Causes of cervical disease
The causes of cervical diseases are:
- injuries occurring after abortion or childbirth;
- infections (mycolasma, chlamydia, trichomonas, cocci, etc.) causing inflammation and increased desquamation of the epithelium;
- viruses, which include papilloma, which can in some cases cause cervical cancer;
- disruption of hormonal balance (mainly progesterone deficiency);
- weakening of the immune system, which plays an important role in tissue repair;
- early sexual life, frequent change of sexual partners.
I. BACKGROUND PROCESSES
- Hyperplastic processes associated with hormonal disorders:
- a) endocervicosis (simple, proliferating);
- b) polyp (simple, proliferating, epidermal);
- c) papillomas;
- d) leukoplakia (without atypia);
- d) endometriosis.
- Inflammation:
- a) true erosion;
- b) cervicitis.
- Post-traumatic processes:
- a) ruptures;
- b) ectropion;
- c) scar changes;
- d) cervicovaginal fistulas.
Symptoms
Symptoms of diseases of the reproductive system organ - the cervix:
- In inflammatory diseases, mucous and purulent discharge from the vagina, fever, and pain in the lower abdomen, especially upon palpation, appear. In many cases, the disease occurs without symptoms, which increases the risk of complications.
- With underlying diseases, there are no symptoms or slight mucous discharge from the genital tract.
- Precancerous diseases are characterized by the occurrence of profuse, watery, white and bloody discharge after sexual intercourse.
- With cervical cancer at an early stage, bloody discharge from the genitals is observed, especially after sexual intercourse. In the later stages, pain in the legs and back, blood in the urine, weight loss, and swelling of the legs are noted.
The most common diseases of the cervix
Cervical diseases are characterized by a conditional division into background, precancerous diseases and cervical cancer.
Background diseases:
- dyshormonal processes: ectopia, polyps, benign transformation zone, papillomas, endometriosis;
- post-traumatic processes: rupture or scar changes in the cervix, ectropion, cervicovaginal fistulas;
- inflammatory processes: cervicitis, erosion.
Precancerous diseases:
- dysplasia: papillary and precancerous transformation zones, simple leukoplakia, condylomas, precancerous polyps;
- leukoplakia with cell atypia;
- adenomatosis;
- erythroplakia.
Cervical cancer:
- preclinical forms: proliferating leukoplakia, fields of atypical epithelium, papillary zone of transformation, zones of atypical transformation and vascularization, intraepithelial cancer, microcarcinoma;
- clinical forms of cancer: exophytic and endophytic, mixed.
The cervix is most susceptible to the following common diseases:
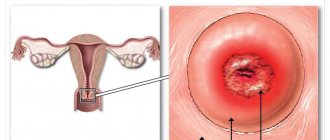
- Erosion. The cervix is damaged and a bright red wound forms on it, which can be detected by a gynecologist during examination. The causes of erosion are inflammatory processes, physical or chemical influences, as well as hormonal imbalances. Erosion heals if the cause of its occurrence is eliminated, but if healing does not occur, then it turns into pseudo-erosion.
- Pseudo-erosion. It is an unhealed erosion, as a result of which the cervix is subject to the appearance of nabothian cysts.
- Nabothian cysts. These are bubbles filled with liquid that are located under the mucous membrane. In most cases, if the cause of erosion is eliminated, a complete cure occurs. However, with prolonged treatment of erosion, the processes that occur in the cells of the superficial layer of the cervix change and can lead to the development of dysplasia.
- Leukoplakia. It is a compaction in the form of a white spot. This disease develops from erosion.
- Polyps. The cervix undergoes the formation of outgrowths, the development of which is caused by inflammatory or hormonal processes.
- Flat condylomas. This is a manifestation of the human papillomavirus. Dysplasia can develop within flat condylomas, which characterizes them as a precancerous condition.
- Dysplasia. This disease cannot be seen with the naked eye; it is determined only through special studies.
Types of diseases and their symptoms
Ectopia
Ectopia is the displacement of the columnar epithelium onto the vaginal part of the cervix. It can be acquired or congenital (previously it was called pseudo-erosion). Hormonal, inflammatory and mechanical factors can trigger the onset of this disease.
In the presence of an inflammatory process, the stratified epithelium becomes loose, the layers are not reliably connected to each other. When subjected to mechanical stress, it is damaged and desquamated. The infection creates a general dyshormonal background, in which columnar epithelium is formed from reserve cells. In the presence of a disturbed menstrual cycle, the likelihood of ectopia increases by 5-6 times.
