Protrusion of intervertebral discs is a physiological pathology consisting in bulging of the disc without compromising the integrity of the fibrous ring. Often occurs against the background of osteochondrosis. A healthy ring does not extend beyond the boundaries of the disc, but as this disease develops, it begins to bulge. Treatment of protrusion must begin immediately after detection. According to statistics, I diagnose it more often than a hernia.
Localization of the disease is the lumbar, cervical and thoracic regions. That is, the most mobile parts of the spine. Without treatment, the protrusion develops into a hernia, which can interfere with quality of life and seriously reduce a person's ability to work.
Prevalence of the disease
Statistics show that protrusion is a fairly common disease, especially in people over thirty years of age. Half of the documented evidence of the disease is that the most common type of protrusion is localized in the lower back. It occurs less often in the thoracic region. It is extremely rarely diagnosed in the cervical region.
Often, hernias develop from protrusions of intervertebral discs, for this reason it is necessary to undergo timely examinations and monitor your health.
Which doctor treats disc protrusion?
Since back pain can come not only from intervertebral discs, it is necessary to be examined by several doctors:
- Neurologist - seen in peripheral clinics;
- Urologist – if spinal diseases are excluded, this specialist will help determine the origin of the pain;
- A vertebrologist is a narrow specialist who specializes in the condition of the spine; appointments are carried out only in specialized medical institutions;
- Orthopedist, cardiologist, rheumatologist, pulmonologist, gastroenterologist - when there is a suspicion that the pain is of a projection nature.
Causes
Protrusion does not develop out of nowhere; first of all, stable morphological and pathological changes in the column occur, which can last up to several years. Other deformities of the spine and intervertebral discs lead to protrusion.
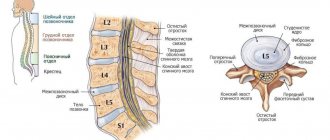
The disc consists of a fibrous ring and its immediate center, the nucleus pulposus. The core surrounded by a ring is protected. However, under the influence of various circumstances, the tissue of the ring can be damaged and suffer from micro-tears. This gives rise to the development of the disease.
Then the following happens: the vertebrae put pressure on the core, so it, avoiding this pressure, begins to slowly shift into the newly formed micro-tears. The center begins to produce additional resistance to the periphery, which subsequently leads to protrusion of the intervertebral disc. Treatment for bulging discs involves pushing the annulus fibrosus back into place before it ruptures.
| Factors provoking the development of protrusion | Factors provoking the development of protrusion |
| Microtraumas; extra load; displacement of some vertebrae; poor nutrition; fractures and injuries of the spine; curvature; weak, untrained muscles; frequent sitting work; low physical activity; genetic predisposition. | High degree of obesity, flat feet, osteoporosis, curvature (severe), osteochondrosis, changes in the quality of health with age. |
Why does protrusion develop?
Previously, it was believed that age was the main risk factor for the occurrence of protrusion, but it is now noted that the disease can also affect a young body.
The following main factors lead to the development of protrusion:
- Incorrect posture;
- Back injuries;
- Obesity;
- Heavy heredity;
- Underdevelopment of body muscles;
- Metabolism deficiencies;
- Severe infectious diseases;
- High loads on the back (sports can also have negative consequences);
- Physical inactivity.
Symptoms
The pathology develops and lasts for a long time due to the influence of provoking factors and risk factors, sometimes it can last for decades. For this reason, at first the patient may not notice the disease.
The protrusion forms and progresses without any obvious symptoms. Since people do not know about the pathology, they do not seek treatment. And the ring begins to protrude more and more until it ruptures and forms a hernia. But what is happening still has a clinical manifestation. Among the characteristic symptoms are the following:
- numbness of the limbs;
- tension in the spine;
- headache;
- discomfort in the spine;
- sleep problems;
- fast fatiguability;
- chronic pain in the spine;
- chilliness of the limbs;
- movements are limited.
These signs must be carefully monitored in order to begin treatment on time. If you notice that new symptoms have appeared or old ones have begun to develop in strength, do not delay in contacting a doctor.
Advantages of the clinic
The Health Energy Clinic works so that every patient can receive qualified medical care in the shortest possible time at an affordable price. At your service:
- experienced and skilled medical personnel who regularly improve their knowledge;
- the opportunity to get advice from foreign experts (via the Internet);
- modern diagnostic equipment;
- all types of laboratory tests;
- medicinal and surgical treatment methods, physiotherapy, massage, exercise therapy, chiropractor services;
- individual approach to the selection of therapy;
- organization of sanatorium-resort treatment;
- procedures in a day hospital;
- assistance in hospitalization in other hospitals in the city;
- issuing the necessary certificates, conclusions and certificates of incapacity for work.
