Disc herniation of the cervical spine is an advanced form of degeneration of the cervical intervertebral segments, which is complicated by displacement of the nucleus pulposus of the disc with its extension beyond the anatomical boundaries. The disease is characterized by pronounced neurological and reflex manifestations, including the cerebral type. This is explained by the fact that in this section the ridge connects to the head, and the spinal cord passes into the brain, and a dense neurovascular network is concentrated here. The pathological process is mainly a complication of long-term osteochondrosis, the symptoms of which were ignored by patients for a long time.
MRI of the cervical spine.
Even a hundred years ago, in the field of view of neurologists, pathology with such a serious localization fell into the category of isolated cases, and it was mainly the lot of older people. Today, cervical intervertebral hernia is one of the most common diagnoses among all possible problems with the spine. Now, unfortunately, it too often concerns the working population. The diagnosis of “cervical hernia of the spine” predominates in people 20-55 years old. The incidence rate in men and women is approximately the same: 52% of patients are male patients, 48% are female.
In general, in the structure of all diseases of the human body, cervical hernias occupy 5th place in the number of hospitalizations, 3rd place in the need for surgical treatment. According to data from authoritative sources, at least 20% of people with cervical hernias suffer from severe vertebroneurological disorders, which often lead to disability. In approximately 35%-40%, the pain syndrome becomes chronic, which is why patients live in constant stress and emotional tension.
The risk group includes people suffering from systemic connective tissue diseases, obesity and various metabolic disorders, diabetes mellitus, and orthopedic pathologies. Also, professional athletes, office workers, teachers, machine operators, seamstresses, draftsmen and other people whose cervical region lingers in an immobilized position for a long time or performs monotonous monotonous movements have a high predisposition to displacement of the disc fragment in the cervical region.
Basic information about the disease
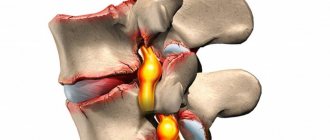
An intervertebral hernia of the cervical spine develops when the integrity of the fibrocartilaginous discs—the shock-absorbing pads between the vertebrae—is disrupted. In this case, the elastic nucleus pulposus located inside extends beyond the spinal column, compressing the spinal cord and spinal nerve roots.
As a rule, this is preceded by periodic pain in the neck. Such complaints occur in more than half of the population, and constant pain persists throughout the year in a quarter of the adult population. Pains of a more varied nature occur in women, but in men they appear more often.
The cervical region is the most mobile part of the spine, consisting of 7 small vertebrae C1 - C7). The vertebrae are quite fragile and easily injured; the muscles that support the cervical spine are less powerful than the spinal vertebrae.
These structural features contribute to permanent injury to the cervical vertebrae. The hernia most often develops in the lower sections at the levels C5–C6 and C6–C7. The code for cervical intervertebral hernia according to the International Classification of Diseases, 10th revision (ICD-10) is M51.
A herniation of the cervical spine is accompanied by dysfunction of the brain and spinal cord, compression of the vertebral arteries supplying the brain and the development of severe complications. But not everything is so bad: contacting an experienced specialist will help stop the pathological process. Such specialists can be found at the Paramita clinic.
Reviews of classes in our center
Feedback from a patient of the Innovative Medical Center
Patient's review Innovative Medical Center
Feedback on recovery after knee surgery
26.01.2021
I would like to express my gratitude to all the staff of the medical center for the treatment provided. I came to the center for treatment of heel spurs. The initial appointment was with Dr. Bogdanov V.Yu., who, after an examination, prescribed a course of UHT and hyvomat. I would like to express my special gratitude to the physiotherapist Tatyana Ivanovna Shmakova for her professionalism and excellent human qualities. After several procedures, the quality of life improved significantly. The pain gradually goes away. I hope it goes away forever. Thank you very much again. The medical center is very well located, not far from the metro, and has its own parking lot. The center is very cozy and equipped with modern equipment. If the need arises, I will definitely contact this institution.
read in full Olga
04.12.2020
I came to the center with back pain, the spasm would not go away. After several sessions of kinesiotherapy and massage, the spasm went away and my back felt better.
read in full Elena
All reviews
Causes of development of a hernia of the cervical spine
Intervertebral hernia of the cervical spine develops under the influence of the following reasons:
- Degenerative-dystrophic changes in the vertebral discs – osteochondrosis. The disease can develop at a young age in the presence of predisposing factors:
- burdened heredity (familial osteochondrosis);
- sedentary lifestyle - nutrition of intervertebral discs in adults occurs osmotically, becoming more active during movement; if a person moves little, the discs lose moisture, become thinner and crack;
- poor nutrition, excess of high-calorie foods with limited vegetables and grains;
- bad habits – smoking, alcohol abuse.
