Osteochondrosis (degenerative disc disease) in the lumbar spine or lower back is caused by involutional changes in the discs, which leads to lower back pain.
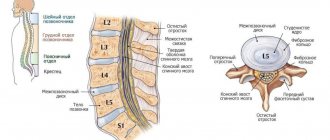
Intervertebral discs are tough, fibrous structures that act as ligaments between vertebrae, absorbing shock and providing shock absorption to the spine. The discs are flexible but strong enough to facilitate movements such as bending your torso forward, backward or sideways.
Despite the name, osteochondrosis is not considered a true disease and symptoms usually do not worsen over time. Discs, like all structures of the body, degrade as we age, and disc degeneration develops in all people as part of the involutionary process.
A characteristic feature of osteochondrosis is a gradual decrease in symptoms as the spine begins to stabilize. Treatment for lumbar spine degenerative disc disease focuses on minimizing pain, stabilizing the spine, and improving or maintaining mobility.
Symptoms
Most cases of manifestation of osteochondrosis of the lumbar spine consist in the presence of minor, constant back pain, which intensifies from time to time for several days or more.
Symptoms may vary, but the most common include:
- Moderate, constant pain in the lower back. Pain in the area of the damaged disc is the most common symptom of disc degeneration. The pain may radiate to the buttocks, groin and upper thighs. This pain usually feels dull and can range in intensity from mild to severe.
- Periodic acute episodes of pain. Back pain may get worse for a few days or weeks and then return to a more mild level. Flare-ups of pain occur as the spine degenerates and subside as the spine gradually stabilizes. Flare-ups of pain can occur suddenly and pain often results in decreased mobility.
- Local soreness. The area of the lower back surrounding the degenerated disc may be tender to the touch. Local soreness is caused by inflammation and muscle tension in the area of the disc damaged by degeneration.
- Leg pain. Neurological symptoms, including numbness, weakness, or sharp, shooting pain in the buttocks, thighs, and/or back of the leg, may be felt if the height of the disc is significantly reduced and conditions for nerve root compression occur. Pain in the legs with osteochondrosis of the lumbar spine usually does not fall below the knee.
- A feeling of sudden weakness or instability may occur when the disc is significantly weakened and the patient feels as if the lower back is not functioning properly.
In addition, the pain may increase or decrease with certain movements or certain postures, such as:
- Pain when sitting. Sitting for long periods often causes lower back pain and stiffness to worsen and is relieved by standing up or changing positions.
- Increased pain when bending or rotating. Twisting the spine and bending forward, backward, or sideways can cause intense, pain in the area of the damaged disc.
- Reduced pain when walking or changing position. When the spine changes position, the pressure on the discs is reduced or redistributed from the discs to the muscles and joints. Changing positions frequently, alternating between standing and sitting, and short walks can help relieve stiffness and keep pain to a minimum.
Disc degeneration should not cause symptoms of bowel/bladder dysfunction, fever with back pain, unexplained and rapid weight loss, or intense abdominal pain. These symptoms indicate more serious conditions and often require surgical treatment.
Proper nutrition for osteochondrosis
To prevent the problem from developing and help eliminate it, the clinic doctor develops an individual diet. Basic principles of proper nutrition for osteochondrosis:
- increase the amount of fresh fruits in the diet;
- eat more greens and vegetables (tomatoes, onions, carrots, cabbage);
- include dairy products in the area;
- drink only purified and still water;
- consume more foods containing calcium (sesame, almonds);
- increase the consumption of wheat, eggs, barley, which contain a lot of proteins;
- eat more seafood.
In addition, it is necessary to maintain the level of vitamins A, B and D in the body.
At the same time, it is necessary to reduce consumption or completely abandon:
- spicy foods and foods high in salt;
- strong coffee and tea;
- alcohol, including low-alcohol drinks (beer);
- fried, dried and smoked products (fish, meat);
- products with artificial inclusions (GMO).
Proper nutrition will protect intervertebral discs from premature damage and reduce the risk of their displacement.