Disc protrusion seems like a minor problem compared to other diseases, but it can cause severe pain and unpleasant disorders. Do not bring the disease to its extreme stage, get diagnosed and treated at Health Energy.
Degree of progression of protrusion
Conventionally, the degree of neglect of the disease can be conditionally attributed to one of three stages. Depending on how long the disease has progressed, treatment and rehabilitation are prescribed. Let's look at each of the stages.
First stage
At this stage, the fibrous ring, which is the shock absorption of the spine, begins to suffer from disturbances in its structure: cracks may form, the shape of the core may change, and so on. Patients with mild protrusion can be treated quickly and without further consequences.
Second phase
After this, the ring continues to deform. The core begins to protrude to a distance of approximately 3-4 millimeters. This leads to pressure on blood vessels and nerve endings that lie nearby. Patients at the second stage complain of lumbago in the spine and developing pain in the area where the ring was deformed.
Third stage
If the protrusion is not treated, the disease will move to the next stage. The ring begins to protrude to a distance of at least 5 millimeters, which leads to rupture of the core. The patient develops a hernia as a result.
What is protrusion of the lumbar spine
The lumbar spine is formed by 5 vertebrae, between which are located cartilages called intervertebral discs. They are responsible for softening the impacts of the vertebral bodies during walking and physical activity, and also provide the ability to bend, turn the body and other movements.
The lumbar intervertebral discs are the largest in the entire spine.
Intervertebral discs do not have their own blood vessels, and their nutrition is provided by the diffusion method. During walking, they are compressed by the vertebral bodies and abraded, as a result of which the joint fluid is squeezed out of them. It is immediately enriched with nutrients from the blood vessels of the vertebrae and, when the load is removed, is absorbed back into the disc, ensuring rapid regeneration of damaged layers.
Normally, the processes of disc destruction and restoration are in balance. But under the influence of age-related changes, increased physical activity, prolonged sitting or other factors, it is disrupted, which leads to the predominance of the processes of abrasion of the intervertebral discs over their regeneration. The result is the development of degenerative-dystrophic processes in this cartilaginous formation.
If the pathology is not diagnosed at this stage, it progresses and leads to disruption of the diffuse nutrition of the intervertebral disc. Gradually it loses water and the ability to regenerate. The consequence of this is a decrease in the elasticity and strength of the fibers that form the fibrous ring.
Each intervertebral disc has an internal jelly-like content - the nucleus pulposus and an outer fibrous membrane - the annulus fibrosus.
Since the pressure of the vertebrae on the discs does not disappear, compression of the nucleus pulposus leads to the fact that it puts pressure on the fibers of the fibrous ring. This leads to the appearance of microscopic breaks in them. But since the outer shell of the disc is formed by fibers intertwined in 3 directions, it can maintain its integrity for a long time. But with an increase in the number of micro-fractures, its resistance progressively decreases and sooner or later a cavity forms in the most vulnerable place in its thickness. It immediately fills with the nucleus pulposus, which leads to deformation of the shape of the disc - it protrudes outward at the site of the rupture. In such cases, intervertebral disc protrusion is diagnosed.
90% of all protrusions are found in the lumbar spine.
During protrusion, the fibrous ring still retains its integrity, since it is quite thick and collapses gradually. But if appropriate measures are not taken at this stage, under the influence of loads, layer after layer of fibers of the fibrous ring will be destroyed and ultimately it will rupture, and the nucleus pulposus will come out, which is called an intervertebral hernia. The final stage of the development of the disease is sequestration, i.e. separation of part of the nucleus pulposus, which allows the resulting fragment to move into the cavity of the spinal canal, squeezing and injuring the nerve roots and spinal cord located there, which is fraught with severe and sometimes irreversible complications.
Most often, protrusions are diagnosed in the L3-L4, L4-L5 discs.
Possible consequences
And although at first glance the disease seems imperceptible and harmless due to its mild onset and virtually asymptomatic nature, it can still cause truly terrible consequences after itself. Among them are lower back pain, disability, paralysis of the lower extremities, serious disorders of the pelvic organs (for example, the development of incontinence), and the appearance of disability. Therefore, it is so important to start treatment of disc protrusions on time.
The main danger of this pathology lies in the possibility of progression to large sizes and the formation of a hernia in the future. A small deformity will not cause discomfort, but already developed protrusion and hernia lead to the following problems:
- chronic and severe pain;
- chronic and severe pain;
- blood vessels and nerve endings are compressed in the sleeve or hole.
