Focal epilepsy is considered one of the most common among all forms, types and subtypes of this disease. This disease is characterized by frequent and obvious seizures. Most often, the pathology manifests itself in childhood, but is distinguished by the gradual disappearance of symptoms as a person grows older.
Focal epilepsy in the international classification of diseases has an ICD 10 code G40.
Before diagnosing pathology, you should pay attention to the following points: whether repeated seizures occur and whether spontaneous paroxysms develop. The only exceptions are reflex episodes of malaise. Their classic examples are characteristic of the photosensitivity form, that is, when bright light can provoke an illness.
What is focal epilepsy
Symptomatic focal epilepsy is one of the forms of the disease in which seizures are explained by the presence in the brain of a clear and distinct focus of paroxysmal activity. As a rule, the pathology is characterized by secondary manifestations or develops against the background of other serious diseases. It is determined by simple and complex manifestations of seizures, based on the main characteristics of which the lesion can be determined.
Focal epilepsy combines any types of seizures, the formation and manifestation of which directly depends on the zone of electrical activity of neurons in cerebral structures. Starting from a small focus, epileptic activity can subsequently spread, covering an increasingly larger area of the cerebral cortex, while stimulating the development of secondary generalized seizures.
Multifocal epilepsy, caused by the presence of several lesions at once, is especially dangerous for the patient. Features of the pathology:
- if all forms of the disease are taken into account, FE accounts for more than 82% of cases;
- in more than 75% of cases, the first attack can be noticed in childhood;
- Pathology especially often develops against the background of brain damage of any etiology: infectious, traumatic, ischemic, as well as as a result of developmental anomalies as a consequence of disorders of the prenatal and birth periods;
- symptomatic focal epilepsy (ICD code 10 G40) occurs in more than 71% of cases.
Causes and pathogenesis of focal epilepsy
The development of FE is preceded by the following pathologies:
- tumors of a malignant and benign nature;
- serious disturbances of metabolic processes in the body, including cerebral circulation;
- injuries of the skull and internal tissues;
- infections of any kind, for example, encephalic or meningococcal;
- violations of the structure of the intracranial substance of a hereditary nature.
The main causes of the disease include factors acquired as a result of any negative impact on the brain or caused by hereditary diseases.
Pediatric FE is mainly characterized by prenatal problems or congenital diseases. In both cases, certain areas of the cortex are affected. In particular:
- infection inside the womb;
- oxygen starvation;
- suffocation of a newborn during the passage of the birth canal;
- increased intracranial pressure;
- birth injury.
In some cases, the disease manifests itself against the background of underdevelopment of the cerebral cortex of both or one hemisphere. The likelihood that the pathology may disappear as the child grows and develops is very high.
The functional genesis of epileptic seizures with focal seizures is characterized by several zones:
- sector of epileptogenic disorder, corresponding to the area of morphological changes visible in tomographic studies;
- primary - the compartment of the cortex in which epileptic discharges are formed;
- irregular - a source of activity observed on electroencephalography and deciphered as the period between attacks;
- functional deficit - the sector in which disorders accompanying an epileptic seizure are generated.
Causes
Partial seizures of epilepsy occur under the influence of the following factors:
- abnormalities of limited areas of the brain: cysts, arteriovenous malformations, areas of dysplasia in the cortex;
- cerebral infections: cysticercosis, abscesses, encephalitis of various origins, neurosyphilis;
- vascular pathologies: hemorrhages in the medulla;
- TBI;
- neoplasms;
- dysmetabolic encephalopathies.
During development in children, intrauterine infections and complications during pregnancy and childbirth play a significant role: fetal hypoxia, asphyxia during passage through the birth canal. Sometimes symptoms are provoked by disturbances in the maturation of cortical structures and disappear as they grow older.
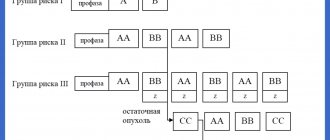
Classification of focal epilepsy
So, focal epilepsy and what is it in adults and children, how is it classified? There are many parameters for defining a term in medicine. From a neurological perspective, there are three main forms of PE:
- Symptomatic. It is diagnosed if the cause of damage to a specific sector of the medulla can be clearly identified. As a rule, instrumental diagnostics are used for this.