Associated symptoms
With osteochondrosis of the lumbar spine, in addition to low back pain, other symptoms associated with disc degeneration may occur. For example:
- Proteins contained within the disc can cause significant inflammation if they come into contact with the surrounding spinal structures, and this inflammation can lead to spasms of the lower back muscles as well as radicular pain radiating to the hips and the back of the lower extremities (also called sciatica).
- Lumbar disc degeneration can contribute to the development of lumbar stenosis and/or lumbar osteoarthritis, as well as other conditions in the lower back.
- A degenerated disc can also lead to a herniated lumbar disc. Neurological symptoms from a herniated disc can be acute and intense.
- Symptoms caused by disc degeneration in the lumbar spine can vary widely depending on how quickly or completely the disc degenerates and how it affects surrounding spinal structures.
- Pain from osteochondrosis is usually caused by deformation of the muscles that support the spine and inflammation around the structures adjacent to the disc.
Literature:
- Biktimirov R.G., Kedrov A.V., Kiselev A.M., Kachkov I.A., Osteochondrosis of the spine - Almanac of Clinical Medicine - 2004. P.329,330,333,334, https://cyberleninka.ru/article/n/osteohondroz-pozvonochnika/viewer
- Human anatomy: textbook. -method. manual / M. V. Ulitko, I. M. Petrova, A. A. Yakimov; [under general ed. M. V. Ulitko]; Ministry of Science and Higher Education education Ros. Federation, Ural. federal n-t. - Ekaterinburg: Ural Publishing House. University, 2021. - 88 p. ISBN 978-5-7996-2447-7
- Oleynik A.D., Kovalev S.A. // Criteria for a comprehensive assessment of foci of lumbar osteochondrosis // Bulletin of the International Scientific Surgical Association - 2008 P. 84 https://cyberleninka.ru/article/n/kriterii-kompleksnoy-otsenki-ochagov-poyasnichnogo-osteohondroza/viewer
- Nikiforov A.S., Avakyan G.N., Mendel O.I., Modern approaches to the treatment of complications of spinal osteochondrosis - RMZh No. 26 from November 26, 2010 - P.1633 https://www.rmj.ru/articles/nevrologiya /Sovremennye_podhody_k_lecheniyu_osloghneniy_osteohondroza_pozvonochnika/
- Velichko T.I., Loskutov V.A., Loskutova I.V. // Exercise therapy and therapeutic swimming in orthopedics // 2014 -2.5 — Osteochondrosis https://monographies.ru/en/book/section?id=7270
- Gushcha A.O., Konovalov N.A., Dreval O.N., Grin A.A., Dzhindzhikhadze R.S., Arestov S.O., Dreval M.D., Kashcheev A.A., Vershinin A. V.V., Asyutin D.S., Korolishin V.S., Clinical guidelines for the diagnosis and treatment of herniated intervertebral discs of the lumbosacral spine. - 2014 - pp.4,7,8 https://www.mst.ru/information/manual/lumbar_disc_herniation.pdf
- Pilipovich A.A., Treatment and prevention of osteochondrosis - 2015. — S.1,17,18,19 https://cyberleninka.ru/article/n/lechenie-i-profilaktika-osteohondroza/viewer
- Rodichkin P.V., Shalamanov N.S. Pathophysiological rationale for complex therapy of intervertebral hernias -2012-P.32 https://www.vmeda.org/wp-content/uploads/2016/pdf/31-36.pdf
- Instructions for medical use of the drug Motrin ® tablets, Reg. number P N002874/01 ///o-motrin
- Buchakchiyskaya N.M., Maramukha V.I., Maramukha A.A., Maramukha I.V., Non-drug treatment of patients with neurological manifestations of osteochondrosis of the lumbar spine - Science of Life and Health - 2013. P.104 https://cyberleninka.ru/article/n/nemedicamentoznoe-lechenie-bolnyh-s-nevrologicheskimi-proyavleniyami-osteohondroza-poyasnichnogo-otdela-pozvonochnika-sovremennyy/viewer
- Therapeutic physical education for spinal osteochondrosis: textbook / O. V. Bezrukova, G. I. Bulnaeva; GBOU VPO IGMU of the Ministry of Health of Russia. – Irkutsk: IGMU, 2013. – 58 p.
