Osteochondrosis
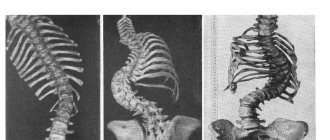
is a concept used to designate a group of diseases associated with degenerative and dystrophic changes in the structures of the spine.
First of all, the intervertebral discs suffer, and as the disease progresses, the vertebrae themselves. Degenerative
are changes associated with the processes of tissue wear, aging, loss of original properties, and
dystrophic
are changes caused by tissue nutritional disorders.
Thus, the term osteochondrosis unites most non-inflammatory spinal pathologies. Osteochondrosis of the spine
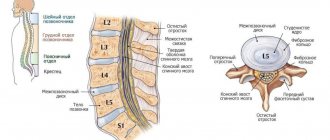
The spine forms the basis of the skeleton, connecting the various parts of the skeletal system. It supports the head, ribs and muscles are attached to it. The spinal cord passes through the spinal column, through which the brain is connected to various parts of our body. Man is the only upright creature in the world, and the spine is designed to ensure upright walking. Therefore, the spinal column has a curved shape, reminiscent of the letter S of the Latin alphabet and is not a rigid rod, but a complex structure consisting of elements fastened together - vertebrae. This structure of the spine allows us to perform various movements, be flexible and absorb shocks and shocks. The function of shock absorbers is performed by intervertebral discs - cartilaginous layers consisting of the nucleus pulposus and the fibrous ring surrounding it. The core takes on the load and absorbs it, and the fibrous ring prevents the core from flattening under pressure.
A decrease in the elasticity of the intervertebral discs can be the beginning of a wide range of problems. Unable to withstand the load, the intervertebral discs begin to deform and the spine loses its correct shape. The progression of the disease leads to further destruction of the intervertebral discs, the fibrous ring is torn, the vertebrae come into rigid contact with each other, and pinching of the nerves connecting the spinal cord with various parts of the body becomes possible. This is how osteochondrosis develops. Intervertebral hernias occur, and inflammation often develops. Deprived of shock absorption, the vertebrae can become flattened, and together their joints form scar and bone growths.
Osteochondrosis is one of the most common diseases. Only cardiovascular diseases are more common. According to some estimates, every second person on the planet suffers from osteochondrosis. Osteochondrosis is more common in women, but in men its manifestations are on average more painful.
What is osteochondrosis?
Osteochondrosis: parts of the spine
Osteochondrosis affects various parts of the spine. Depending on which department suffered the most, there are:
- lumbar osteochondrosis – most common;
- cervical – ranks second in “popularity”;
- sacral;
- chest;
- widespread osteochondrosis, which affects several parts of the spine at once;
- cross pathologies (lumbosacral or cervicothoracic).
General information
It is believed that osteochondrosis of the cervical spine is more common than in other parts. In fact, this is not so - degenerative phenomena develop evenly at all points of maximum load - in the area of the main bends of the spinal column (the lower the department is located, the greater the load it bears). However, the symptoms of cervical osteochondrosis are more pronounced and therefore seem to be a more common occurrence. This is due to the high mobility of the vertebrae of the neck, which at the same time support the head, as well as the peculiarity of the location of the exits of the spinal cord roots.
On a note!
According to statistics, the disease affects more than 60% of middle-aged and older people. However, recently there has been a rejuvenation of the pathological process - pathology occurs in young people and even adolescents. This is due to the widespread computerization of study and work, as well as a decrease in physical activity and a deterioration in the quality of nutrition.
Taking into account the age audience, 2 forms of cervical osteochondrosis can be distinguished - physiological and pathological.
The physiological process is associated with the natural aging of the body, when the symptoms of the disease are a consequence of the gradual wear of the intervertebral discs. The process occurs under the influence of the endocrine system and is a consequence of menopausal changes. The destruction of cartilaginous structures begins from the center of the intervertebral disc and is accompanied by the gradual replacement of cartilaginous tissue with fibrous tissue. The pathology is irreversible, but can be compensated with special medications.