- Cryptogenic. It is characterized by the inability to make an accurate diagnosis depending on the location of the lesion. The likelihood that the disease is a secondary manifestation, and the frontal lobe and other parts are not damaged, is high.
- Ideopathic. Regardless of any cause, the symptoms are idiopathic in nature.
Symptoms of focal epilepsy
A common symptom for all types of pathology is a focal attack of epilepsy. Moreover, seizures recur with varying degrees of frequency. They can be simple and complex. In the first case, seizures occur at moments when the person is fully conscious, but motor, sensory and somatic autonomic symptoms are observed. Complex ones are characterized by clouding of consciousness for different periods of time, and serious manifestations of a mental nature, hallucinations, etc. occur.
By the way, complex seizures can begin as simple ones and are aggravated by loss of consciousness. The third type of pathology is non-malignant, that is, it does not lead to global impairments in speech, memory, and motor activity during the period of remission. If a child or teenager has symptomatic focal frontal lobe epilepsy, it may be accompanied by mental and psychological development. The clinical picture of the pathology directly depends on the location of the lesion and its size:
- Temple. The attack can last up to a minute, while an aura and automatism appear, in some cases there may be a loss of consciousness.
- Forehead. Characterized by serial attacks, absence of aura, turns of the head and eyes, and involuntary movements of the limbs. In this case, an attack can occur even in a dream.
- Back of the head. Prolonged seizures lasting up to 13 minutes, accompanied by visual hallucinations.
- Darkness. A rare pathology that occurs against the background of tumor processes. It is characterized by sensorimotor paroxysms, Todd's palsy, and impaired speech functions.
Most often there is one focus. It is the so-called epileptogenic zone. Under some conditions, activity is not limited to it, but spreads to the nearest sections, thereby causing characteristic disorders. In a number of situations, the development of secondary generalized paroxysms is allowed.
The hereditary disease is most often accompanied by generalized paroxysms and has a characteristic age of onset. In some cases, once a certain age is reached, the episodes stop. In such a situation, the use of antiepileptic medications is completed. On the other hand, forms have been identified in which drug therapy is lifelong.
Types and symptoms
Epilepsy is multifaceted and multifaceted; its symptoms are not limited to seizures. The most common classification is depending on the severity of attacks and their main manifestations.
Aura (harbingers)
Many epileptic seizures begin with an aura. This is the name given to a complex of specific sensations that occurs shortly before a seizure. Manifestations of an aura can be completely different: paresthesia (pathological sensations), a specific taste in the mouth, auditory, visual or olfactory hallucinations, etc. Before the appearance of an aura, a person often begins to experience causeless anxiety and internal tension.
Partial (focal) seizures
These conditions occur when a small area of the brain is involved in pathological overexcitation.
Simple partial seizures are characterized by preserved consciousness and last only 1-2 minutes. Depending on the location of the pathological focus, a person feels:
- sudden change of mood for no apparent reason;
- small twitching in a certain part of the body;
- feeling of déjà vu;
- hallucinations: lights before the eyes, strange sounds, etc.;
- paresthesia: a feeling of tingling or crawling in any part of the body;
- difficulty pronouncing or understanding words;
- nausea;
- change in heart rate, etc.
Complex attacks are characterized by more severe symptoms and often affect consciousness and thinking. Human can:
- lose consciousness for 1-2 minutes;
- there is no point in looking into emptiness;
- scream, cry, laugh for no apparent reason;
- constantly repeat any words or actions (chewing, walking in a circle, etc.).
Typically, during a complex seizure and for some time after it, the patient remains disoriented for some time.
Generalized seizures
Generalized seizures are one of the classic signs of epilepsy that almost everyone has heard of. They occur if the epileptogenic focus has spread to the entire brain. There are several forms of seizures.
- Tonic convulsions. The muscles of most of the body (especially the back and limbs) simultaneously contract (come to tone), remain in this state for 10-20 seconds and then relax. Such attacks often occur during sleep and are not accompanied by loss of consciousness.