STAGES OF DEVELOPMENT
The degeneration process is quite long. Disc protrusion forms through several stages:
1. Stage I - changes affect up to 70% of the intervertebral structure. The disc is flattened, inelastic, and tears form in the fibrous ring. The nucleus pulposus gradually shifts to the area with the least resistance. The patient complains of local pain and mild muscle spasms.
2. Stage II - actual protrusion. The nucleus pulposus is significantly shifted, the fibrous membranes are stretched to 2-3 mm. In the area of damage there is intense pain and loss of sensitivity. The pain extends below the protrusion zone.
3. Stage III - the last before complete rupture of the fibrous ring and the formation of an intervertebral hernia. The filling of the disk protrudes greatly. The pain is intense, radiates to various parts of the body, and neurological symptoms are observed.
Kinds
Depending on the location of the protrusion, three types of protrusion are distinguished. They are most often formed in one of three sections - cervical, thoracic, lumbar. This happens because these segments of the spine are characterized by the greatest mobility.
Cervical protrusion
Despite the rarity of the formation of protrusions in the cervical spine, we must not forget about the possibility of its occurrence in you. First of all, you need to pay attention to localized pain in the neck and shoulder area. The pain in this place is usually aching and sharp. As the disease progresses, the pain begins to increase. In addition, your hands may also begin to suffer.
Often, cervical protrusion leads to numbness, tingling of the skin, a noticeable loss of sensitivity of the skin, muscle weakness, “jumping” blood pressure, problems with coordination and dizziness.
The cervical region is where the brain begins and where the main blood vessels are located that provide blood flow to the brain. Therefore, deformation of the rings in this segment can lead to really serious health problems. The first signs of this are high fatigue. The neck often begins to become numb when sitting for a long time, it is uncomfortable to lie in bed (the pillow seems uncomfortable), the head is held only with great tension in the neck. These signs should alert you, after which you should immediately consult a doctor.
There are seven vertebrae in the cervical region, separated by IVDs. The main difference between this segment of the spine and others is mobility, high mobility thanks to the discs. Therefore, neck movements are easy for us, and the head is kept quite stable without additional problems in a healthy state.
Excessive mobility can lead to wear of the intervertebral discs and the appearance of a bulge. And this leads to pinching of nerve endings, roots, and also the spinal cord.
Another factor that makes cervical protrusion the most dangerous is the severity of detection without examination. Unfortunately, it is often discovered only after the ring has ruptured. During the progression of the disease, myelopathy, one of the types of chronic damage to the spinal cord, may develop. The syndrome is characterized by an irritating effect.
The main consequences of the pathology: hearing loss, loss of vision. Reflexes may disappear, and patients suffer from invincible muscle weakness. In the worst cases, paralysis of the entire body is possible.
Thoracic protrusion
It is rare to see protrusion of the intervertebral disc in this region. This is due to the relatively low mobility of the chest and spine in this segment. But they can still form. Why is this happening?
This can occur with general pain in the spine or incorrect diagnosis of a heart attack (the symptoms are quite similar). The disease most often manifests itself in the form of neuralgia in the intercostal space with varying strength. Pain is accompanied by muscle weakness and noticeable stiffness in the chest and back.
Not only pain can become an important signal about the development of thoracic protrusion: thus, another flag should be discomfort that appears when sitting or standing. Also, an eternal, persistent feeling of fatigue in the back muscles, a negative effect on the spine in the form of irritation of local places. Unpleasant sensations in the thoracic region. The body uses these signals to tell you that the IVD is in poor condition.
Let's highlight the main symptoms of the development of pathology, which indicate the need for treatment of spinal protrusion in the thoracic region. You should never give them little importance, everything is important. So the list is like this:
- the middle of the back suffers from constant pain;
- numbness and lumbago appear in the chest and abdomen;
- intercostal pain;
- the tone of the abdominal muscles noticeably decreases;
- stiffness in the back.
This variant of the pathology becomes dangerous for the internal organs of the body. First of all, the kidneys and liver come under fire, which can lead to permanent diseases, pathologies and problems with the gastrointestinal tract. The pain can become chronic and intense.
Lumbar protrusion
The most defenseless section of the spine, which is most often susceptible to protrusion formations, is the lumbar and lumbosacral sections. This occurs due to the large number of loads on this area, the greatest amplitude in movements and mobility. With age, protrusions can only get worse. Intervertebral discs noticeably wear out over time, especially under the influence of provoking factors. In this case, the characteristic features are pain in this region, which spreads to the lower limbs and significantly complicates coordination, up to the loss of the ability to move the legs.