- Frick et al. Efficacy and safety of naproxen sodium and ibuprofen for pain relief after oral surgery. Current Therapeutic Research. 1993;54(6):619-27.
- Clinical recommendations. Diagnosis and treatment of musculoskeletal (nonspecific) pain in the lower back. Russian Interregional Society for the Study of Pain. 2021
- Cochrane Database of Systematic Reviews. (2010.) “Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica.” https://pubmed.ncbi.nlm.nih.gov/20556780/
- Svetoslav Nikolaev Stoev, Stanislav Radoslavov Gueоrguiev, Vasil Georgiev Madzharov, Hristina Viktorova Lebanova (2021). “Naproxen in Pain and Inflammation – A Review”, International Journal of Pharmaceutical and Phytopharmacological Research, 11(1), pp.142-148.
Causes of osteochondrosis of the lumbar spine
Osteochondrosis occurs due to age-related wear and tear of the disc structure, and the degeneration process can be accelerated by injury, general condition, health and lifestyle, and possibly a genetic predisposition to the development of pathological processes in the musculoskeletal system.
Osteochondrosis rarely begins with a serious injury, such as a car accident. It is more likely that the initiation of degenerative processes is associated with low-energy disc trauma.
Low back pain associated with lumbar osteochondrosis is usually generated by one or more pathological processes:
- Inflamed, proteins from the disc irritate surrounding nerves - both small nerves in the disc itself and potentially large nerves that go to the legs (sciatic nerve).
- Abnormal micromotion instability when the outer rings of the disc, called the annulus fibrosus, wear out and cannot effectively absorb force vectors onto the spine, resulting in movement along the vertebral segment.
- Over a long period of time, pain from osteochondrosis of the lumbar spine eventually decreases, rather than getting worse. This pain relief occurs because the fully degenerated disc no longer has any inflammatory proteins (which can cause pain) and the collapsed disc moves into a stable position, eliminating the micro-movements that cause pain.
Risk factors
Lifestyle factors that affect overall health can affect intervertebral discs. Risk factors for degenerative disc disease (osteochondrosis) include:
- Family history of back pain or musculoskeletal disorders
- Excessive stress on the lower back due to sports or the nature of work
- Prolonged static loads on the discs due to prolonged sitting and/or poor posture
- Lack of disc support due to weak back muscles
- Obesity
- Smoking or any form of nicotine consumption
Disc degeneration is part of the aging body, but not all people develop pain or any specific symptoms. Symptoms tend to occur when there is instability, muscle tension, and possibly nerve root irritation.
Lifestyle correction
The first thing the doctor does after discovering lumbosacral osteochondrosis is to recommend that the patient make a number of specific changes to his lifestyle. They will vary in different cases and depend on individual characteristics. So, if the patient is overweight, he will be advised to take measures to eliminate it. This could be a transition to a more rational, healthy diet, or an increase in the level of physical activity. But any grueling workouts and one-component diets for weight loss are strictly contraindicated!
If lumbosacral osteochondrosis is diagnosed in an office worker, he is advised to increase the level of physical activity. As a rule, it is worth leaving your workplace every hour to stretch and restore normal blood circulation in all parts of the body. It is also recommended to walk outdoors more often. This will not only help you feel better, but will also help improve your sleep quality.
With the development of lumbosacral osteochondrosis in people engaged in heavy physical labor or prone to frequent grueling workouts, they will, on the contrary, be recommended to reduce the load on their back or even change the type of activity. Weightlifting, wrestling, and jumping sports are contraindicated for this disease.
Diagnostics
- The medical history includes a detailed study of the patient's symptoms, their intensity and the relationship of pain with exercise or body position. Information about regular physical activity, sleep habits, and past injuries is also needed.
- A physical examination is necessary to examine range of motion and muscle condition. The presence of painful areas on palpation or physical abnormalities is also determined. In addition, neurological tests are performed to determine neurological deficits.