- Clonic convulsions. Rarely occur in isolation from other types of attacks. Manifested by rhythmic rapid contraction and relaxation of muscles. The movement cannot be stopped or delayed.
- Tonic-clonic seizures. This type of attack is called grand mal, which means “great illness” in French. The attack is divided into several phases: precursors (aura);
- tonic convulsions (20-60 seconds): the muscles become very tense, the person screams and falls; at this time his breathing stops, his face becomes bluish, and his body arches;
- clonic convulsions (2-5 minutes): the muscles of the body begin to contract rhythmically, the person thrashes on the floor, foam is released from the mouth, often mixed with blood due to a bitten tongue;
- relaxation: convulsions stop, muscles relax, involuntary urination or defecation often occurs; consciousness is absent for 15-30 minutes.
After the end of a generalized seizure, a person remains for 1-2 days feeling overwhelmed, problems with coordination of movements and fine motor skills. They are associated with cerebral hypoxia.
- Atonic attacks. They are characterized by short-term muscle relaxation, accompanied by loss of consciousness and falling. The attack lasts literally 10-15 seconds, but after it ends the patient does not remember anything.
- Myoclonic seizures. They manifest themselves as rapid twitching of the muscles of individual parts of the body, usually the arms or legs. The seizure is not accompanied by loss of consciousness.
- Absence seizures. The second name for attacks is petit mal (minor illness). This symptom of epilepsy occurs more often in children than in adults and is characterized by a short-term loss of consciousness. The patient freezes in place, looks into emptiness, does not perceive speech addressed to him and does not react to it. The condition is often accompanied by involuntary blinking of the eyes, small movements of the hands or jaws. The duration of the attack is 10-20 seconds.
Pediatric epilepsy
Childhood epilepsy has many masks. In newborns, it can be manifested by periodic muscle contractions that do not resemble seizures, frequent tilting of the head back, poor sleep and general restlessness. Older children may suffer from classic seizures and absence seizures. Partial seizures most often occur:
- severe headaches, nausea, vomiting;
- short periods of speech disorder (the child cannot utter a single word);
- nightmares followed by screams and hysterics;
- sleepwalking, etc.
These symptoms are not always a sign of epilepsy, but they should serve as a reason for an urgent visit to the doctor and a full examination.
Diagnosis of focal epilepsy
Approximately 65 million patients worldwide are diagnosed. It begins to develop most often in childhood, adolescence or old age. The disease is diagnosed in men more often than in women. It is impossible to cure completely, but its course can be controlled with the help of medications and various techniques.
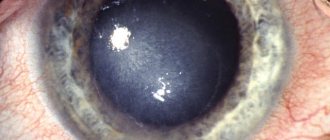
The occurrence of partial paroxysm is a serious manifestation that requires urgent medical intervention. First of all, the doctor will conduct a visual examination and interview the patient to identify visible symptoms of the disease. The following should be excluded from the list of causes of defeat:
- Focal cortical dysplasia is a disorder of neuronal proliferation and the architecture of the cerebral cortex.
- Vascular malformation is a violation of the intrauterine development of the brain, accompanied by a violation of its structure and functions;
- Tumors are both benign and malignant, and in both cases they threaten serious health problems.
The neurologist must identify the sequence, timing, frequency and strength of the attacks. The information obtained allows us to determine the location of the lesion with maximum accuracy.
To obtain confirmation of the diagnosis, the patient first needs to contact a specialist - a neurologist or epileptologist. The patient is prescribed the following diagnostic tests:
- Electroencephalography is a technique that allows you to determine epiactivity in the interval between attacks.
- An EEG with provocative tests is prescribed if the information obtained during the first study is insufficient. Sometimes daily monitoring of cortical activity is carried out.
Extremely informative data is obtained if the electrodes are installed under the skull. The method is called subdural corticography, but due to the complexity of its implementation, it is little used in ordinary medical practice.
