormone. Synonyms thyrotropin, thyrotropin are also used. Stimulates the thyroid gland. Determines the content of the main thyroid hormones in the blood: thyroxine (T4), converted into a more active form - triiodothyronine (T3).
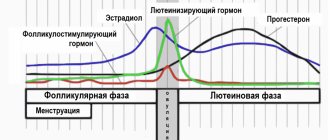
In the functioning of the pituitary gland, there is a phenomenon of interaction between TSH, T4, T3, and the feedback principle operates. It is expressed as follows: if the level of T4 decreases even slightly, the pituitary gland immediately reacts to this with a multiple increase in TSH in the blood. It, in turn, activates the thyroid gland, causing it to increase the production of vital thyroxine.
If the thyroid gland releases a lot of thyroxine, and its concentration exceeds the norm, then the excess is suppressed by inhibiting the release of TSH. Suppression of synthesis is carried out by the action of the isolated thyrotropin on the anterior lobe of the pituitary gland.
Based on this interconnected production mechanism, based on the level of thyroid-stimulating hormone in a blood test, diagnosticians and endocrinology specialists:
- judge the functional activity of the thyroid gland;
- study the production of hormones, the body’s needs for thyroxine;
- assess the quality of compensation for the condition caused by persistent hormone deficiency (primary hypothyroidism);
- determine the hormonal background of a woman - without TSH, a diagnostic examination for hormones will not be complete;
- develop diagnostic and treatment tactics;
- monitor the effectiveness of treatment
How often do you need to get tested for TSH, who and where?
TSH analysis is especially important for children and women when planning pregnancy, as well as during it. Any suspicion of hormonal disorders associated with the thyroid gland requires testing using hormone tests, including TSH.
It is imperative to monitor TSH for those who have already had problems with the thyroid gland before. According to the recommendation of the American College of Physicians, TSH testing should be done regularly for all women over 50 years of age, since this is a risk group for hormonal disorders due to the onset of hormonal changes in the body (entry into menopause).
You can get tested for TSH in almost any clinic or laboratory. However, only at LAB4U the affordable price of a TSH blood test is combined with high quality and accurate results.
Functions of thyroid-stimulating hormone in the female body
The first thing that elevated TSH means is a low concentration of triiodothyronine and thyroxine in the bloodstream. The role of thyroid-stimulating hormone is to ensure an increase in the production of T4 by the gland, which is achieved through its effect on receptors that are located on the membrane of the follicular cells of the thyroid gland. The result of this effect is an increase in iodine consumption by thyrocytes (thyroid cells), which trigger the process of synthesis and secretion of the most important regulators of differentiation of tissues, organs and systems - the hormone T4 (about 80%) and the more powerful T3 (about 20%). The effect appears within 1-2 minutes. Regulation of the biosynthesis of thyroid hormones is the main, but not the only task of thyroid-stimulating hormone.
In a woman’s body, it is also responsible for:
- quantitative change in phospholipids, nucleic acids;
- lipolytic effect (lipolysis) – enhances the breakdown of fat molecules into glycerol and fatty acids;
- production of proteins, support of energy balance;
- maintaining the normal structure of the thyroid gland (when TSH is increased, the size of the woman’s thyroid gland also changes - tissue growth, an increase in volume and a change in the contours of the thyroid gland are observed, which can be identified visually or determined by touch);
- an increase in the number and size of hormone-producing cells;
- sensitivity of hormonal receptors - prepares tissues for the action of triiodothyronine and thyroxine.
Norm T3 and T4 and interpretation of the analysis
Since the level of triiodothyronine and thyroxine is determined simultaneously with the study of TSH, and they are all interconnected, it is important to know the normal values of these two hormones.
The T3 content in the blood of an adult should be in the range from 1.08 to 3.14 nmol/l. As for thyroxine, the values for men and women are different. For men, the norm is a level from 59 to 135 nmol/l, for women the figure is slightly higher - from 71 to 142 nmol/l.
Deviations from the norm indicate existing pathologies. If T3 is elevated, the reasons may be:
- hyperthyroidism;
- thyroid adenoma;
- Pendrer's syndrome (a genetic disease characterized by vestibular disorders, bilateral hearing loss and goiter);
- chronic liver pathologies;
- choriocarcinoma;
- nephrotic syndrome.