The pathological process is associated with abnormal destructive changes in the body - immune, dystrophic, inflammatory, metabolic. First of all, pericartilaginous tissues are involved - salt deposits appear on bone structures, nerve roots become inflamed, atrophy or hypertonicity of skeletal muscles occurs, which leads to impaired blood circulation in the head-neck-chest area. With timely diagnosis, the pathology can be treated and ends with the complete restoration of the healthy function of organs and tissues.
Stages of cervical osteochondrosis and their symptoms
There are 4 main stages of the pathological process:
- Stage 1 – expressed by mild discomfort and muscle strain in the affected area, cartilage discs lose their stability;
- Stage 2 – local pain appears, especially when moving the head. Intervertebral discs are deformed, the fibrous ring begins to collapse, the distance between the vertebrae is reduced;
- Stage 3 – pain intensifies and becomes constant, movements are limited. Turning the head can provoke attacks of dizziness, nausea, impaired blood supply to the brain leads to general lethargy, fatigue, impaired concentration, cartilage tissue becomes thinner, the vertebrae close, the fibrous ring is completely destroyed with the risk of intervertebral hernia;
- Stage 4 – pain syndrome completely immobilizes the neck area; cerebral circulation is impaired and requires constant medication support; the vertebrae begin to fuse.
Causes of osteochondrosis
The causes of osteochondrosis are quite varied.
Firstly, with age, the elasticity of the intervertebral discs is gradually lost.
This means that our back requires special attention. Prolonged stay in a position that causes spinal misalignment can cause irreversible changes. You should avoid sitting in an asymmetrical position, fight the habit of lying on only one side, and carrying a load (for example, a bag) in only one hand.
A sedentary lifestyle has a detrimental effect on the health of the spine. It is necessary to move, but physical activity should be moderate. The spine should be given the opportunity to recover after stress, and it is also advisable to avoid injuries that also lead to the development of spinal pathologies.
The second group of reasons is associated with metabolic disorders
and
poor nutrition
. Food rich in carbohydrates and fats saturates the body with calories, which we, in our sedentary city life, often simply have nowhere to spend; As a result, energy is stored as fat tissue, creating excess weight. Obesity is an increased load on the spine, which leads to the development of osteochondrosis. In addition, such a diet usually contains insufficient amounts of microelements (calcium, potassium, phosphorus, magnesium, manganese and others), which are so necessary to strengthen bone tissue. Endocrine diseases are often the cause of excess weight. At the same time, a violation of energy, water or mineral metabolism can also negatively affect the tissues involved in the structure of the spine.
Factors contributing to the development of osteochondrosis may be:
- flat feet;
- hormonal changes;
- infectious diseases;
- local circulation disorders,
as well as some other factors.
Diagnostic procedures
The patient’s treatment process always begins with a comprehensive examination. He is recommended to donate urine and blood, and undergo instrumental techniques. Most often prescribed:
- X-ray. The resulting image allows you to determine the general condition of the vertebrae, the presence of injuries or the degree of development of pathology.
- Ultrasound. Ultrasound allows you to identify neoplasms or other processes that are similar in symptoms to osteochondrosis. Most often, the technique is used to exclude other pathologies.
- Myelography. The introduction of a contrast agent into the bone marrow during the process makes it possible to identify inflamed areas and determine the extent of the disease.
- MRI or CT. A high-precision technique that determines the condition of not only bone tissue, but also cartilage, joints, and intervertebral discs. Based on these data, treatment tactics are determined.
It is impossible to make an accurate diagnosis only on the basis of a visual examination; the doctor can only make a guess, and confirmation requires obtaining research results. During the process, the doctor clarifies how the disease manifests itself, determines the localization of unpleasant sensations, and studies the medical history.
