Subdural hematoma is a pathological condition characterized by a limited accumulation of blood between the dura and arachnoid membranes of the brain. It accounts for up to 40% of all intracranial hematomas. Most often it occurs as a result of traumatic brain injuries in male patients over the age of forty.
The danger of a subdural hematoma is that it negatively affects the brain structures located around it through pressure on them, their displacement and even damage. So she gives them some serious time. The reasons for its appearance are hemorrhages and traumatic injuries to the blood vessels of the brain.
The Neurosurgery Department of CELT invites you to undergo diagnostics and treatment of hematomas in Moscow. Our multidisciplinary clinic is equipped with the latest technology and has high-precision diagnostic equipment that allows you to make a correct diagnosis. Our specialists use gentle techniques to provide treatment in accordance with international standards.
Etiology of subdural hematomas
This type of hematoma is most often a consequence of traumatic brain injuries and ruptures of blood veins that develop as a result of them, passing in the subdural space. However, the reasons do not necessarily lie in injuries; sometimes hematomas can be provoked by pathological conditions characterized by the destruction of the walls of blood vessels and a decrease in their plasticity. Other reasons are as follows:
- Blood diseases that change its properties;
- Diseases of the blood vessels of the brain;
- Increased intravascular and blood pressure;
A hematoma formed on the side of the injury appears with a small contact area and even without direct contact. This can happen when stopping too suddenly or changing the direction of movement, as well as when falling on the lower limbs or legs. In the process, a sharp shaking of the head occurs, provoking a displacement of the cerebral hemispheres inside the skull, leading to rupture of the blood veins.
As for a hematoma formed on the opposite side of the injury, it can form when the head hits a large, inactive object, causing a large contact area. Much less often, hematomas are formed due to injuries directly to the veins and arteries when the integrity of the dura cerebral membrane is violated.
Epidural hematoma of the brain
Cerebral epidural hematoma (EDH) is a separate type of volumetric limited accumulation of liquid or clotted blood. A blood clot forms in the space between the dura mater of the brain and the bone structures of the skull.
The pathology is most often caused by damage or rupture of a large blood vessel of an artery damaged as a result of a violation of the integrity of the bones of the skull.
Epidural hematoma is a less common pathology compared to subdural variants and is recorded in no more than 3% of people who have suffered a skull injury.
The shedding of blood into the epidural space has a number of features. Most often, the victim immediately faints. The phase of loss of consciousness is followed by a period of imaginary well-being, in which there are no symptoms.
From the editor: Types of perception: auditory, visual, kinesthetic and their characteristicsAfter some time, the “bright interval” is replaced by an exacerbation stage. A sharp deterioration in the patient's well-being is recorded. Vomiting often develops. The patient is overwhelmed with anxiety. Consciousness disturbances occur. Such phenomena are caused by compression (compression) of the brain.
Epidural hematomas almost always require immediate surgical removal.
Causes and mechanism of development
In most cases, these formations are identified in persons under 45 years of age who have suffered from severe head injuries resulting in fractures of the bone structures of the skull.
The shedding and accumulation of blood in the epidural space is characteristic of blunt impact to the head area, which occurs when falling or colliding at low speed with a blunt object.
Almost always, epidural hematomas are associated with a linear fracture, in which there is no displacement of the internal bone plate.
Epidural hematomas are most often observed with traumatic brain injury in the temple area.
Such severe damage, as a rule, accompanies a rupture of the middle meningeal artery (arteria meningea media), penetrating into the cranial cavity through the spinous foramen (foramen spinosum).
Since the movement of blood through arterial vessels passes under high pressure, their rupture and subsequent outflow of blood leads to the rapid development of intracranial hypertension.
In 95% of patients, a single unilateral epidural hematoma is recorded. In the remaining 5% of patients, bilateral pathological collections and multiple foci of liquid or clotted blood are found.
More than 95% of epidural hematomas have a supratentorial localization (in the upper parts of the brain) and are located in the lobes: temporo-parietal (60%), frontal (20%), parieto-occipital (20%). The remaining less than 5% of formations are detected in the deepest part of the internal base of the skull - the posterior cranial fossa.