Triiodothyronine is reduced in the following cases:
- iodine deficiency;
- hypothyroidism;
- adrenal insufficiency;
- significant physical activity;
- weight loss.
Deviations from the norm of the T4 hormone are due to the following reasons:
- increase: thyrotoxic adenoma, nephrotic syndrome, decrease in thyroxine-binding globulin;
- A decrease in the hormone is usually associated with diseases of the thyroid gland.
Test results can be indirectly influenced by factors such as severe stress and taking oral contraceptives.
Features of thyroid-stimulating hormone
When trying to independently determine what to do if the TSH test is elevated, you should take into account the normal daily variability of its level. The range of physiological fluctuations in values can be 1-3 mU/l. The highest concentration is observed late at night - at 2-4 o'clock. Then a slight decrease occurs. Thyrotropin is secreted in a pulsating manner.
The highest concentration is also observed at 6 am, and the lowest - in the period of time preceding the evening (17-19 hours). If a woman’s standard sleep-wake pattern is disrupted, the rhythm of secretion changes and a shift occurs to a later date. The circadian rhythm normally persists in old age and during pregnancy.
Individual variability (variability) of indicators, due to the use of different methods and test systems by laboratories, is of clinical importance. When interpreting the result of the study, it is important to exclude the influence of drugs that can increase the concentration of thyrotropin.
What factors affect TSH levels?
High levels of the hormone TSH – this may be due to:
- long-term iodine deficiency, defects in its absorption;
- intense physical activity, prolonged training on an exercise bike (overload can provoke a 4-fold increase in concentration);
- taking radioactive iodine;
- lead poisoning;
- use of medications, hormone therapy;
- medical actions - thyroid surgery, gallbladder removal, ECT, blood purification;
- hypocorticism;
- diseases associated with aging women, gynecological problems;
- absence of menstruation (from 6 months) in a woman of reproductive age;
- to give up smoking;
- psycho-emotional overload.
The age of a woman does not have a significant effect on thyrotropin levels - it increases slightly, and concentration peaks at night become less pronounced.
Reference range for women
This term is the most correct and correct. It replaced the concept of “TSH norm”, which cannot fully reflect all the results. Clearly defining the norm when it is necessary to take into account the influence of many factors (gender, age, race, weight, previous diseases, health status, etc.) is not an easy task. In healthy women, the content of thyrotropin varies widely.
Compared to men, women have higher TSH concentrations (approximately 20%). Some laboratories accept the range of 0.4-5.0 mIU/l as normal (this is the same as the unit of measurement mU/l), other clinics consider values in the range of 0.3-4.5 normal. In a situation where the analysis form says, for example, “TSH 4.8,” you should focus on the normal parameters that were determined and approved by the specific laboratory that conducted the blood test.
It is important to know, according to the latest data, patients whose TSH concentration in the analysis goes beyond the values of 2.5-3 are considered to be at an early stage of hypothyroidism (mild form). Such women are recommended to undergo repeated tests, because even at relatively low concentrations, various dysfunctions of the endocrine gland can manifest themselves.
Hypothyroidism: should it be treated?
This disease is associated with insufficient production of thyroid hormones. Nina Vladimirovna KUSHNIR, an endocrinologist of the highest category at the Polyclinic Research Institute of Physics and Medicine, Federal Medical and Biological Agency, spoke about how to recognize, diagnose and treat hypothyroidism (and in some cases, prevent its development).
— What is hypothyroidism and how does it manifest?
— With this disease, the thyroid gland produces insufficient amounts of thyroid hormones T3 and T4. The degree of risk of developing hypothyroidism is indicated by an increase in the level of the hormone TSH - this is the first “bell”. Since thyroid hormones are necessary for all organs, tissues and cells without exception, hypothyroidism can manifest itself in a variety of disorders, which are often very similar to other diseases.
Women are more prone to hypothyroidism (especially during the postmenopausal period); they are diagnosed with it 8–10 times more often than men. For Moscow this figure is 6–7%.
— What are the most characteristic symptoms of this disease?