- The above diagnostic methods are usually sufficient to diagnose osteochondrosis, but an accurate diagnosis requires the use of imaging methods.
- CT
- Radiography
- MSCT
- PAT
- MRI is a diagnostic method that allows you to clarify the degree of degeneration, the presence of fractures, herniated discs and stenosis. Often, an MRI examination is necessary in preparation for surgical treatment in order to accurately determine the location of the degenerated disc and plan the operation.
Studies have shown that MRI findings of moderate to severe disc degeneration are found in scans of patients with both severe pain and minimal or no pain. In addition, many disease conditions may not show up on MRI. For this reason, the diagnosis cannot be made solely on the basis of imaging results, and verification of the diagnosis is possible only on the basis of a combination of all clinical and instrumental examination methods.
Non-drug therapy
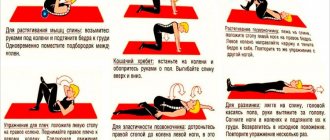
Physical therapy plays an important role in the treatment of lumbar osteochondrosis5,10,11. To prevent the development of the disease and alleviate its symptoms, the lower back muscles must be kept in good shape. Dosed physical activity and exercises help strengthen the muscle corset, increase range of motion and prevent complications5,11.
There are various complexes, which usually include exercises such as “bicycle”, “scissors”, lifting the body, performed in a lying position11. It is useful to do the “penknife” exercise: lying on your back, you need to press your hips to your chest and your head to your knees, “folding” like a penknife. It is recommended to do the exercise 10 times in total11. Therapeutic swimming also helps with osteochondrosis5.
It is better to carry out training under the supervision of a specialist in physical therapy, since many exercises are allowed only in the interictal period, and bending the torso forward at a certain angle can displace the disc even more5,11.
In addition to physical therapy, for lumbar osteochondrosis they use5,10:
- corsets;
- “stretching” the spine;
- manual therapy and massage;
- physiotherapy (magnetic therapy, laser therapy, ultrasound therapy);
- acupuncture.
Considering that osteochondrosis in advanced cases can lead to complications, it is important to pay close attention to the spine at any age. Prevention of disease and pain requires active action - normalizing weight, choosing comfortable shoes and regular physical activity. If the pain is severe, you should consult a doctor who will select the optimal treatment.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
to come back to the beginning
Treatment
Initial treatments for lumbar spine osteochondrosis and pain usually include the following combinations:
- Over-the-counter pain relievers
such as aspirin (Bayer), ibuprofen (Advil), or naproxen (Aleve) can reduce inflammation that contributes to discomfort, stiffness, and irritation of the nerve roots. - Prescription pain medications
. For severe pain, muscle relaxants or narcotic painkillers may be prescribed. These drugs are usually used to treat intense, sharp pain that is not expected to last more than a few days or weeks. These medications can be addictive and cause serious side effects, so they should be used with caution. - Heat and ice
. Applying heat to the lower back improves blood circulation, which reduces muscle spasms and tension and improves mobility. Ice packs can reduce inflammation and relieve mild pain. It is helpful to apply heat before exercise to relax muscles and to apply ice after exercise to minimize inflammation. - Manual therapy.
Manipulation by a specialist is a popular method of pain management for low back pain. Medical practitioners called chiropractors use their hands to manipulate different areas of the body to relieve tension in muscles and joints. Manipulation has been found to be an effective measure for temporarily reducing pain, and in some cases is as effective as drug therapy. - Massage
. Massage techniques can reduce tension and spasms in the muscles of the lower back, reduce pressure on the spine and relieve pain. In addition, therapeutic massage can improve blood circulation, delivering nutrients and oxygen to tight muscles. - Epidural steroid injections
(ESI). Injecting a steroid into the space surrounding the spine can reduce pain impulses as well as inflammation. A steroid injection can be used in conjunction with a physical therapy program to relieve pain during exercise and rehabilitation. Typically, an epidural steroid injection can reduce pain for a period of several weeks to one year.