Visual examination does not provide a basis for making a diagnosis, but is necessary to obtain an overall picture of the patient’s condition
Symptoms of osteochondrosis
Osteochondrosis - treatment at JSC Family Doctor
At the initial stage of osteochondrosis, there are no pronounced symptoms. The development of osteochondrosis can be assumed in the following cases:
- dull painful sensations in the back (in the affected area of the spine);
- feeling of heaviness in the back, constant tension in the spinal muscles;
- muscle numbness, the appearance of “goosebumps”. In such cases, they usually say that “the back is numb”;
- crunching when turning the body and neck;
- headache, dizziness, tinnitus (typical of cervical osteochondrosis);
- aching pain in the chest area (typical of thoracic osteochondrosis).
At the first appearance of such symptoms, it is advisable to undergo examination by a neurologist.
Further development of the disease manifests itself in symptoms that cause significant discomfort:
Back pain
There is severe pain in the back (along the spine). The pain may radiate to the limbs.
Numb fingers
A typical manifestation of osteochondrosis is numbness of the fingers and toes.
Limitation of physical activity
Even with minimal physical activity, the pain intensifies (for example, as a result of shaking and jolts when traveling in transport). Pain leads to significant limitations in mobility and physical activity.
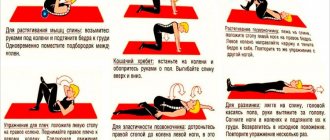
Treatment options
Treatment of common spinal osteochondrosis is aimed at eliminating pain, relieving spasm, inflammation, restoring spinal mobility and the damaged structure of cartilage tissue, and general rehabilitation of the patient. Therapy is always complex and includes taking medications, exercise therapy, and physiotherapeutic procedures. Each of them separately will not give a lasting effect; only combined use allows you to achieve the desired result.
Taking medications
During the acute period, it is extremely important to relieve the patient of acute pain, especially if it is localized in the cervical region. To do this, the following types of medications are prescribed:
Symptoms and sensations of thoracic osteochondrosis
- Anti-inflammatory drugs (Ibuprofen, Diclofenac). They allow you to suppress inflammation in soft tissues, relieve pain, and provide relief during the next attack.
- Muscle relaxants (Mydocalm, Baclofen, Sirdalud). Prescribed in the presence of spasms and muscle tension. They relax the fiber, reduce tone, thereby relieving blocks.
- Painkillers (“Solpadein”, “Ketoral”, “Analgin”). For acute pain that cannot be eliminated with conventional tablets, novocaine or lidocaine blockade is used. It will alleviate the condition and limit the area of inflammation.
- Antibiotics (“Amoxicillin”, “Penicillin”). If the inflammatory process is bacterial in nature, then such drugs cannot be avoided. They suppress the growth of pathogenic microflora and accelerate the healing process.
- Chondroprotectors (“Rumalon”, “Chondroetin”, “Arthra”, “Teraflex”). They are usually prescribed by a doctor during a period of remission to restore damaged cartilage tissue. They trigger the process of synthesis of collagen and elastane, which regenerate disorders resulting from pathology.
- Vasodilators (Trental, Berlition, Actovegin). With their help, blood flow is activated and sufficient oxygen supply to the brain is ensured.
Antidepressants may also be prescribed if the patient is chronically stressed. Taking a comprehensive multivitamin that includes B vitamins and minerals is also helpful. They also help to naturally suppress inflammation, improve blood flow and restore normal muscle tone.
Electrophoresis is carried out in a special room under the supervision of medical staff
Physiotherapy
A visit to the physiotherapist's office is recommended for all patients during the period of relief of the acute stage. Procedures are prescribed individually, taking into account the presence of contraindications, this will eliminate the risk of complications. Typically, in the treatment of widespread osteochondrosis, the following methods are used:
- Electrophoresis. Under the influence of a small electrical discharge, particles of the drug move to the area of inflammation. It is carried out using special equipment.
- Magnetotherapy. Involves the use of static magnetic fields for treatment. They have proven themselves well in the treatment of pathologies of the musculoskeletal system.
- Phonophoresis. It involves a combination of medication and ultrasound effects on the affected area. The duration and intensity of the impact is always selected individually.