— A lack of thyroid hormones leads to fluid retention in the intercellular space and a slowdown in metabolic processes, so unexplained weight gain, constipation, hair loss, swelling of the face, snoring, and deepening of the voice (due to swelling of the vocal cords) may occur. On the part of the central nervous system, these are fatigue, depression, and anxiety. From the genital area – menstrual irregularities, infertility. If any of the listed symptoms are observed, it is necessary to determine the level of the hormone TSH - its increase, as we said, may be a sign of hypothyroidism.
— What should TSH be normal?
— A TSH level of 0.4 to 4.0 mU/l is considered normal. But not everything is so simple here. If the TSH level is slightly higher than normal (i.e., from 4.0 to 10.0 mU/l), this indicator alone cannot make a diagnosis of “hypothyroidism,” and treatment in this case is not always required. First of all, the level of T3 and T4 is determined, and if these indicators are normal, then this may be subclinical hypothyroidism. In some cases, it is enough just to be observed by an endocrinologist. But if TSH is above 10.0, then treatment is necessary. It should be noted that in young women of reproductive age, TSH should be 2.5 mU/l or even lower. If your TSH level is above 4.0 mU/l, be sure to contact an endocrinologist - only he will determine the tactics for further management.
— What causes lead to hypothyroidism?
— A fairly common cause is autoimmune thyroiditis (AIT). This is a rather complex disease. For reasons that are not entirely clear, the autoimmune system malfunctions, as a result of which the production of thyroid hormones gradually decreases. To diagnose AIT, a blood test is taken to look for antibodies in the thyroid gland. Another common cause of hypothyroidism is surgery on the thyroid gland for various diseases (toxic goiter, multinodular and nodular goiter, thyroid tumors). Finally, chronic iodine deficiency can lead to serious changes in both the thyroid gland and other systems.
— Are additional studies prescribed (for example, ultrasound) or are hormonal tests sufficient?
— After a screening study (which is an analysis of the levels of the hormones TSH, T3 and T4), if necessary, an ultrasound is prescribed, which allows us to assess the structural changes and size of the thyroid gland. It is very important to understand what exactly led to the underproduction of hormones; treatment tactics will depend on this. Maybe it’s diffuse goiter (enlargement of the thyroid gland due to iodine deficiency) - then iodine supplements are prescribed, and the TSH level will return to normal. And if it is a nodular goiter, a puncture biopsy of the nodes is required to determine their cellular composition.
— Many people are afraid to perform a puncture.
— Yes, there is a persistent myth that piercing a node with a needle can supposedly provoke the growth or development of a tumor. In fact, it has been proven that if there is no oncology, then puncture does not lead to the growth of cancer cells, but is the most important diagnostic criterion: the earlier it is diagnosed, the easier it is to treat. After all, there are no markers for thyroid cancer.
Normally, the volume of the thyroid gland does not exceed 18 cm3 in women and 25 cm3 in men.
— What is the treatment for hypothyroidism, if necessary?
— Since hypothyroidism is a deficiency in the body of the hormones thyroxine (T4) and triiodothyronine (T3), treatment involves compensating for this deficiency and is called replacement therapy. Properly selected replacement therapy prevents all possible adverse consequences of thyroid hormone deficiency and allows you to lead a lifestyle that is practically no different from normal.
— What about postoperative patients?
— If we are talking about complete removal of the thyroid gland, mainly due to cancer, then hormone replacement therapy is prescribed immediately after the operation. It is important to be observed by an endocrinologist and maintain TSH levels at the lower limit of normal or even slightly lower.
— You mentioned iodine deficiency. Is it necessary to take iodine supplements to eliminate it, or is it enough to adjust the diet?
- Let's go in order. Iodine is truly the most important element in the synthesis of thyroid hormones. It is also true that Russians are in a state of severe iodine deficiency: with a daily requirement of 150 mcg of iodine, we receive no more than 80 mcg of iodine per day. We get up to 95% of iodine from products of plant and animal origin (for example, the iodine content in 1 kg of seaweed reaches 800,000 mcg) and only 3–5% from air and water.
- So you need to eat seaweed every day?
- Not at all necessary. Mass prevention, in accordance with the state program, involves the use of iodized salt. There are also group and individual prevention. Pregnant women are included in a separate group - they all take iodine supplements.