In many cases, a combination of treatments is necessary for effective pain relief. A process of trial and error is usually necessary to find the treatment that will be most effective.
Prolonged bed rest is not recommended, and immobilization is generally possible for severe pain for a short period of time, as lack of physical activity can weaken the muscles and normal support of the spine.
Exercise therapy and activity modification
Exercise is essential to maintaining healthy spinal mobility. An effective exercise program for the lumbar spine should include:
- Stretching exercises for the muscles of the lower back, hips and pelvis, as well as the harmstring muscles. Tightening of these muscles increases pressure on the lumbar spine and contributes to the development of lower back pain.
- Strengthening your lower back and abdominal muscles helps you maintain good posture and better support your spine. A muscle strengthening exercise program may include an individual exercise program, dynamic lumbar spine stabilization, tai chi, Pilates, or others.
- Low-impact aerobic exercise, which increases your heart rate, improves blood circulation and the supply of nutrients and oxygen needed to repair body tissues. For example, this could be walking, swimming and water aerobics.
Exercise programs are usually tailored on a case-by-case basis, depending on your overall health, severity of pain, and personal preference.
In addition, small adjustments to daily activities (lifestyle modifications) can effectively alleviate pain. For example, wearing a brace when lifting heavy objects or avoiding twisting when lifting heavy objects can prevent increased pain due to excessive stress on the discs. Using an ergonomic chair and orthopedic mattress can also improve your posture and reduce stress on your discs.
Surgery
Surgical treatment of osteochondrosis of the lumbar spine is necessary in cases where conservative treatment for 6 months was ineffective. Surgical treatment for osteochondrosis is always selective, which means that the patient himself decides whether to undergo surgery or not.
It is recommended that all factors be taken into account before deciding to undergo surgery for osteochondrosis, including the length of the recovery period, pain management during recovery, and spinal rehabilitation.
Vertebral fusion surgery
The standard surgical treatment for lumbar spine degenerative disc disease is fusion surgery, in which two vertebrae are fused together. The purpose of fusion surgery (spinal fusion) is to reduce pain and eliminate instability in the motion segment of the spine.
All spinal fusion surgeries consist of the following:
- The damaged disc is completely removed from the intervertebral space (discectomy).
- Stabilization is carried out using bone graft and/or instrumentation (implants, plates, rods and/or screws).
- The vertebrae then fuse to form a solid, immobile structure. Fusion occurs within a few months after the procedure, and not during the operation itself.
After the operation, wearing a corset and taking analgesics are prescribed. Physical exercises are included very carefully, taking into account the individual characteristics of the patient and the degree of tissue regeneration. Full recovery from fusion surgery may take up to a year while the vertebrae fuse together.
Surgical replacement with artificial disc
Replacing a damaged disc with an artificial implant has been developed in recent years as an alternative to fusion surgery. Disc replacement surgery consists of completely removing the disc damaged by degeneration (discectomy), restoring the disc space to its natural height, and implanting an artificial disc.
This procedure is designed to maintain motion in the spine similar to natural motion, reducing the likelihood of increased pressure on adjacent spinal segments (a common complication of spinal fusion).
Recovery from disc replacement surgery usually lasts up to 6 months.
Orthopedic devices and prevention
Some patients are advised to wear orthopedic corsets, which help reduce the load on the spine. They differ in the degree of rigidity and design features, so your doctor will help you choose a specific model. He will be able to accurately determine whether a particular patient needs a bandage or not.
But absolutely everyone who has been diagnosed with lumbosacral osteochondrosis is recommended to change their mattress and pillow to orthopedic ones. If you have osteochondrosis, you should sleep on a medium-hard mattress that maintains the physiological curves of the spine, and the right pillow will help support the cervical spine.
Thus, lumbosacral osteochondrosis is a fairly common problem, which over time can lead to a number of undesirable consequences, including the need for surgery or disability. Therefore, when symptoms of the disease appear and after its diagnosis, it is important to immediately begin treatment for lumbosacral osteochondrosis in Moscow under the guidance of an experienced neurologist according to an individually designed program.
0 0 votes
Article rating