There are other markers that need to be considered for the possible formation of a bulge. This is tension and aching pain in the lumbar region before going to bed (the syndrome is relieved by lying down), lack of comfort in a sitting position. It is difficult for patients to spend at least a few minutes without changing their position; sitting without leaning on the back of a chair becomes difficult. These and other signs indicate deeply developed protrusions that need to be treated urgently. Don't delay this, especially if you have the following symptoms:
- pain in the central part of the lower back, which spreads horizontally and covers the entire lower part of the torso;
- there is noticeable stiffness in the affected area;
- radiculitis develops;
- the muscle frame in the legs noticeably weakens, especially in the thighs and calves;
- constant feeling of numbness in the toes;
- tingling feet;
- from time to time the process of urination is disrupted, the body’s false urge to urinate appears;
- leg reflexes noticeably decrease and disappear;
- the body is difficult to rotate along the vertical axis;
- when sitting, the lower back suffers from severe pain;
- the body reacts sharply to changing weather conditions.
In the future, lack of treatment leads to paralysis of the lower limbs. Don't delay going to the doctor.
Treatment of protrusion of the lumbar spine
If the size of the pathological disc protrusion is not critical and it does not pose a serious threat to the patient, treatment is carried out conservatively. The patient is necessarily prescribed a set of measures aimed at eliminating pain and inflammation, improving blood circulation, normalizing metabolic processes and muscle tone, as well as restoring the intervertebral disc.
Therefore, the components of conservative therapy are:
- drug therapy;
- osteopathy;
- manual therapy;
- massage;
- physiotherapy (phonophoresis, carboxytherapy, ozone therapy);
- individual sessions with a rehabilitation doctor.
Patients are strongly advised to reconsider their lifestyle and diet. If a protrusion has already formed in the lumbar region, it is recommended to avoid lifting heavy objects, but sedentary work will not contribute to recovery. Office workers, drivers, seamstresses, etc. need to get up from their workplace every hour and do a light workout. Exercises in the pool will also be useful.
You should definitely reconsider your own diet. If you are overweight, you should take measures to reduce it, as it increases the load on the lumbar discs. Nutrition should provide sufficient intake of essential minerals, vitamins and other compounds. Particular attention should be paid to fish, dairy products, vegetables, herbs, nuts, veal and poultry.
If it is impossible to avoid increased loads on the lumbar spine, you should think about the need to use an orthopedic corset.
Drug therapy
For protrusions, drug therapy is aimed at improving the patient’s condition, reducing the inflammatory process and creating favorable conditions for disc restoration and normalizing the transmission of nerve impulses. For these purposes, patients are prescribed:
- NSAIDs are medicines produced in the form of tablets, injection solutions, ointments, gels, creams that have analgesic and anti-inflammatory properties;
- corticosteroids - drugs with powerful anti-inflammatory effects, most often used in the form of injection solutions;
- muscle relaxants - medications that eliminate reflex muscle spasm, which provokes an increase in the severity of pain;
- B vitamins – improve the quality of nerve impulses;
- Vitamin D is a remedy responsible for the condition of bone tissue, as well as for higher brain functions, such as memory, memory, attention, and speech.
- chondroprotectors - help increase the rate of regeneration of cartilage tissue, but their effectiveness in protrusion has not been proven. To prevent diseases of the musculoskeletal system, we recommend Mermaids Marine Collagen to our patients;
All medications are selected strictly individually for each patient, taking into account concomitant diseases and the nature of the manifestations of lumbar protrusion.
Manual therapy
Manual therapy is of great importance in the treatment of protrusion of the lumbar spine. Using various manual methods, it is possible to restore the normal position of the vertebrae and increase the distance between them, which creates optimal conditions for the regeneration of intervertebral discs.
An experienced chiropractor, especially one who knows the Gritsenko technique, can eliminate the pressure of protrusion on the spinal roots, which leads to solving the problem of impaired sensitivity and mobility of the legs, as well as dysfunction of the pelvic organs. Special techniques allow you to eliminate increased tone and spasm of the lower back muscles, which quickly leads to a decrease and then elimination of pain.
Thanks to a course of manual therapy sessions, it is possible to significantly improve the patient’s well-being in a short time and create the best conditions for the regeneration processes in the disc.
Physiotherapy
Physiotherapeutic procedures are designed to increase the effectiveness of the treatment, reduce the severity of pain and inflammation. Depending on the characteristics of the condition, patients may be prescribed courses:
- electrophoresis;
- laser therapy;
- ultrasound therapy;
- UHF.