Symptoms: pain, bleeding. With this type of cervical disease, the following characteristic features are observed during diagnosis:
- examination - the presence of a bright red, irregularly shaped area on the lip of the cervix;
- colposcopy – round/oblong red papillae are visible in areas (they make the mucous membrane seem velvety), “transformation zones” can also be observed, in which the process of cell replacement is visible;
- histology - allows us to distinguish 3 types of ectopia: congenital glandular, congenital papillary, ectopia with squamous metaplasia.
Treatment is prescribed on an individual basis depending on the severity of the disease. In mild forms - observation with regular colposcopy and cytology, in more serious forms - cryodestruction, diathermoelectroconization, laser coagulation, surgitron, solkovagin.
From the point of view of histogenesis, the congenital form is considered the norm. Its appearance is explained by hormonal effects on the fetus during pregnancy. 50% of newborns have ectopic columnar epithelium, which resolves after completion of the maturation process due to the natural migration of the epithelial boundaries.
Ectropion
Ectropion is a disease in which the mucous membrane of the cervical canal everts onto the vaginal part due to tears in the muscle fibers of the cervix. In fact, it is a combination of scar deformation with pseudo-erosion. The disease can be congenital or acquired.
Acquired ectropion occurs after childbirth, abortion, diagnostic curettage of the uterine mucosa. The disease acquires pronounced symptoms only after the addition of inflammatory processes or precancerous diseases of the cervix. In this case, leucorrhoea, pain in the lower abdomen, spotting, and cycle disruption appear. Diagnosis is carried out using:
- examination - a deformed neck, a gaping or slit-like external pharynx, red areas of columnar epithelium are visible;
- colposcopy;
- cytological and morphological examination.
Treatment is selected individually depending on the degree of deformation, age and the ability to have children. In case of minor damage or congenitality, electrocoagulation, laser vaporization, cryodestruction, diathermoelectroconization, and radiosurgery are used. If the lesion is significant, conization and excision are performed.
Leukoplakia of the cervix
With leukoplakia, the stratified squamous epithelium becomes keratinized. Keratinization has three degrees of severity - parakeratosis, hyperkeratosis and acanthosis. There are two types of leukoplakia:
- simple;
- proliferating with cell atypia - precancerous disease of the cervix, classification depends on the degree of atypia.
The disease is provoked by immune factors, endocrine factors, infections, and injuries. It can be detected in several diagnostic ways:
- upon examination, clinically pronounced forms are not always visible; white plaques in the ectocervix, rising above the surface, may be observed;
- colposcopically - the presence of a film with a smooth or bumpy surface, whitish in color, red dots and lines (blood vessels) are observed;
- cytologically – it is not possible to differentiate simple and atypical leukoplakia;
- cervical biopsy with histological examination is an effective method of differential diagnosis.
Treatment is selected individually, the doctor evaluates reproductive functions, age, and size of the leukoplakia area. The preferred methods are diathermo-electroconization and radiosurgical conization followed by biopsy of the removed piece. If a woman wants to give birth in the future, in order to avoid scars, laser vaporization, cryodestruction, and radiosurgery are used.
Erythroplakia
Erythroplakia is a disease in which the stratified epithelium locally becomes thinner and only a few layers are preserved (intermediate cells disappear). At the same time, the adjacent areas of the ectocervix retain normal epithelium. The disease occurs extremely rarely, and the causes have not yet been precisely studied. It is believed that it can occur against the background of HPV. There may be periods of remission, after which inflammation resumes. Erythroplakia is prone to malignancy. Sufficient treatment is considered to be elimination of the source of origin using cryodestruction, conization and diathermocoagulation.
Polyps of the cervical canal mucosa
Polyps are growths of connective tissue covered with epithelium. There are two types:
- glandular - growths are covered with single-row cylindrical epithelium;
- epidermised - covered with multilayered epithelium.
Polyps are bright pink, leaf-shaped or oblong in shape and hang from the external pharynx. For correct diagnosis, it is important to distinguish them from endometrial polyps. For this purpose, polypectomy is performed under the control of hysterocervicoscopy.
Diagnosis is made using ultrasound equipment. The NEARMEDIC clinic has modern devices of the latest generation, which make it possible to detect even small polyps that have not yet gone beyond the boundaries of the external pharynx. Treatment is done with polypectomy. The stalk of the polyp is carefully removed during the operation. The second treatment option is coagulation under endoscopic control.
Examination of the cervix at the Diagnostics MC
Medical suggests that all women undergo an examination of such an important organ of the reproductive system as the cervix. We offer three diagnostic methods:
- A smear is the easiest, painless and informative method, which is recommended for every woman to perform once a year.