— What is subclinical hypothyroidism, which you talked about earlier?
— Subclinical hypothyroidism is characterized by elevated TSH levels (from 4.0 to 10.0 mU/l) with normal levels of T3 and T4 and without clinical manifestations. Treatment (or correction) is required in a number of cases: for example, in a young woman of reproductive age who is about to become pregnant and give birth (since low levels of thyroid hormones negatively affect the development of the fetus and the woman’s health). Treatment is also necessary for postmenopausal women, if along with increased TSH there is increased cholesterol, excess weight, diabetes, etc. - then there is no need to wait for a further increase in TSH and a decrease in T4. Although the final decision is made by the attending physician.
Subclinical hypothyroidism occurs in 10% of the population. In women of the older age group, its prevalence is 12%.
- But what if there is none of this?
- Then it’s enough just to be observed by an endocrinologist. There are cases of the so-called. transient (short-term) increase in TSH with normal T4 against the background of certain conditions - the postpartum period or subacute thyroiditis. In such cases, a follow-up examination is scheduled after three months.
— And the last question: sometimes the media advise everyone to take thyroid hormone medications after a certain age. Is it necessary and possible to do this without consulting a doctor?
— Tactics in this matter are changing. About 20 years ago in medicine it was believed that thyroid hormones were “hormones of youth”, so they were taken in small doses. And many did this. There was no harm from this, but was there any benefit? After all, if there are violations, then an adequate dosage is needed, taking into account side diseases, such as peptic ulcers, since the drugs are taken on an empty stomach. In my opinion, you cannot take any hormonal therapy without consulting an endocrinologist!
Interviewed by Maria SHCHERBAKOVA
High TSH - what does it mean?
Elevated TSH in women does not always require treatment. It is possible to diagnose a pathological process only after excluding the influence of temporary and random factors. The level of serum free T4 is also taken into account. Treatment is prescribed for elevated TSH in combination with low (suspect hypothyroidism in a woman) or high (check for hyperthyroidism) concentration of thyroxine and/or triiodothyronine.
If the level of free T4 is normal, the functions of the thyroid gland are not impaired, then repeated tests are carried out at certain intervals, incl. using other test systems.
Deviations in the TSH level to a greater extent are detected quite rarely - only in 8% of patients (men and women) the indicator exceeds the normal value of 2.5-3 mU/l. Among patients with hypothyroidism, only 24% have levels of 10 mU/L or higher. This is a pathological increase.
Such high values occur in women with serious ailments:
- a malignant tumor that arises in the cells of the thyroid gland;
- congenital anomalies of the thyroid gland;
- tumor proliferation of pituitary cells (TSH-secreting adenoma);
- hormone-secreting neoplasms (in lung tissue, glandular tissue of the mammary gland);
- hereditary insensitivity to thyroid hormones;
- severe somatic pathology in the recovery stage;
- inflammatory disease of the thyroid gland – autoimmune or subacute thyroiditis.
If the upper limit of the “norm” is not exceeded to this level, the TSH indicator is 7.5, a little less or more within the range of 5-10 mU/d - what to do in this case? You should immediately consult a doctor - only a qualified endocrinologist can find the cause of the deviation and make a diagnosis. To confirm or exclude pathology, a number of diagnostic measures will be required.
Additional diagnostics
Insufficient TSH production is more likely to lead to increased levels of thyroxine and triiodothyronine. To confirm or refute suspicions, the woman is additionally prescribed a blood test for T3 and T4 levels. The combination of tests depends on the symptoms and the degree of decrease in thyrotropin.
Frequent variations of hormonal tests and their interpretation:
- TSH is low, and T3 and T4 do not exceed the norm - subclinical hyperthyroidism. There are no pathological symptoms yet, but the content of hormones in the blood serum changes.
- TSH is critically low, and T3 and T4 are high - thyrotoxicosis with pronounced symptoms. If iodine-containing hormones are high, TSH automatically stops being produced, since its synthesis will only increase the secretory activity of the thyroid gland. Because of this, the level of thyroid hormones will become even higher.