Holidays at balneological resorts have a positive effect on well-being. Therefore, as part of the prevention of exacerbation, patients are recommended to go annually to specialized sanatoriums and undergo a course of preventive procedures.
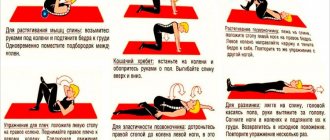
Exercise therapy
The physical therapy program for each patient is developed strictly individually by a rehabilitation physician, taking into account the size, position of the protrusion of the lumbar spine, level of physical fitness and the presence of concomitant diseases. Initially, classes are carried out under the supervision of a specialist until the patient masters the correct technique for performing the exercises. In the future, he is allowed to study at home on his own, but under no circumstances make sudden movements.
Exercise therapy classes should be carried out daily. They help normalize muscle tone and strengthen the lower back muscles, which will create adequate support for the spine.
Thus, lumbar protrusions are quite common. But to prevent them from leading to disastrous consequences, you should seek medical help when the first symptoms of the disease appear. In such cases, the prognosis is most favorable, and the progression of intervertebral disc protrusion can be completely stopped.
5 1 vote
Article rating
Diagnostics
The main obstacle and problem in diagnosing and treating spinal protrusion is the weak manifestation of the disease at the clinical level in the early stages of development. Often the patient notices the problem and seeks help already at the third stage, when the ring breaks and the formation of a hernia begins.
People who are suspected of having bulging intervertebral discs are prescribed a variety of diagnostic tests by various specialized doctors. In addition, the patient undergoes a number of additional measures to more accurately determine the disease:
- A life history is collected, which is needed to determine why the protrusion formed and the pain began to intensify;
- Inspection and further palpation of the spine (column), making it clear about the tension of the nerve roots and the position that brings more pain. At this stage, it is possible to notice low reflexes, weakness in the muscles, decreased skin sensitivity, which indicates progressive protrusion;
- An X-ray image that provides a huge amount of information about the condition of the spinal column: structural features of the vertebrae and discs, the distance between them, pathologies, signs of osteochondrosis, sustained injuries, the level of neglect of the disease;
- MRI of the spine, which makes it possible at the first stage of the disease to determine whether a person is more protrusive, as well as provide information about the size and strength of compression of the roots and tissues.
The patient is also required to undergo examination for impaired functionality and efficiency of the spinal roots and other neurological problems.
During diagnosis, it is important to distinguish the disease from osteochondrosis, radiculitis, myositis (they all have similar external symptoms with protrusion of the vertebral discs). In the thoracic region, gastritis, pancreatitis and angina must also be excluded.
Examination methods
During the first visit, the neurologist conducts an initial examination of the patient, which includes a complete history taking and special tests to assess the patient’s neurological status. A qualified specialist will be able to suspect lumbar disc protrusion based on initial monitoring of the problem. We emphasize that it is impossible to just suspect, approve and prescribe treatment without conducting instrumental diagnostics. Similar symptoms and signs of neurological deficit are typical of many central nervous system pathologies.
In order to confirm or reject this diagnosis, the neurologist refers the patient to study this department using magnetic resonance imaging. X-ray can also be used, but only as a preliminary MRI examination, since it is completely devoid of the ability to visualize soft tissues. And soft tissues are the disc itself, nerve and vascular formations, the spinal cord, and muscle-ligamentous structures.
Protrusion on MRI.
In the topic of “making a diagnosis,” it is impossible not to inform patients that taking an anamnesis, neurological tests and radiography are also of great importance. Yes, these are auxiliary methods, but they allow a specialist to:
- find out about the nature, strength, time of appearance, frequency of recurrence of disturbing ailments before a person goes to a medical institution;
- assess muscle strength, coordination, motor-support potential and identify the relationship between the increase in pain and a particular movement;
- understand what the patient’s level of physical data was before the onset of the disease and what it is now;
- identify violations of posture, measure the range of motion of the spine in all physiological directions;
- carefully examine reflexes and tactile sensitivity;
- determine the presence, size, number of osteophytes in the examined area of the ridge, shifts of the vertebrae relative to each other, the size of the intervertebral space, bone density;
- study the history of a person’s illnesses, lifestyle, professional sphere, record weight and height, take into account age, which, like everything else, plays an important role in identifying the etiology of degenerative spinal disease and in determining treatment tactics.
The process of dislocation of the nucleus pulposus, metamorphosis in the tissues of the fibrous ring, the accuracy of the location and direction of protrusion, nerve entrapment and the condition of the spinal cord can be determined purely on MRI images.