- Cervical spine injuries:
- microtraumas – constant minor injuries, for example, during work involving constant tilting of the head and neck, work involving vibration, frequent sudden turns of the head, etc.;
- macrotraumas – compression fractures, vertebral subluxations; They are rare, but very dangerous; against their background, a variety of changes in the vertebrae and discs subsequently develop.
- Cervical scoliosis is a curvature of the spine due to hormonal disorders or hereditary predisposition.
The cervical region is the most mobile part of the spine.
People in the following professions are at risk for developing a cervical hernia: athletes, military personnel, dancers, people who work at a computer for a long time, hairdressers.
Psychosomatics
There is a clear connection between physical disorders and the characteristics of neuropsychic development and mental trauma. Thus, a hernia of the cervical spine often indicates the impossibility of coming to terms with some situation, solving it with willpower, or making a compromise. The constant fear of losing the love and support of a loved one leads to the same result.
Psychotraumatic situations continue for years, which leads to retraction of the neck into the shoulders, constant stubborn tilt of the head, and improper development of the neck muscles. All this sooner or later affects the condition of the cervical discs and ends with the development of a hernia.
Laboratory research
Laboratory tests are necessary to exclude other diseases (rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome and polymyalgia rheumatica). These studies may include the following tests:
Rheumatoid factor (increased in rheumatoid arthritis)
HLA-B27 (positive in ankylosing spondylitis)
Erythrocyte sedimentation rate (increased in polymyalgia rheumatica)
In addition, blood tests can rule out infectious processes such as discitis, epidural abscess or vertebral osteomyelitis:
Changes in the number of leukocytes (increased, with a shift to the left - with bacterial infection)
Blood culture (positive if infection is present)
Red blood cell sedimentation rate (increased during infection)
Symptoms of a herniated cervical spine
A cervical hernia develops gradually and does not manifest itself at first. The sudden appearance of severe pain or other manifestations of a hernia is most often associated with some triggering factor - a sudden turn of the head, injury, stress or illness.
First signs of illness
At first, the signs of a cervical hernia are vague:
- periodic neck pain that goes away on its own;
- a feeling of numbness and crawling on one side of the neck when tilting or turning the head for a long time; numbness of fingers on one side;
- crunch in the neck when turning;
- changes in blood pressure;
- frequent headaches, which are not always associated with the condition of the spine;
- periodic attacks of dizziness;
- double vision, tinnitus;
- drowsiness during the day and insomnia at night.
If such signs appear, it is better to immediately consult a doctor and undergo a course of treatment - at this stage, a developing hernia is best treated.
Obvious symptoms
The characteristic symptoms of a cervical hernia usually develop after several years. In the cervical spine, symptoms have a clear connection with the level of disc damage. Symptoms are very varied:
Radicular syndrome
Radicular syndrome develops when the roots of the spinal nerves are pinched and manifests itself in the form of pain, motor and sensory disturbances, and metabolic disorders. When different discs of the cervical spine are affected, the following symptoms develop:
- C2 – C3.
Tormenting headaches - migraines. Pain and sensory disturbances in the neck are often unilateral. Visual, auditory, olfactory disorders. Lesions of the facial nerve - paresis and paralysis, impaired tongue movements. Frequent inflammatory processes of the ENT organs. Hernias in this disc develop extremely rarely. - C3-C4.
Sensory disturbances extend to the entire half of the neck. The pain radiates to the teeth, face, ear. Visual and hearing impairments. Mental disorders are typical - depression, panic attacks. A rare type of hernia. - C4 – C5.
Numbness and pain spread throughout the neck, inner and front surface of the shoulder. Muscle weakness. It is difficult to turn your head and bend your arm at the elbow. A common type of hernia. - C5 – C6.