- TSH, T3 and T4 are below normal values – a violation of the inversely proportional connection between the thyroid gland and the pituitary gland. The pituitary gland stops synthesizing TSH, which is why the secretion of iodine-containing hormones is not stimulated.
The principles of treatment of endocrine diseases in women are determined by the concentration of not only TSH, but also thyroid hormones. Therefore, if thyrotropin levels are low, patients are referred for further examination.
TSH and pregnancy
It is recommended for women to check their TSH level at the stage of planning a child. The functions of the thyroid gland are closely related to the activity of the reproductive system. For women who want to become a mother, the optimal value is in the range of 0.2-2.5 mIU/l. If the TSH value in women exceeds this figure and is at the upper limit of normal, then treatment may be required. It is prescribed by a doctor based on the results of a complete examination. To correct hormonal balance, patients may be advised to take synthetic thyroxine preparations.
If pregnancy has occurred, then it is especially important to monitor the condition of the endocrine glands. Tests are taken throughout the entire period of pregnancy, as well as after childbirth. After conception, hormonal changes begin in a woman’s body, which is expressed by an increase in the secretion of thyroid hormones and a decrease in TSH levels (when twins or triplets are expected, the TSH level tends to zero). In the middle or end of the term, the indicator may return to normal values.
If these physiological mechanisms are disrupted and thyrotropin concentrations remain high in the first trimester, then urgent action will be required to avoid adverse consequences. What to do if a pregnant woman has elevated TSH: a treatment plan is drawn up in accordance with the established diagnosis. Drug therapy usually includes drugs containing levothyroxine sodium as the active substance.
What can affect the results of a TSH test?
The level of the TSH hormone can vary due to the influence of various external or internal factors on the body. This is especially true for the time of day. The maximum concentration is observed at night (from 2 to 4 am and from 6 to 8 am), and the minimum is from 5 to 7 pm. In the absence of proper sleep at night, hormonal synthesis is disrupted. In addition, a decrease in TSH can become a symptom of pregnancy and breastfeeding, which is regarded as a variant of the norm. Some medications may also cause changes in TSH concentrations. The thyroid gland is closely related to other internal organs, so disruption of their functioning significantly affects hormonal production. In middle-aged women and elderly men, the maximum value of thyroid-stimulating hormone is detected in December. During menopause, an increase in TSH is allowed in the absence of signs of an increase in the size of the thyroid gland.
Symptoms of elevated TSH
In most cases, the development of the pathological process can be recognized by characteristic signs. High thyrotropin makes itself felt:
- lack of vigor and energy;
- rapid fatigue;
- excessive sleepiness;
- deterioration of memory, intelligence;
- weight gain due to poor appetite;
- obsessive feeling of cold;
- swelling;
- sensation of crawling goosebumps;
- dry skin;
- deepening of a woman's voice;
- brittleness, splitting of nails;
- deterioration of hair condition, excessive hair loss.
The following symptoms will indicate that a woman has elevated TSH and T4 at the same time:
- noticeable enlargement of the thyroid gland;
- increased heat generation, sweating;
- eating large amounts of food, but experiencing weight loss;
- disorder of the myocardium, vascular system, high pulse;
- vomiting, diarrhea, discomfort in the abdomen, solar plexus;
- thinning hair, premature appearance of gray hair;
- irritability, anxiety, instability of attention;
- menstrual irregularities;
- decreased muscle tone, general weakness.
Reasons for low TSH
A decrease in hormone levels is observed:
- with diffuse toxic goiter;
- thyrotoxic adenoma;
- postpartum necrosis of the pituitary gland;
- latent thyrotoxicosis;
- pituitary injuries;
- nervous breakdown or starvation due to diet;
- attempts to independently regulate the amount of T4 and the subsequent development of thyrotoxicosis.
A drop in TSH levels can be observed in pregnant women with hypothyroidism.
Changes in the direction of decreasing hormone levels occur when using certain medications. The list includes anabolic steroids, glucocorticosteroids, cytostatics, antihypertensive medications and other drugs.
When is the test ordered?
A local physician, general practitioner, gynecologist, or endocrinologist can issue a referral for a blood test.
The indication is:
- detection of alarming symptoms;
- suspicion of deterioration in the functional state of the gland or cancer;
- the onset of pregnancy;
- monitoring the effectiveness of therapy.