- Colposcopy is a study of the structure of the epithelium under a colposcope. During the examination, the cervix is treated with dyeing solutions in order to identify existing pathology. The procedure is painless, since the colcoscope allows you to assess the condition of the organ from a distance.
- Biopsy is the most informative method, in which a small infected area of epithelium is taken for histological examination.
It should be noted that timely detection of the disease depends on correct diagnosis. In the early stages, the disease can be completely cured, so every woman needs a preventive examination by a gynecologist.
Stop precancer!
What is precancer and how to stop it?
It is this question that sooner or later appears in the mind of a person who monitors his health and cares about its preservation. Precancer is a pathological condition of tissue that has a high risk of developing into a malignant tumor. For many tumors, these conditions are unknown, which means that diagnosing and fighting precancer is extremely difficult. Scientists and clinicians today know a lot about such a part of the female body as the cervix. Cervical dysplasia is a precancerous condition in which abnormal cell growth occurs on the surface of the lining of the cervix or inside the cervical canal, located between the uterus and vagina. This condition is also called cervical intraepithelial neoplasia (CIN). Cervical dysplasia most often occurs in women under the age of 50, but, unfortunately, can develop at any age. Cervical dysplasia usually causes no symptoms and is most often detected by a routine Pap test, which looks for the presence of abnormal cells from the cervix.
There are 3 degrees of severity of cervical dysplasia.
Mild dysplasia sometimes resolves on its own without additional treatment, requiring only close monitoring with Pap smears every three to six months.
Changes that manifest as moderate to severe cervical dysplasia or mild cervical dysplasia that persists for two years—these conditions usually require aggressive treatment to remove abnormal cells and reduce the risk of cervical cancer. For women with cervical dysplasia who receive appropriate monitoring and treatment, there is a clearly favorable prognosis for recovery. Unfortunately, patients who are not adequately and promptly diagnosed or who do not receive appropriate treatment are at higher risk of developing cervical cancer.
Causes of cervical dysplasia
Many women with cervical dysplasia have human papillomavirus (HPV) in the cells of this organ.
HPV infection is common in women and men and most actively affects sexually active women under 20 years of age. In most cases, the immune system suppresses HPV and helps clear it from the body. However, in some women the infection persists and leads to cervical dysplasia. Of the more than 100 different strains of HPV, more than one-third can be transmitted sexually, and two specific types—HPV 16 and HPV 18—are strongly associated with cervical cancer. HPV is usually transmitted from person to person during sexual contact, such as vaginal, anal or oral sex. But it can also be transmitted in some cases through skin-to-skin contact with an infected person. Among women with chronic HPV infection, smokers are twice as likely to develop severe cervical dysplasia because smoking suppresses the immune system. Although a Pap smear alone can detect mild, moderate, or severe cervical dysplasia, additional tests are often necessary to determine the existing condition and follow-up monitoring and treatment.
These include the following:
- Repeat Pap smears
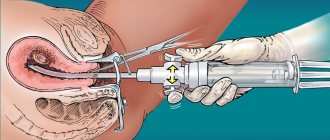
- Colposcopy, an examination of the cervix under magnification (to detect abnormal cells so that a tissue biopsy can be taken)
- Endocervical curettage – obtaining tissue from the cervical canal – also to detect abnormal cells
- electrosurgical excision procedure (LEEP), which is performed to exclude invasive cancer. During LEEP, the doctor cuts out the abnormal tissue using a thin, low-voltage electrical loop of wire.
- HPV DNA test that can identify oncogenic strains of HPV.
Treatment of cervical dysplasia
Treatment for cervical dysplasia depends on many different factors, including the severity of existing tissue changes and the age of the patient.
For mild cervical dysplasia, only continuous monitoring with repeat Pap smears is often necessary. In other cases, electroconization or excision of the cervix (removal of affected tissue using an electrosurgical loop) is used; laser, radio wave or cryosurgical treatment is also possible. A modern method of treating cervical precancer is photodynamic therapy (PDT). This is a therapy that uses a drug called a photosensitizer and a certain type of light. When exposed to light of a certain wavelength, photosensitizers produce certain forms of oxygen that promote the death of precancerous cells. At the same time, unchanged cells within healthy tissues remain preserved.
Photodynamic therapy is performed on an outpatient basis and is a minimally invasive procedure, which allows patients to preserve the cervix, including for future reproductive function. Minimal impact on healthy tissue, significant reduction in long-term morbidity, absence of insensitivity to therapy, and good cosmetic effects make this type of treatment a valuable therapeutic option for patients of any age. Contact your gynecologist about diagnosing the condition of the cervix and, if necessary, choosing the optimal method of treating it. Be healthy!