Pain and sensory disturbances along the back of the shoulder. The pain may spread along the outer edge of the arm to the thumb. The neck muscles are tense. Paresis and paralysis. Cough, shortness of breath, bronchospasms, hoarseness. The most common location of cervical hernia. - C6 – C7.
The pain spreads along the outer and back surface of the arm, radiating to the shoulder blade, elbow, 2nd to 5th fingers. The function of the thyroid gland is impaired. Happens frequently.
When different cervical vertebrae are affected, different symptoms appear.
Autonomic disorders
Often the main symptoms of cervical disc herniation are autonomic disorders. They develop when the autonomic fibers of the spinal nerve roots, which innervate internal organs and the walls of blood vessels, are pinched.
At the same time, pain in the heart of a very different nature, changes in blood pressure, nausea, vomiting, sweating, changes in body temperature, and hand tremors appear.
Dizziness
The cause of dizziness due to cervical disc herniation is vertebral artery syndrome. This group of symptoms develops when the vertebral artery that supplies the brain is compressed by a hernial protrusion. The two vertebral arteries enter the lateral foramen of the vertebrae at the level of C6. And once they enter the cranial cavity, they merge into a single basilar artery, which supplies the base of the brain, the medulla oblongata, which contains the vital vasomotor and respiratory centers.
Compression of the artery leads to disruption of the blood supply to the brain, causing severe dizziness, weakness, fainting, sudden loss of coordination, visual and hearing disorders. Headaches in the form of migraines (half of the head hurts) are also typical.
Numbness
Numbness of individual parts of the body develops when the sensory fibers of the spinal roots are pinched. This is one of the manifestations of radicular syndrome. Sometimes, instead of numbness, the patient has a feeling of goosebumps crawling throughout the body.
Symptoms of cervical hernia in men
Cervical hernia occurs more often in men than in women. They are more likely to experience pain along the pinched roots and impaired movement. More common are segmented types of hernia with segments entering the spinal cord, developing paresis and paralysis.
Symptoms of cervical hernia in women
Women are characterized by a wide variety of manifestations of cervical hernia. Especially often they develop vegetative symptoms with heart pain and changes in blood pressure. Panic attacks and very often migraines occur.
What types of intervertebral hernias are most difficult to treat?
4 stages of treatment for intervertebral hernia
Dangerous symptoms
The most dangerous symptoms of a cervical hernia include:
- partial or complete movement disorders - paresis and paralysis - they signal that the spinal cord has been damaged;
- a sharp sudden onset of dizziness, headache with nausea, vomiting and loss of consciousness - indicates a sudden disturbance of cerebral circulation, which can be complicated by the development of ischemic stroke.
If such symptoms appear, the patient must be hospitalized, so it is necessary to call an ambulance.
Complications and consequences of the disease
The cervical region is the narrowest part of the spinal system, in which the largest arteriovascular highway passes. The department includes the largest arteries - the left, right vertebral and basilar, each of which forms up to 6 groups of vascular branches.
In the back of the neck there is also an important cervical nerve bundle (node), which consists of the hypoglossal, lesser occipital, greater auditory, transverse, and supraclavicular nerves.
Thus, even slight deformations of the disc, displacement of the vertebrae in an overly narrow area, densely penetrated by nerves and blood vessels, can cause a real catastrophe:
- clamping of arteries and nerve roots, constant severe pain;
- blocking the circulation of blood and cerebrospinal fluid between the spinal cord and brain with severe cerebro-vertebral signs;
- neurotic nature of auditory and visual disturbances, frequent loss of consciousness, coordination disorders;
- serious dysfunctions of the gastrointestinal tract (nausea, vomiting, fecal incontinence), urinary system (uncontrolled urination) and genital organs (impotence, frigidity, infertility);
- muscle weakness of the arms, including complete or partial paralysis;
- depression of respiratory functions due to severe damage to the spinal substance and nerve nodes, up to the cessation of breathing;
- insufficient blood supply to the brain, which can lead to cerebral ischemia and stroke.
Why are hernias of the cervical spine dangerous?
Intervertebral hernia of the cervical spine is dangerous because the pathological focus is located near the vital centers of the brain and spinal cord. Therefore, it is very important to seek medical help promptly, without waiting for severe symptoms and serious complications to appear.