MRI allows you to collect comprehensive information down to the smallest details about the condition of all disks and other structural components at each software level. Based on cross-sectional MRI images of the area under study in the sagittal plane, even the smallest protrusions, which are less than 2 mm, are determined. After the doctor confirms the diagnosis, treatment that is adequate in the particular case and will be effective is prescribed.
Treatment
To begin with, the patient is subjected to a comprehensive examination and diagnosis of the root cause of the complaints. If a protrusion has been identified, the specialist develops a course of treatment adjusted for the characteristics of the patient’s body, the location of the pathology and its size. The most optimal option for removing a victim from protrusion is a set of measures that will prevent the nucleus pulposus from being further injured and reduce the overall pressure in the painful segment. The following specialists provide treatment:
- Physiotherapy doctor (in private situations);
- Traumatologist;
- Surgeon (in worst situations);
- Orthopedist;
- Neurologist.
Fortunately, intervertebral discs are able to return to a healthy state on their own, but to do this they need help. In this regard, the main task of treatment is to launch this mechanism, allowing the body to restore everything on its own. The methods and courses that have now been developed make it possible to stop the development of protrusion and relieve chronic pain.
The main direction in treatment is the use of non-steroidal medications. The prescribed medications help not only reduce pain, but also stop the inflammation process and help return the cartilage to its previous state. The main disadvantage of this direction is the steady development of side effects with long-term use of medications.
Other main areas of treatment are conservative treatment and surgery.
Conservative
To solve the problem of protrusion it is not necessary to go under the knife. This direction represents special measures that eliminate excess load from the disk. First of all, it is necessary to stretch the spinal region and securely fix it. This also includes a medicinal method of treatment, as it helps relieve pain, reduce swelling and inflammation of tissues.
The main advantage and advantage of conservative treatment of disc protrusion is noticeable results in a fairly short time. Patients stop complaining of pain.
The approach itself can be noted as a disadvantage. It treats the symptoms, not the root cause, which can ultimately lead to a relapse. To prolong the effect, it is necessary to be treated for a long time according to the prescribed course.
Operational
The essence of the method is surgical intervention. In fact, he is approached quite rarely; a decision to operate on protrusions requires really compelling reasons. These include:
- The protrusion is too large, it is no longer possible to pull;
- Other methods do not provide improvement for a long time;
- The location and/or size of the protrusion threatens the life of the patient and can cause irreparable harm to health.
Other situations are not considered convincing enough for the surgeon to intervene. Moreover, this method cannot deal with the cause of protrusion, only with the consequences of the course of the disease. There is a certain risk of a new protrusion forming in the future after surgery. But the percentage is lower than with surgery for intervertebral hernia.
Operation for protrusion
Let us recall that protrusion is the initial form of herniation, when the anatomical integrity of the outer sphere of the fibrous ring is preserved, due to which the nucleus pulposus is still located in the disc. Only such a picture of the disease allows the use of puncture methods of plastic disc surgery. It is advisable to recommend nucleoplasty to a person with a protrusion of the lumbar/lumbosacral location only under the following circumstances:
- ineffectiveness of non-surgical treatment for 3-6 weeks;
- frequent exacerbations of painful symptoms;
- dysfunction of the nerves of the equine ganglion;
- chronic reflex and radicular syndrome;
- rapidly progressing dynamics of protrusion development.
Puncture nucleoplasty is aimed at reducing the pressure inside the intervertebral disc, which facilitates the return of the latter to its normal shape. The effect of reducing intradiscal pressure and retracting deformation is ensured by direct impact on the core (with the goal of its partial destruction) by a certain physical factor:
- cold plasma (cold plasma plastic);
- laser (laser vaporization);
- electromagnetic waves (radiofrequency ablation);
- a pressure jet of isotonic liquid (outdated tactics, hydroplasty).
At their core, all methods of influence “work” and are carried out according to the same principle. They are also approximately equal in effectiveness - the success rate of the procedures is approximately 80%. Access to the intervertebral disc is carried out from the back percutaneously (through a puncture puncture). Anesthesia is used mainly of a local type, but in some situations general anesthesia or epidural anesthesia is not excluded. The intervention is carried out on an empty stomach, before which the patient is given a cleansing enema. The procedure is carried out in the department of minimally invasive neurosurgery, equipped with an intraoperative X-ray machine. Session duration is 15-30 minutes. Let's consider all stages of nucleoplasty.
- The patient is placed on the operating table. The classic position is on your side, with your legs tucked towards your stomach.
- The skin of the lumbar region is widely treated with antiseptics. Anesthesia is performed.