Symptoms
Manifestations of an epidural hematoma most often become apparent immediately after injury. The first symptom is severe cephalgia. But sometimes signs develop only a few hours after a blow to the head. In some patients, the headache spontaneously subsides for a short time, but soon it manifests itself with greater intensity.
The next symptom of hemorrhage in the epidural area is impaired function of consciousness, which increases in severity. Initially, confusion develops - loss of various mental functions. Drowsiness develops. There is a complete loss of the ability to perform movements. Sudden cardiovascular failure occurs. A deep coma follows.
In more than 50% of cases, a short-term fainting state is followed by a period of imaginary well-being. Then symptoms of depression of consciousness develop again, which are complemented by muscle weakness developing on the side of the body opposite to the damaged area of the brain.
During the light interval, the patient indicates a very intense, intensifying, unbearable headache. Cephalgia is caused by detachment of the dura mater from the inner covering of the skull. The duration of the light interval varies. Its short duration indicates massive arterial bleeding.
Fixing a “light gap” in a patient is an informative sign that the brain damage was not severe. The end of a period of relative well-being is indicated by diencephalic syndrome, most often associated with damage to the hypothalamus.
Clinic of subdural hematomas
Clinical manifestations of subdural hematomas are presented in two large groups, which can be found in our table below:
| Group of symptoms | Clinical manifestations |
| General cerebral symptoms of hematomas |
|
| Focal symptoms of hematomas |
|
Prevention
The main preventative measure is to prevent injury. Preventive steps:
- Always wear a helmet when riding a bicycle.
- Reduce adrenaline sports.
- Do not take risks when playing sports, respect the instinct of self-preservation.
- Drink alcohol in moderation.
- Do not smoke.
- When treating hypertension, take medications regularly and undergo examinations.
- Try to lose weight.
Recommendations related to hematoma:
- If you have hemophilia diagnosed at birth or use anticoagulants to thin your blood, reduce contact and adrenaline sports, which have an increased risk of injury.
- In case of a head injury with short-term loss of consciousness, nausea or other suspicious symptoms, consult a doctor for a CT scan.
- Try to stay in good physical shape. This will prevent the risk of falling.
- If necessary, use appropriate shoes and rehabilitation aids such as walkers, French sticks.
- Wear glasses to correct your vision.
- Drink enough fluids, especially in summer.
- Reduce the use of sleeping pills and blood pressure-lowering medications if they are not urgently needed. This will prevent possible collapse with subsequent falls and injury.
- If blood circulation in the extremities is impaired, use special medications and ointments.
Diagnosis of subdural hematomas
Recognition of a subdural hematoma can be seriously complicated by the variety of its clinical manifestations. In order to correctly make a diagnosis, the neurologist takes into account the following factors:
- Nature and characteristics of traumatic injury;
- Development of disturbances of consciousness;
- Presence/absence of a light gap;
- Neurological status of the patient.
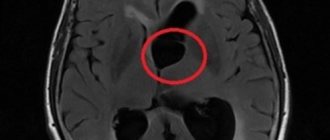
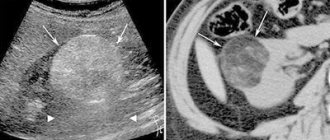
Instrumental diagnostic studies that are prescribed to the patient are presented as follows:
- X-ray of the skull;
- Detailed examination of the fundus (ophthalmoscopy);
- Cerebral angiography (study of cerebral vessels);
- Computer and magnetic resonance imaging, incl. and with contrast.
Life forecast
The prognosis of life with chronic subdural hematoma depends on the timeliness of seeking medical help. Severe consequences are observed mainly in elderly patients. Lethal cases occur not only due to the presence of the hematoma itself, but also against the background of traumatic effects on brain tissue. Edema, cerebral ischemic processes, and dislocation of brain structures may occur.
After surgical treatment, it is necessary to establish strict monitoring of the patient's condition. In the first hours after surgery, cerebral edema may occur.