Stages
The formation of a cervical hernia occurs in the following stages:
- degenerative-dystrophic
- under the influence of various factors, metabolism in the discs of the cervical spine is disrupted, they become thin, and lose their shock-absorbing properties; This stage is characterized by the appearance of primary symptoms; - protrusion
– the fibrous disc is covered with cracks, the nucleus pulposus is displaced at the edge of the disc. The pain intensifies, sensory disturbances and vegetative symptoms appear; a sudden movement or turn of the head is enough for the disease to progress to the next stage; - extrusion
- violation of the integrity of the fibrous ring and exit of the nucleus pulposus beyond the disc, compression of nerve roots, spinal cord and vertebral arteries; A detailed picture of the disease with all the characteristic symptoms; - sequestration
- segments are separated from the nucleus and enter the spinal cord, compressing it and disrupting various functions. At this stage, severe complications are possible - strokes, paresis, paralysis.
By size, cervical hernias are divided into small (up to 2 mm), medium (3 - 4 mm), large (5 -6 mm).
Complications
If a cervical hernia is not treated in the early stages, complications will arise.
In advanced stages of the disease, the following complications are possible:
- cervicalgia (cervical lumbago) - the sudden appearance of severe pain in the neck, due to which the patient cannot move;
- cervical migraine - severe attacks of headache in one side of the head with nausea and vomiting;
- paresis and paralysis of the muscles of the face, neck, arms;
- cardiac and respiratory arrest due to cerebrovascular accident.
The complications are serious, so if these symptoms appear, you should urgently call an ambulance.
What to do during an exacerbation
An exacerbation can begin under the influence of some external (trauma, heavy lifting) or internal (any acute disease) factors. With each exacerbation, the condition of the affected disc worsens - the disease progresses. During remission, this process stops.
Experts are trying to prevent exacerbation. For this purpose, courses of anti-relapse treatment are prescribed. With proper adequate treatment, the process of destruction of cervical discs can be completely stopped.
Impact of massage
The leading function of massage is to create a trophic effect. This means that massage techniques make it possible to increase blood circulation in the area of interest, ensure better lymph outflow and the supply of necessary metabolites and oxygen to tissue cells. Another goal of massage is to prevent atrophic phenomena in muscle structures and reduce intradiscal compression. However, we note that in no way can special techniques for massaging the cervical-collar area eliminate the hernia and reduce its volume.
This type of treatment is recommended strictly according to indications, since it is not equally useful for all types of hernias. It is prescribed especially with caution for medium and large protrusions, nerve pinching in the projections of the neck. Such manipulations in a neglected, complicated clinic can give a completely opposite effect, since it is easy to turn a large hernial mass in an unfavorable direction using this method of influence. Therefore, before prescribing a massage, the doctor must weigh the pros and cons.
At the beginning of the development of a hernia, massage can serve as an excellent measure to prevent the progression of degenerative-dystrophic pathogenesis in a still slightly changed disc. But we emphasize that massage techniques, if the doctor gives the go-ahead for them, should be carried out by a good massage therapist from the neurology department. And, finally, this is an auxiliary treatment tactic, which makes sense to use purely in conjunction with other basic treatment programs.
Types of cervical hernias
All manifestations of the disease depend on the direction in which the nucleus pulposus is displaced. Based on this feature, the following types of cervical hernias are distinguished:
- Dorsal
– the nucleus falls back into the canal where the spinal cord passes. They occur frequently and are divided into:- median
- the nucleus wedges into the spinal cord in the middle and compresses the spinal cord; the largest in size, accompanied by paresis and paralysis; - paramedian
- with deviation from the middle; causes pinching of two roots - at this and the following levels; accompanied by severe pain along the nerves - radiculopathy. - Foramial
- the nucleus pulposus wedges into the hole from which the spinal nerve root emerges and pinches it. Severe radiculitis pain along the pinched nerve. - Lateral
- causes pinching of the root at a given level, but less severe than foramial. The cervical vertebrae are small and there is practically no distinction between foramial and lateral species. - Ventral
- the nucleus moves forward without touching the spinal cord, so it does not manifest itself for a long time. Pain and decreased mobility gradually appear due to ossification of the ligaments. A rare type of cervical hernia. - Schmorl's hernia (vertical)
- the nucleus is wedged into the bone of a vertebra located above or below the hernia. It occurs mainly in children or with severe osteoporosis - loss of bone tissue due to loss of calcium. It is asymptomatic, but can sometimes cause vertebral destruction.