- Under X-ray control, in a safe interval, the surgeon makes a puncture (2-5 mm) with a puncture needle inserted into the disc at the required distance. Usually to the center of the core.
- An electrode is installed into the working cannula of the needle, through which the “destruction agent” of the gelatinous substance will be supplied.
- By rotating and translational movements of the electrode, emitting, for example, pulses of laser radiation or a flow of low-temperature plasma, the jelly-like component in the disk is partially evaporated.
- The denucleation performed ensures inverse retraction of the pulpous mass that has shifted to the periphery of the ring during the course of the disease. The configuration of the lumbar disc is restored, and the pinched nerve root is eliminated.
- At the end of the operation, thin working instruments are removed, and an antiseptic patch is applied to the puncture. Usually such a tiny wound does not require stitches.
During the procedure.
If the protrusion is not confirmed by MRI, and a rupture of the fibrous part of the intervertebral lining is diagnosed, the significance of nucleoplasty is completely annulled. The operation of choice for already formed lumbar hernias is microdiscectomy or endoscopy.
Separately, it is worth highlighting the fact that elderly patients (after 50-55 years) do not undergo puncture surgery on lumbar discs. Experts explain this by the fact that, due to age-related aging, the lumbar intervertebral discs at this age are too severely dehydrated. This fact indicates the intractability of the unacceptably dehydrated fibrous ring to reverse retraction in the protrusion zone when using any type of nucleoplasty. And, consequently, the ineffectiveness of such procedures in elderly patients.
Rehabilitation
After a course of treatment for protrusion, it is important to undergo rehabilitation. This will not only help you get yourself in order, but also prevent the protrusion from forming again in the future.
It is important to give more rest to the affected area of the spine and not to disturb it again. Try to pay more attention to your posture, engage in therapeutic physical training, and eat right. It is important to gradually end the course of medication, otherwise the disc will quickly return to its original position before treatment.
In addition to the classic methods of withdrawing from treatment, there are others that are beginning to gain increasing popularity. Thus, among many others, one can note the effective treatment complex of Professor Kozyavkin. He uses a precise and effective technique for treating SINR, which, among other things, allows for rehabilitation after treatment of protrusion. The abbreviation stands for “Intensive Neurophysiological Rehabilitation System.”
The foundation of this popular treatment system is the idea of using various methods of influencing the patient. The main component is correction of a biomechanical nature, which is skillfully combined with therapeutic and rhythmic gymnastics, massage, apitherapy, mechanotherapy and reflexology.
Cost of services in the direction of “Medical massage”
| Services list | Duration | Price, rub |
| Back + Legs Massage | 55 min. | 3700 |
| Therapeutic back massage | 25-40 min. | 3000 |
| Neck massage | 15 minutes. | 2200 |
| Massage of the thoracic spine | 15 minutes. | 2200 |
| Massage of the lumbosacral spine | up to 30 min. | 2200 |
| Massage of the collar area + one upper limb (arm) | 30 min. | 3000 |
| Neck massage + two upper limbs | 40 min. | 3900 |
| Neck massage + chest massage | 40 min. | 3900 |
| Massage of one upper limb | 15 minutes. | 2200 |
| Massage of two upper limbs | 30 min. | 3000 |
| Chest massage | 15 minutes. | 2200 |
| Massage of the lumbosacral spine + one lower limb (leg) | 30 min. | 3000 |
| Massage of the lumbosacral spine + two lower limbs | 45 min. | 3900 |
| Massage of one lower limb | 20 minutes. | 2200 |
| Massage of two lower limbs | 30 min. | 3000 |
| Cupping massage (dynamic setting) | 25 min. | 2200 |
| Therapeutic back massage + cupping massage | 40 min. | 3900 |
| General therapeutic massage | 120 min. | 6900 |
| Modeling massage (for weight loss) (Thighs, Buttocks, Abdomen) | 45 min. | 5800 |
| Anti-cellulite full body massage | 90 min. | 7200 |
| Head massage | 20 minutes. | 2200 |
| Neck and collar area massage | 20 minutes. | 2200 |
Contact us
Call now
8 (495) 803-27-45
Make an appointment through our service
Make an appointment
Exercises
Gymnastics are prescribed by the specialist involved in your treatment, based on the results of MRI and other studies of the patient’s body. Physical activity will help to “set” the disc and give the body the necessary physical activity. But you should understand that this method of treatment is not suitable for every person. There are a number of people for whom exercise therapy can only harm. For example, you should not exercise if the pain gets worse in the affected area. It is also prohibited to exercise in the following cases:
- heart diseases;
- inflammatory processes;
- infections;
- opened internal bleeding.