Surgery for chronic hematoma is one of the most effective treatment methods. Conservative therapy is used as an additional way to help the patient. The Medsi Clinic successfully performs neurosurgical operations for such conditions.
Treatment of subdural hematomas
The treatment tactics for subdural hematomas are based on the results of diagnostic studies and the individual indications of the patient. It may involve the use of conservative or surgical techniques.
| Hematoma treatment methods | What are they? |
| Conservative | Indicated for patients who have not lost clarity of consciousness with hematomas up to 10 mm thick, accompanied by a displacement of structures by no more than 3 mm. They are also used if the patient is in a deeply depressed state of consciousness or in a coma, provided that the volume of the hematoma does not exceed forty milliliters and the intracranial pressure is not lower than 25 mm. rt. Art. Conservative treatment involves the use of drugs to prevent cerebral edema, relieve pain, vomiting and convulsions. |
| Neurosurgical | Surgical intervention is practiced for hematomas with symptoms of brain compression, focal manifestations, or in case of increased intracarnial pressure syndrome. Removal can be carried out using endoscopic techniques through a specially created opening. In addition, craniotomy is used, aimed at removing not only the hematoma, but also the areas of crush injury. |
The Department of Neurology at CELT sees neurologists and neurosurgeons with many years of experience in scientific and practical work. You can make an appointment with them online on our website or by contacting our operators: +7 (495) 788 33 88.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
4. Treatment of the disease
Depending on the patient’s condition and the volume of the hematoma formed, treatment can be either conservative or surgical. Both treatment methods have their own advantages and disadvantages. Modern medicine has new methods for treating this pathology, which combine higher efficiency compared to conservative ones and are less invasive compared to surgical ones (craniotomy). This method is called closed external drainage of the hematoma.
To eliminate the hematoma, the skull is perforated through the skin with an intraosseous needle. Then drainage
with a catheter diameter of no more than 3 mm with a fluid receiver located below the level of the head.
Practice has confirmed the high efficiency of the new method and shown a number of advantages of hematoma drainage:
- surgical removal of compression (squeezing) of the brain;
- reducing the risk of postoperative infection;
- maintaining the integrity of the skull;
- minimizing the likelihood of relapse.
Transmedavia – emergency medical assistance that saves lives
A brain hematoma is a serious injury, inattention to which can lead to the development of serious or even irreversible consequences. Timely, competent medical care can reduce the likelihood of developing complications and avoid death, and therefore, in severe cases, the count is not in hours, but in minutes.
Our doctors are true professionals in their field, who have modern, comfortable cars at their disposal, equipped with everything necessary to provide emergency care to victims. By using, you can be sure that the ambulance team will arrive quickly, take the necessary measures to save the patient’s life and deliver him to the appropriate medical facility as soon as possible. If necessary, we are also ready to arrange transportation for you to another region or treatment abroad.
How can the disease progress?
There are several options for how a hematoma can occur:
1. Called classic. Here everything goes in three phases - loss of consciousness at the time of injury, then a “bright” period when there are no symptoms, repeated loss of consciousness. During recovery, the patient will suffer from headaches, nausea, dizziness, memory loss, and a feeling of stupor.
Article on the topic
Get to the brain. What beliefs about him are wrong? 2. Option implies an erased picture of the “light” gap. The initial loss of consciousness is similar to a coma, then there is a partial restoration of consciousness, then the patient again experiences stupor or coma. Against this background, epileptic seizures may develop.
3. This option implies that there is no “light” gap. It occurs with multiple injuries, which are quite severe. The man is in a coma. There is no consciousness, there is no talk about positive dynamics.
How are they treated?
Therapy can be carried out either conservatively or surgically. To begin with, the doctor must assess the type, volume of formation, as well as the individual characteristics of the patient. In the acute form, the hematoma is removed. Displacement and compression of brain structures may also be an indication for surgery.
The prognosis in 60% of cases is unfavorable, because TBI, concussion and neurological disorders do not just go away. After surgery, the patient needs mechanical ventilation support, as well as strict blood pressure control. In 5-20% of patients, subdural hematoma can recur.