Also distinguished:
- diffuse (widespread) cervical hernia
- a large protrusion occupying half the circumference of the disc; - sequestered cervical hernia
- the separated segment enters the spinal canal; the most dangerous type of hernia.
What types of hernias develop in individual cervical discs
Lateral and foramial intervertebral hernias most often develop in the C6-C7 discs. They make up 60% of all hernias in a given disc. Median and paramedian hernias with movement disorders are much less common.
When the C5–C6 disc is affected, lateral and foraminal hernias with radicular pain are much less common, in approximately a quarter of cases. Here you can often find median hernias with significant motor impairments.
All types of posterior and lateral hernias occur on discs C4 – C5. On the upper discs, hernias are very rare and can have different directions.
Read about other types of spinal hernias here.
Each type of intervertebral hernia has serious complications, so you should not delay treatment.
See how easy it is to get rid of a hernia in 10 sessions
Pain due to hernia of the cervical spine
Acute pain from a herniated cervical spine is of two types: associated with compression of the spinal nerve roots - radiculopathy and headaches associated with cerebrovascular accidents and autonomic disorders.
In addition, patients may be bothered by constant aching pain that intensifies with various movements or after a long stay in the same position.
Symptoms of a cervical hernia include constant aching pain.
Cervical lumbago (cervical radiculopathy, cervicago)
The pain begins suddenly after a sharp turn or tilt of the head and is associated with pinching of the spinal nerve roots. The pain is very severe, patients compare it to an electric shock. This pain is most often localized on the back of the neck and spreads along the upper limb to the hand and fingers.
At the same time, a sharp spasm of the neck muscles occurs - the patient is unable to move his head. Severe pain does not allow movement, sometimes it is difficult for the patient to even talk, cough or sneeze. After some time, the pain may become less acute, but continues to be excruciating. Without medical help, it can last several hours or even days, and then over time become chronic with exacerbations and remissions.
Cervical migraine
These are attacks of painful unilateral headaches that develop against the background of vertebral artery syndrome. The cause of the sudden development of migraine may be tissue swelling or prolonged positioning of the head in the same position, followed by a sudden change in position.
Unlike classic migraine, in which the headache is associated with a sharp dilation of blood vessels and stagnation of blood, with cervical migraine there is compression of the vessels supplying the brain and the nerve plexuses surrounding them. The pain is one-sided, severe, and can begin either suddenly or relatively gradually. May have a pressing, tearing character. It often begins in the back of the head, then spreads to the eye socket, ear, teeth, and forehead. Accompanied by nausea, vomiting, visual and hearing impairment. The attack can last for several hours.
How to relieve pain
With a cervical lumbago, the patient should:
- lie down on a hard surface with a small pillow under your knees; or take a different position in which the pain is felt less;
- ask others to call an ambulance;
- take any painkiller orally: Analgin, Pentalgin, Ibuprofen, etc. You can apply pain-relieving ointments externally to painful areas: Voltaren, Fastum-gel, etc.
Voltaren, Fastum-gel, Analgin, Pentalgin, Ibuprofen will help get rid of cervical lumbago.
Emergency doctor:
- will give a painkiller injection; For this purpose, drugs from the group of non-steroidal anti-inflammatory drugs - NSAIDs are usually used; the most effective is Diclofencac;
- muscle relaxants (Mydocalm) are administered to relieve muscle tension;
- if this does not help, a paravertebral blockade is performed - an anesthetic (Novocaine, Lidocaine) is injected into the soft tissue near the exit site of the spinal roots.
If this does not help, the patient is hospitalized and an epidural block is performed - an anesthetic is injected into the space between the hard shell of the spinal cord and the bone of the spinal column.
For cervical migraine, the patient should:
- take the most comfortable position to help reduce pain during a spinal hernia; for most patients this is a supine position;
- ask loved ones to open a window or window - the patient needs fresh air;
- close the curtains on the window, reduce the number of sets, remove any sounds;
- take a painkiller - Analgin, Nise, Paracetamol.
If the pain does not go away for a long time, you can call an ambulance. The doctor will enter:
- intramuscularly any drug from the NSAID group - Diclofenac, Nise;
- glucocorticoid hormones (Dexamethasone) – will relieve tissue swelling and reduce constriction of the vessel;
- nootropic drugs – reduce tissue oxygen demand (Nootropil);
- drugs that improve blood flow - Pentoxifylline.