In clinically asymptomatic women, hormonal blood tests to detect the disease are recommended every 5 years after reaching 35 years of age. Patients diagnosed with hyperthyroidism or hypothyroidism - congenital or acquired - are examined annually throughout their lives.
Preparing for a hormone test
The amount of hormones in the blood depends on the time of day, since there is a daily rhythm of secretion (release of hormones). Blood for hormonal analysis should be taken in the morning, on an empty stomach.
In women, hormonal levels also depend on the stage of the menstrual cycle. The most favorable days for analysis are days 5-7 of the cycle, starting from the first day of menstruation.
On the eve of the test, you should not drink alcohol, and you should also avoid increased physical activity and stressful situations. It is advisable not to smoke for an hour before the test.
A week before the test, you must stop taking hormonal medications. If you are prescribed medication, discuss this with your doctor; the test may have to be postponed.
Donating blood for TSH hormone
This is a laboratory test. Conducted in standard mode. It involves examining biomaterial taken from the patient using specialized equipment. Each medical laboratory has its own methodology, equipment, reagents, rating scales, which causes some discrepancies in measurement results. This is important to consider when visiting different clinics.
Repeated annual checks are recommended to be done in the same institution and at the same time, because daily and seasonal fluctuations in thyrotropin levels are possible. Its concentration in the blood can be determined as part of a separate study or as part of a set of tests. In laboratory diagnostics, chemiluminescent immunoassay is used to determine TSH.
Material for research
The biomaterial is blood serum. Hemolysis and lipemia may affect the test result. A woman's blood sample is obtained from a vein (forearm, cubital fossa). When drawing blood, the patient sits or lies. Venous blood collection is the simplest invasive procedure. The laboratory technician treats the injection site with a disinfectant. A tourniquet is applied to restrict blood circulation.
How do you prepare for the procedure?
It is advisable to collect blood in the morning.
Preparatory activities include:
- Exception on the eve of the examination of physical procedures and other methods of examination - X-ray, X-ray fluorography, ultrasound.
- Refusal to use hormone-containing drugs (7 days before) and medications containing iodine (3 days before). The exact timing of abstinence and the names of medications must be agreed upon with your doctor in advance.
- Avoiding alcohol consumption, stressful situations, overheating, hypothermia, minimizing emotional stress, physical activity (1 day).
- Limiting fatty foods, fried foods, not exercising (1 day).
- Elimination of any food before the session, pure non-carbonated water is allowed (the procedure is carried out on an empty stomach).
- Abstinence from smoking, keeping calm (1 hour).
Period of execution
The urgency of the analysis depends on the specific laboratory and its capabilities. After collecting the material, the study can be carried out independently or samples can be sent for analysis to another institution. In most cases, the result in the form of a special table on a laboratory form (indicating reference values) can be obtained on the same or the next day. By agreement with the contractor, the result can be sent by email.
How to decrypt
Specialists from a medical institution help to correctly interpret the final result, but for a more accurate interpretation, you will need to consult with the attending physician, who has all the necessary information about the internal picture of the disease, the woman’s health status, her physiological characteristics, and the presence of concomitant diseases.
How to prepare?
A little preparation is required before taking laboratory tests:
- Blood should be donated in the morning (from 8 to 10) on an empty stomach. The last meal is no later than 12 hours before the procedure.
- The day before, cancel physical activity, give up alcohol and smoking.
- It is advisable to come to the laboratory in a calm psycho-emotional state, without hypothermia or overheating.
- During the first examination, you need to stop all medications that affect the functioning of the thyroid gland two to four weeks before the procedure.
- During a control analysis carried out to assess the effectiveness of treatment, stop taking medications on the day of the study.
- Report the use of corticosteroids, aspirin, tranquilizers, and oral contraceptives.
Treatment of elevated TSH
If thyroid-stimulating hormone is elevated, the first thing a woman needs to do is visit an endocrinologist. The interpretation of blood parameters, the search for the cause of increased levels, and the determination of treatment strategies should be carried out by a qualified specialist.