- Acupuncture. Impact on acupuncture points using special needles with rounded ends. They trigger the necessary processes in the body to improve metabolism and stimulate the functioning of internal organs. It is carried out only by a qualified specialist with extensive experience.
- UHF therapy. It is the effect of ultra-high-frequency waves on the painful area and promotes faster recovery.
- Electrical stimulation. This technique is not often used, only when stimulation of nerve endings and muscles is necessary.
All the described methods are aimed at relieving stiffness and pain in the joints, restoring the natural movement of blood and lymph, and eliminating the inflammatory process. Yoga and swimming are also recommended; unlike taking medications, they are aimed not at eliminating symptoms, but at combating the cause.
Manual therapy
In addition to physiotherapeutic procedures, manual therapy sessions are also prescribed. They are performed by experienced surgeons using various exercises. With their help, the condition is alleviated in a short time, muscle tone is restored, and the correct position of the vertebrae is restored.
Manual therapy increases the clearance of pinched nerves, which reduces pain and relieves neurological manifestations. The intensity of exposure and duration of the course are selected taking into account the prevalence of the disease and the nature of the lesion. You cannot conduct classes, as in the case of therapeutic exercises, during an exacerbation.
Surgery is resorted to as a last resort
Surgery
Common osteochondrosis in the early stages (grades 1, 2) is usually treated conservatively. But if it does not give the desired result, then the doctor prescribes radical methods. Most often, the operation is palliative in nature, that is, it is performed to relieve the main symptoms and improve the patient’s quality of life. The operation itself cannot completely cure the patient, but it will temporarily relieve his pain and restore joint mobility.
The operation can be stabilizing or decompression. The first is aimed at bringing the spinal column into the correct position, the second eliminates excessive pressure on the nerve roots.
Main types of invasive techniques:
- Facetectomy. It involves removing the facet joints in order to reduce pressure on the processes.
- Foraminotomy. It is carried out to create a larger lumen in the spinal canal, which often narrows due to the proliferation of osteophytes.
- Laminectomy. Surgeons remove the back part of a vertebra that is deformed due to the development of osteochondrosis.
- Laminotomy. A portion of the vertebra is cut out to widen the brain canal.
Decompression surgeries are aimed at removing all or part of the intervertebral disc to relieve pressure on the nerve. The main techniques are discectomy and copectomy. Interventions are prescribed only as a last resort, since the risk of complications is always high. This could be infection, false fusion, pain due to the transimplant, or breakage of the implanted fasteners. After the operation, a long course of rehabilitation will be required.
Methods for diagnosing osteochondrosis
The main role in the diagnosis of osteochondrosis belongs to instrumental studies: radiography, computed tomography, MRI.
It may be necessary to confirm that the symptoms observed are not caused by other diseases. For the purpose of differential diagnosis, general and biochemical blood tests, general urinalysis, and ultrasound examinations of internal organs are performed.
X-ray of the spine
X-rays of problematic parts of the spine are taken. Which department needs to be examined is determined based on the patient’s complaints.
More information about the diagnostic method
Computed tomography (CT)
Computed tomography (MSCT) makes it possible to obtain a more informative picture of pathological processes and determine the degree of their severity. In particular, MSCT can detect intervertebral hernia.
Computed tomography is performed in cases where radiographic data is insufficient.
More information about the diagnostic method
Magnetic resonance imaging (MRI)
MRI is the most informative method for diagnosing osteochondrosis. In some cases (for example, if osteochondrosis of the thoracic spine is suspected), MRI cannot be avoided. Magnetic resonance imaging allows you to visualize cartilage and soft tissue, based on which you can localize the source of problems as accurately as possible and determine the cause of the disease.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Possible complications
If you do not start treating the pathological process in time, it will not go away on its own. Using traditional methods or painkillers will also not solve the problem. Therefore, all patients who are postponing a visit to the doctor should know the dangers of the advanced process:
- Acute dysfunction of the genitourinary system.