Other cases do not prohibit physical therapy. But it is important to take into account the age of the patient, the location of the protrusion and the severity of the pathology before drawing up the program.
Localization determines the list of exercises, since each affected department has its own exercises. However, their goal is the same - to remove displacement, stretch the vertebrae, improve blood flow and increase physical activity. All this can have a positive effect on the patient.
Before starting class, choose comfortable clothes. You should also not forget about sports shoes: without them, gymnastics can only harm an already sore spine. To choose the right shoes, make sure that the sole is textured, thick, elastic and cushioned.
You don’t need any special equipment for practicing, just a chair and a mat (in case you are sliding on the floor). The main thing to remember is that exercise should not cause discomfort. Otherwise, you are doing something wrong and may make your situation worse.
Warm up before you start. Without warming up, you can injure unprepared muscles; this is as important a part of the lesson as the exercises themselves.
- For people with protrusion not in the cervical region, you can tilt your head to the sides and back and forth five times;
- Next, carefully rotate your wrists, elbows, and shoulders five times;
- Stand on your toes and lower yourself several times in a row;
- Stand on your toes and lower yourself several times in a row;
To improve the quality of your workout, you can take a hot shower before starting the class, which will better warm up your muscles.
Recovery after surgery
After a minimally invasive simple session, the patient is activated after 2-3 hours. Most of those operated on notice noticeable improvements within the first hours after minimally invasive surgery. Perhaps, immediately after activation, he will be allowed to go home on his own. But in order to avoid postoperative complications, which are not excluded even after percutaneous (the most gentle) surgery, the following are prescribed:
- antibiotic therapy (against infections and suppurations);
- taking vascular medications (against limb thrombosis, thromboembolism);
- a calm physical regimen, especially gentle on the lower back during the recovery period;
- special physical therapy for good restoration of the operated area, muscle strengthening, and prevention of relapses;
- wearing a support corset during rehabilitation;
- ban on lifting weights, lifelong refusal from heavy sports.
In total, rehabilitation measures take 2 months. But this does not mean that during these 2 months a person will be limited from walking, going to work, doing household chores, etc. No, with a successful intervention, patients even go to work within 3-5 days. However, non-compliance with specific rehabilitation and lifelong regimens, which the doctor thoroughly informs about upon discharge, is associated with high risks of postoperative complications. The first among them is the rapid resumption and more progressive course of protrusion.
Prevention
The main task of prevention in this case is to develop and maintain healthy muscle tone and their strength value. In the future, this will reduce the risk of complications and further development of osteochondrosis, protrusions, intervertebral hernia, as well as permanently consolidate the results of treatment. The list of preventive measures includes the following measures:
- From early childhood it is necessary to develop correct, healthy posture, and also maintain it in later life;
- Eliminate non-physiological loads on the spinal region from your life;
- Getting rid of bad habits and abstaining from them;
- Proper nutrition, taking into account the characteristics of the body;
- Regularity of sports exercises with a selected load and alternation with unloading.
And although this list is aimed at preventing protrusions, compliance with it will also help improve the quality of life in general. An organism that receives the required amount of nutrients, training and stress copes better with diseases and is less subject to degeneration and deformation. In a situation with bulging intervertebral discs, it is true that it is easier to prevent them than to cure them.
Useful tips
When treating spinal protrusion in addition to treatment methods during exacerbations (relapses), we strongly recommend that patients adhere to a gentle regimen. Limiting physical activity will prevent deterioration of the condition and further injury to the spinal roots, and will prevent the development of aseptic inflammation. When carrying out rehabilitation actions you should:
- avoid heavy activities, especially heavy lifting;
- constantly wear special orthopedic devices (soft bandages, Shants collars, elastic corsets);
- strictly follow all recommendations of our specialists;
- In case of disc protrusion during treatment, it is necessary to strictly adhere to the developed treatment method and not make adjustments on your own.
Self-medication is strictly prohibited. A frivolous attitude towards one’s own health leads to a deterioration in the condition and the development of severe complications, leading the patient to the need for complex surgical operations with a long and difficult recovery period. For example, paramedian protrusion of the intervertebral disc, in the presence of which there is complete prolapse of the nucleus pulposus, can lead to immobilization.
With the timely detection of intervertebral disc protrusions, every person should know what to do and how to help themselves or not harm themselves. We invite you to visit our specialized clinic - we can answer all your questions and help with almost any diagnosis, with the help of our experienced specialists we will provide competent treatment.
The article was reviewed by Professor, Dr. med. Sciences, neurologist Ronami V.G.