He will conduct a thorough examination, and, if necessary, prescribe a repeat analysis and other specialized tests and samples, which together allow us to assess the functional state of the hypothalamic-pituitary-thyroid system, which works on the principle of feedback. To bring the hormone back to normal, treatment requires predominantly conservative comprehensive treatment.
Drug therapy
The main effective direction of treatment is the method of therapy using hormonal drugs. A concentrated extract from the pituitary gland of cattle can be used as a medicine for elevated TSH. The drug Thyrotropin made on its basis is administered by injection, strictly according to indications, the course is 5-7 days. Several courses are held throughout the year.
But more often correction is carried out with synthetic thyroid hormones. Hormonal and replacement drugs include Levothyroxine, L-Thyroxine, Thyroidin, Euthyrox, Thyreocomb, Thyreotom, etc. Some women are wary of hormone replacement therapy regimens, citing side effects and changes in hormonal levels.
You should know that the dosage of medications is optimal and individual, selected by the doctor for each individual woman, taking into account the results of the examination and the clinical picture. The duration of the course is minimal.
ethnoscience
Using alternative therapy methods by independently selecting recipes is dangerous to health and is fraught with aggravation of pathological changes. With the approval of the attending physician, traditional medicine recipes can only be used as general tonics and as a way to eliminate unpleasant symptoms. Most often, decoctions and infusions are prepared from medicinal plants (St. John's wort, licorice root, rowan fruits, rose hips, yarrow, coltsfoot flowers). To cover the lack of iodine, they resort to consuming kelp (sea kale), products derived from spirulina.
Diet and healthy lifestyle
For women with elevated TSH hormone, a therapeutic diet has been developed, which implies a complete, balanced diet. A sufficient content of fiber, proteins, and fats must be ensured (due to fatty fish, goat's milk, eggs, and fish oil).
Products containing this important element in large quantities will help compensate for the lack of iodine. Such as:
- products of marine origin (algae, fish, seafood, caviar);
- persimmon and black currant;
- organic cheese;
- chicken breast;
- milk products;
- buckwheat.
You should exclude from your diet foods that block the absorption of iodine - these are radishes, turnips, soybeans, cauliflower and red cabbage. Coffee, strongly brewed tea, chocolate and spices are harmful, because... they are stimulating. It is equally important to organize the correct drinking regime - drink enough clean water. You also need to change your daily behavior: ensure psycho-emotional comfort, avoid conflicts, overload, give up cigarettes and alcohol.
How to normalize TSH levels
Before increasing TSH, the cause of pituitary dysfunction is determined. Depending on this, the doctor selects the optimal treatment methods:
- Hyperthyroidism. Conservative therapy is aimed at reducing the production of thyroid hormones. Therefore, women are prescribed antithyroid drugs - Tyrosol, Mercazolil, Propylthiouracil, etc. They accumulate in glandular tissue and inhibit the secretory activity of its cells. Due to this, the level of T3 and T4 decreases.
- Thyrotoxic adenoma. In 90% of cases, women undergo surgical treatment. The scope of surgical intervention is determined by the size of the adenoma and its location. If possible, women undergo organ-conserving surgery, in which only the nodes are removed. If there are contraindications to surgery, radiotherapy is used.
- Hashimoto's thyroiditis. There is no specific treatment for the disease, so women undergo hormone replacement therapy with levothyroxine. If patients simultaneously experience inflammation of the gland, glucocorticosteroids and non-narcotic analgesics are prescribed - Prednisolone, Diclofenac, Indomethacin, etc.
All women, without exception, are given a dietary program, since good nutrition improves the functioning of the thyroid gland and pituitary gland.
Why is an increase in TSH dangerous?
An increase in thyrotropin secretion is observed relatively rarely; it manifests itself as hypothyroidism or thyrotoxicosis. Symptoms usually progress quickly. High concentrations of thyrotropin in women often cause infertility, difficulties with conception, spontaneous abortion in the early stages, severe toxicosis, bleeding, fetal hypoxia, developmental delay and even fetal death. The consequence of high TSH can also be problems with the heart, vision, mucous edema, thyrotoxic crisis, atherosclerosis, and disruptions in the functioning of the central nervous system. Without medical care, a woman's quality of life can seriously deteriorate.
With timely, competent treatment and strict adherence to all medical recommendations, the prognosis is generally favorable.