The effect of gymnastic exercises
Of course, it will not be possible to get rid of the disease through special gymnastic exercises for the neck. Exercise, even the best, is not able to “retract” the fallen pulpous element back or destroy it without a trace, or “patch” the gap in the fibrous ring. This can only be accomplished during surgical treatment.
However, exercise therapy has been proven to improve well-being and, importantly, prevent the development of atrophy of the muscles of the cervical and cervicothoracic complex and upper extremities. Let us immediately emphasize that the productivity of LH action is significantly reduced in the penultimate and final stages of the hernia. Still, unique physical training makes the greatest contribution to the restoration of musculoskeletal potential after surgical repair of a hernia. In general, the effect of physical therapy both during conservative therapy and at the time of postoperative rehabilitation is due to:
- stimulation of blood circulation;
- activation of metabolic processes;
- increasing the production of nutrients necessary to maintain the functions of the spinal structure;
- strengthening and increasing endurance of the neck muscles;
- correct, gentle development of motor and support functions of the neck;
- increasing the distance between the vertebrae, which helps prevent or reduce radicular/vascular compression.
But in order to really benefit from gymnastics, you need to get a training program from a specialist that is specially designed just for you, taking into account all the characteristics of the clinical picture on MRI. Plus, indicators of age and body weight, level of physical fitness, and associated health problems are taken into account.
It is advisable to take the first course in a physical therapy room under the supervision of a professional instructor in order to thoroughly understand and hone the technique of each individual exercise. When performing training, it is important to follow 5 rules:
- Regularity of exercise therapy.
- Gradual increase in load.
- Smooth and accurate movements of the cervical spine.
- Complete abolition of physical exercise if the slightest pain or changes in sensitivity appear in any part of the body.
- Based on point No. 5, urgently contact a treating specialist so that he can conduct a high-quality examination and make adjustments to the therapeutic exercise plan.
Taking and applying any physical activity on your own from the Internet, at random, or on the advice of other patients is highly not recommended! In the acute phase, exercise therapy is contraindicated! If you neglect these rules, the likelihood of achieving disastrous results is too high. Consequences of an illiterate campaign - exacerbation of symptoms of hernia SHO
, increased frequency of relapses, progression of disc displacement, even greater reduction of the spinal lumen, compression and death of nerve endings, damage to the spinal cord/brain, compression and narrowing of the cervical arteries, separation of the hernial sequestrum. As a result, the deadline for the operation will not move away, but will noticeably get closer.
Diagnostics
To make a correct diagnosis and prescribe treatment, the patient must be examined. The following instrumental studies are prescribed:
- X-ray of the cervical spine in direct and lateral projections - for cervical hernias is not very informative, since it allows you to see a large hernia based on indirect signs - structural changes in the vertebral area;
- computed tomography (CT) – you can clearly see any pathology of bone tissue; CT scan with contrast injection (performed only in a hospital) - allows you to assess how much the hernial protrusion compresses the spinal cord;
- magnetic resonance imaging (MRI) - allows you to examine soft tissues in detail, including hernial protrusion.
How to treat a herniated cervical spine
Treatment of a herniated cervical spine should be comprehensive and include both medications and any other methods that can improve the patient’s condition.
Drug treatment and folk remedies
First of all, they try to relieve the patient from pain. For severe pain, NSAID injections are prescribed - Diclofenac, Nise, Ibuprofen. In the absence of the required effect, pain blockades with Novocaine or Lidocaine are performed. To eliminate muscle tension, treatment is carried out with muscle relaxants (Mydocalm)
If the pain is not too severe, treatment is carried out with medications of the same group, prescribed internally in the form of tablets and capsules and externally in the form of ointments, creams and gels. Neuroprotectors are required - B vitamins that improve the functioning of the nervous system (Milgamma, Neuromultivit).
Drug treatments for cervical hernia also include drugs to improve blood circulation (Pentoxifylline). To improve venous blood flow, Troxevasin and Detralex are included in the treatment.
To stimulate metabolic processes in damaged discs, agents based on animal cartilage tissue are prescribed - chondroitin and glucosamine (Astra, Teraflex, Dona).