- Liver or kidney diseases.
- Disorders of the respiratory system.
- A variety of heart failures.
- Slowing metabolism.
- Atrophic processes in joints, decreased elasticity of muscle fiber.
- Premature aging of connective tissue.
- Constant exacerbations of pathology.
- Intervertebral hernia.
The danger of the disease is that it quickly progresses and spreads to nearby joints. For example, from the lumbar region it easily migrates to the pelvis and legs. Timely initiation of therapy will increase the chances of effectively slowing down the process, relieving unpleasant symptoms and maintaining a high quality of life. In advanced cases, patients are assigned a disability, as many lose the ability to care for themselves.
Why is cervical osteochondrosis dangerous?
The neck area concentrates a dense interweaving of major blood vessels, nerve processes and dynamic skeletal structures. Without treatment, serious pathological changes can be observed:
- weakening of the fibrous ring provokes dislocations and subluxations in the area of the most mobile vertebrae;
- the presence of osteophytes and muscle spasms leads to pinching of nerve roots and blood vessels with the formation of compression syndromes;
- destruction of cartilaginous discs and convergence of the vertebrae leads to intervertebral hernia with pinching of nervous tissue.
Each of these phenomena is followed by a pronounced negative reaction from the whole organism.
Possible complications and consequences
The list of the most common complications of cervical osteochondrosis includes:
- vegetative-vascular dystonia;
- hypertension;
- oxygen starvation of the brain and its structures;
- retinal dystrophy with visual impairment;
- malfunction of the thyroid gland;
- dysfunction of the esophagus and trachea - difficulty swallowing and respiratory spasms;
- intractable pain syndrome in the head, neck, chest, upper limbs;
- cramps and numbness of the face, hands;
- disruption of the hypothalamic-pituitary system, which entails a disruption of all hormonal activities of the body.
Clinical classification of lumbar osteochondrosis. Degrees of osteochondrosis
Classification of lumbar osteochondrosis by degree is used to systematically characterize the clinical manifestations of the disease. This classification systemically describes the symptoms of the disease and begins from the moment the patient experiences pain.
1st degree of osteochondrosis
Occurs when an intervertebral disc ruptures, caused by sudden movement or overexertion. It manifests itself as sudden pain, a feeling of electric current passing in the spine, and the muscles are reflexively tense.
2nd degree osteochondrosis
The second degree can manifest itself in the form of symptoms of intervertebral protrusion and spinal instability. Chronic pain that worsens with exercise. Intervals of remission and exacerbation alternate. The cervical spine is characterized by neck pain that worsens after a long stay in one position, headaches, arm pain, shoulder pain, periodic discomfort or numbness in the fingers. For the lumbar region - pain in the lower back, pain in the gluteal region, periodic pain in the sacrum, frequent fatigue in the legs.
3rd degree osteochondrosis
Manifests itself in the form of symptoms of a herniated disc (pain along the affected nerve, numbness in the arms or legs, changes in gait, headaches) or long-term symptoms of a herniated disc (in the cervical region: frequent headaches, tinnitus, dizziness, decreased vision, hearing , muscle strength in the arms; in the thoracic region: irregular heart rhythm, difficulty breathing; in the lumbar region: kidney disease, gastrointestinal tract, sexual dysfunction, numbness or weakness in the legs).
4 degree osteochondrosis
It is generally accepted that the fourth degree of osteochondrosis begins from the moment when the hernia no longer manifests itself, the manifestations of the disease may decrease, but the symptoms of spinal instability, slipping or twisting of the vertebrae, or their complete fixation relative to each other still remain. They may be joined by manifestations of proliferation of the vertebral bodies (osteophytes), which can also compress the spinal nerves or block the spinal canal (secondary spinal canal stenosis) and compress the spinal cord (spinal cord ischemia). In addition, the fourth degree includes the consequences of surgical intervention if the hernia was removed promptly (various types of innervation disorders, paresis, inflammation).