To identify quantitative and qualitative indicators of the morphology of changes, several basic research methods are used:
- MRI or magnetic resonance imaging with a slice thickness of no more than 2 mm. With the symptomatic type of the disease, changes of a different nature will be observed on the tomogram, including atrophy and lesions. If none are found, most likely the patient has an idiopathic or cryptogenic form of epilepsy.
- PET or positron emission. The study allows you to determine hypermetabolic processes in the affected area.
- SPECT or single photon emission computed tomography. In this case, it is possible to determine the lack of blood supply to the lesion.
Forecast
The prognosis depends on the type of disease. Idiopathic epilepsy is characterized by a benign course, maintaining the usual level of mental activity and cognitive abilities. Sometimes it disappears spontaneously after puberty. In the symptomatic form, the outcome is determined by the underlying disease.
In the absence of serious cerebral changes, adequate selection of drug therapy makes it possible to completely eliminate attacks or significantly reduce their frequency. Significant improvement after surgery is observed in 60-70% of patients, complete recovery in 30%.
At the Leto clinic you can get qualified help for partial forms of epilepsy. High-quality diagnostics and competent medicinal support will allow you to solve the problem and return to a full life. Sign up by phone..
Treatment of focal epilepsy
FE of any etiology and complexity is treated under the supervision of a neurologist or epileptologist. In each case, drug treatment is prescribed, which necessarily includes taking anticolvulsant drugs. When treating the symptomatic form of the disease, the cause of the disease is determined, and it is this that is treated first, simultaneously eliminating the symptoms of attacks and seizures.
In children under 1 year of age, it consists of correct diagnosis, identifying the causes of the disease, and selecting specific medications that can calm the pathological focus and reduce its excitability. Children are often diagnosed with status epilepticus. This means frequent attacks following one another. Their number can exceed 50 times a day.
Drug treatment works best for the occipital and parietal forms of the disease. In the case of the temporal lobe, after a couple of years resistance to taking medications occurs, and the pathology develops with renewed vigor. If a patient has a similar picture, this is considered a direct indication for further surgical intervention.
Surgical intervention is performed by neurosurgeons. The procedure is aimed at eliminating the lesion - a tumor, cyst or area of the brain affected by the disease. However, in medical practice such operations are undertaken only if the lesion is well localized. The operation is called focal resection; in case of multiple or extended lesions, extended resection is indicated. Surgical intervention is carried out only if all laboratory and hardware tests have been completed, and the structure and functionality of the cerebral cortex zones on a corticograph have been taken into account.
Prognosis of focal epilepsy
No doctor can give an accurate prognosis of the course and results of PE. It all depends on the type of pathology and the complexity of its course. For example, the idiopathic variant is characterized by the absence of cognitive impairment. Very often, the pathology resolves spontaneously, so it is almost impossible to predict the outcome.
Symptomatic is due to the influence of the pathological focus on the patient’s body. The prognosis is unfavorable for the development of tumors; in children, this form entails a delay in mental development. As a rule, without appropriate treatment, this form of the disease progresses extremely rapidly.
According to experts, in more than 70% of cases of disease manifestations after surgery, a sharp improvement in the patient’s condition is observed. Subsequently, complete relief from the disease is noted in 30% of cases.
Types of partial seizures
As described earlier, several options for the development of this type of disease are possible. Let's take a closer look at each of them:
- The temporal one occupies the position of the most common type, accounting for 50-60% of all cases associated with distortion of neural connections.
- Frontal is the second most common manifestation; in approximately 25% of cases the disease is associated with this pathology.
- Occipital appears quite rarely, in no more than 10% of patients.
- Parietal almost never occurs and has a probability of occurrence of less than 1%.
The localization of the lesion is determined using an EEG (electroencephalogram). Most often, diagnosis is carried out while the patient is at rest, but the most accurate results can be obtained only during an attack. To create such a situation, with the consent of the patient, special means are used.
In addition to classification according to local criteria, there is also a system of differences based on severity. The following forms are distinguished:
- Simple - not accompanied by a distortion of consciousness, manifestations are variable and determined by the region.
- Complex - simple seizures with simultaneous impairment of consciousness.
- Secondary generalized (convulsive) - develops from simple and complex seizures, accompanied by convulsions.