Sometimes, to enhance the effectiveness of treatment and partially replace medications with natural remedies, traditional medicine methods are used, for example, the following:
- dandelion jam; for a liter jar of dandelion flowers - a liter of water, keep on low heat for an hour, strain, discard the raw materials, add 1 kg of sugar, cook for another 45 minutes, then add the juice of one lemon, bring to a boil; cool and take a teaspoon 3 – 5 times a day; continue treatment for 1-2 months; Neck pain is gently and imperceptibly eliminated;
- tincture for external use; Pour 15 bay leaves into 500 ml of vodka and leave in a glass jar for 72 hours in a dark place, shaking occasionally; strain and rub your neck overnight.
Physiotherapy
Physiotherapy goes well with any other methods of conservative treatment of cervical hernia. Physiotherapy relieves pain, improves blood circulation and metabolism. Depending on the stage of the disease and the type of hernia, the following procedures are included in the treatment:
- electrophoresis
- administration of medicinal solutions using electric current; treatment is often prescribed at the stage of pain relief with novocaine; - Darsonval currents
are pulsed currents of high frequency and voltage, but of low strength; relieve pain, restore normal blood circulation; - laser therapy
– improves blood circulation, has an anti-inflammatory effect, prevents relapses of the disease; - UVT (shock wave therapy)
– treatment promotes the restoration of pathologically altered tissues.
Read more about electrophoresis here.
To treat a herniated cervical spine at home, you can purchase a Vitafon vibroacoustic device.
Fixation means
For severe neck pain and vertebral artery syndrome, patients are recommended to wear a special cervical collar to fix the spine. This prevents tissue injury and gradually relieves pain. Wearing it is prescribed until the pain disappears completely (5 – 10 days). Wearing a collar all the time is not recommended, as the neck muscles weaken.
Another method of fixation is taping - a modern technique for fixing soft tissues using adhesive tapes, preventing microtrauma of the discs.
Massage and manual therapy
Massage for intervertebral disc herniation in the cervical spine is done at any stage of the disease. The course will improve blood circulation, tighten and strengthen the neck muscles and you will not experience pain for a long time. But these procedures can only be entrusted to a specialist with a medical education and a massage certificate. Doing such a massage in a bathhouse or sauna is life-threatening.
Manual therapy is a procedure performed by a manual therapist. During the session, the doctor will eliminate muscle spasms, compression of blood vessels and nerve roots. Sometimes it’s even possible to repair a hernia this way.
Massage and manual therapy are done at any stage of the disease.
Hirudotherapy
Treatment with leeches is almost always included in the complex therapy of cervical disc herniation, since the saliva of leeches has analgesic properties, perfectly relieves inflammation and swelling of tissues, thins the blood, and improves blood circulation.
Reflexology
A method of influencing acupuncture points located on the human body and reflexively connected with all organs and tissues of the body. The method allows the patient to completely relieve pain in the first sessions, even with severe disc damage. After completing a course of treatment, a person forgets about pain for a long time, and regular reflexology courses allow him to feel healthy.
Psychotherapy
All patients with cervical disc herniation should undergo courses of treatment from a psychotherapist or psychologist, since during their illness they have accumulated many unresolved psychological problems that aggravate the course of the disease. But such treatment is especially necessary for people whose disease is caused by psychosomatics. The task of a psychotherapist is to identify and treat these symptoms.
Surgery
Surgical intervention should be carried out strictly according to indications for:
- the appearance of pronounced symptoms of compression of the spinal cord in the form of paresis and paralysis, which cannot be eliminated by conservative methods;
- severe pain (radiculopathy) lasting more than 8 weeks despite treatment.
Nowadays, gentle operations are carried out using microsurgical techniques, which significantly reduce the risk of complications. But if we compare the long-term consequences of conservative and surgical treatment, they are almost the same.
Rehabilitation after surgery
Conservative treatment is also effective as a means for rehabilitation after surgery for herniated disc. During this period, the patient requires a specialized individual course of measures to restore motor functions after surgery and consolidate the achieved result. Doctors at the Health Workshop clinics in St. Petersburg will prepare a course of rehabilitation treatment for you. It will restore the functions of muscles, blood vessels and organs.
Additionally, physiotherapeutic methods such as massage or (if the discs are displaced relative to each other) manual therapy with correction of the position of the discs may be prescribed.