Methods and methods of treatment
Modern medicine offers various methods of treating diseases of the reproductive system. First, it is necessary to identify the cause of the disease and, if possible, eliminate it. For this purpose, treatment of inflammatory processes and hormonal imbalances is carried out, and, if necessary, treatment against viruses and immunological disorders. But sometimes such measures are not enough to eliminate the disease.
MC "Diagnostics" provides the following methods of treating an organ such as the cervix:
- Chemical removal - used for superficial tissue damage and the formation of condylomas.
- Diathermocoagulation is contraindicated in nulliparous women, as it causes scarring.
- Cryotherapy (treatment with liquid nitrogen) - used for superficial tissue damage and the formation of condylomas. Does not leave scars and is painless.
- Laser therapy – removes tissue and stops bleeding. It has increased efficiency, does not leave scars, and is painless.
- Radio wave surgery – cuts off the damaged area, is safe and painless, removes tissue and stops bleeding.
- Excision of the cervix is performed for malignant tumors.
Pathogenesis
The pathogenesis of cancerous, precancerous and background diseases is different and depends on what type of epithelium was damaged and what cells were involved in the process.
To better understand the symptoms and characteristics of your disease, as well as the principles and direction of treatment, you should learn more about the structure of the cervix. The cervix is covered with 2 types of epithelium:
- multilayer flat – vaginal part;
- single-core cylindrical - cervical canal.
In addition to the epithelium, the structure includes the stroma (the tissue of the cervix itself) and the basement membrane, which separates the epithelial cells from the stroma and consists of collagen, reticulin, argyrophilic fibers and neutral mucopolysaccharides.
Multilayer epithelium contains several types of cells, different in shape, nucleus, functionality and other parameters. They are folded in several layers:
- basal;
- parabasal;
- intermediate;
- surface.
The structure of stratified squamous epithelium and glycogen storage activity change with age because they depend on estrogen production. A greater number of layers and a maximum amount of glycogen are observed during reproductive age, the lowest in girls in the neutral period and in postmenopausal women. In postmenopause, only the basal and parabasal layers are preserved, and this is a normal variant.
The columnar epithelium that lines the cervical canal consists of only one row of columnar cells. These cells produce mucopolysaccharides, which are involved in the formation of a mucus plug in the cervical canal.
The cause of this or that deviation is a displacement of the epithelial border to the vaginal portion of the cervix, eversion of the mucous membrane of the cervical canal to the vaginal side, keratinization of multilayered squamous epithelium, its atrophy and reduction in the number of layers, the appearance of outgrowths from connective tissue, impaired cell differentiation and other processes.
The epithelial boundary in this case plays a key role - 90% of all pathologies of the cervix occur precisely there. The unspoken name for this border is the “zone of storms.” Its displacement, as indicated above, indicates the presence of pathologies. During the diagnostic process, the woman’s age should be taken into account, since as she grows older, the “storm zone” changes its location:
- in girls and adolescents - around the external os on the vaginal portion of the cervix;
- in adult women - in the area of the external pharynx;
- in postmenopause - in the cervical canal at different levels.
Rehabilitation period
The rehabilitation period depends on the type and stage of the disease, as well as on the method of its treatment. For example, with laser therapy for erosion it lasts 5-7 days. During this time, tissue rejection and wound healing on the surface occurs. The woman should stay at home, but visit a gynecologist to monitor the healing process.
During the rehabilitation period, minor pain in the lower abdomen and streaks of blood in the discharge may occur 7-10 days after the erosion has been removed. Complete tissue restoration occurs after one to one and a half months.
Contact us to sign up for an examination using the contacts listed on the website.
Principles of treatment
Treatment of established precancerous changes involves removal of pathologically altered tissue. Depending on the degree of change, gentle techniques (cauterization, laser treatment, etc.) and radical operations, including removal of the uterus, can be used.
After removal of the altered tissues, treatment is selected based on the root cause of the disease. This could be antiviral or antibacterial therapy, or taking hormonal drugs. Additionally, immunomodulatory and anti-inflammatory drugs and agents that normalize the vaginal microflora are prescribed. After treatment, the woman must be constantly monitored by a gynecologist. Cases of recurrence of precancerous changes are rare, but they cannot be completely excluded.
Most importantly, it is necessary to conduct regular examinations with a gynecologist. Our clinic has all the necessary methods for timely detection of pathologies of the female reproductive system. The examination can be carried out according to the programs “Women’s Health”, “Oncology Search in Gynecology” and others, which are prescribed by the doctor after the examination.
Timely prevention and early diagnosis prevent the development of oncological processes.