In some cases, spinal traction may be performed using specialized equipment. This procedure not only helps to align the vertebrae, but is also a preventive measure, and therefore can be used even before the problem actually makes itself felt. The procedure in some cases is moderately painful.
These methods are used exclusively when the problem is not in the acute stage.
Exercise therapy for herniated cervical spine
Why is therapeutic exercise so important for cervical hernias? The fact is that a feature of the intervertebral discs of an adult is the lack of blood supply. Nutrition to their tissues comes osmotically from the environment. But in order for the nutrient fluid necessary for metabolism in cartilage tissue to appear in the environment, muscles must work.
Only muscle work can maintain the discs in normal condition. With a sedentary lifestyle, and if you are still overweight, the discs are quickly destroyed. Exercise therapy also helps strengthen the muscles that support the spine, improves blood circulation and blood flow to the muscles, brain and spinal cord.
Therefore, complexes of therapeutic exercises are included in the treatment program immediately after pain relief. A set of exercises is selected by a physical therapy doctor and performed under the supervision of an instructor
Exercises for morning exercises
Together with an instructor, you can select a number of exercises for daily morning exercises, perform them under his supervision, and then continue exercising at home. Here are some exercises:
- lie on your back, relax and begin to clench and unclench your fists with force; do 20 times, relax, count to 20 and repeat;
- sit on a chair, hang your arms down and rotate your shoulders first in one direction, then in the other; perform 5 – 10 times; if difficult, 2 – 3 times;
- sit on a chair, back straight, arms hanging down; raise your arms first to the sides, then, without stopping, up, and then lower them in the reverse order; repeat 3 times.
By doing morning exercises, you can gradually increase the number of exercises performed and the number of approaches.
If pain occurs during the exercise, exercise should be stopped immediately. The next day it can be performed only if there is no pain and the load has been reduced.
Causes
The appearance of a hernia in the cervical spine is caused by:
- weak muscle corset, excess weight and lack of at least minimal physical activity or, conversely, excessive physical activity;
- age-related changes that affect the condition of intervertebral discs;
- smoking and other bad habits;
- spinal injuries, incorrect posture;
- infections;
- osteochondrosis, etc.
Many factors lead to wear and tear on the spine and its components, and hernias appear either suddenly or gradually.
Approach to treating the disease in our clinic
We fully examine each new patient using modern laboratory and instrumental diagnostic methods, including MRI. After this, the attending physician together with the patient draw up a treatment plan. Comprehensive treatment must include:
- the most modern Western methods of treating cervical disc herniation;
- traditional oriental methods aimed at improving the health of the body as a whole, which leads to healing from a hernia.
As a result of this approach to the treatment of intervertebral hernia of the cervical spine, the patient gets rid of pain already in the first sessions of treatment, his mood improves, and there is hope for a return to normal life. After completion of treatment, patients do not forget about our clinic and regularly come for maintenance treatment. Most of them return to normal life.
The truth about treatment: analysis of the effectiveness of all tactics
Do medications help?
In the acute period, doctors prescribe medications for pain, inflammation and swelling for local and internal use to relieve painful manifestations of the disease. The basis of such drug therapy is NSAIDs:
- Indomethacin;
- Ibuprofen;
- Meloxicam;
- Diclofenac.
In addition to non-steroidal anti-inflammatory drugs for pain, specialists prescribe medications from a series of analgesics:
- Analgin;
- Spasmalgon;
- Ketorol.
If the clinical picture is aggravated by muscle hypertonicity, muscle relaxants are recommended to relax the spasmodic muscle structures. Among the most used muscle relaxants are Mydocalm and Siralud.
With constant debilitating pain, which NSAIDs and analgesics cannot cope with, a transition to treatment with strong hormonal or anesthetic drugs is carried out. These include glucocorticosteroids, lidocaine and novocaine. Using powerful hormone-containing and anesthetic agents, only as prescribed by a doctor in specialized conditions, the patient is given a course of spinal blockades. In the very near future, a person with such a critically unsafe diagnosis needs to undergo surgery.
All of the listed drugs act purely symptomatically: there will be no effect in terms of reducing the hernia component. In fact, they only temporarily relieve pain by blocking the transmission of nerve-pain impulses in the problem area. They also have a moderate anti-inflammatory effect. All intervertebral deformations and degenerations still do not disappear.
Note that limiting yourself only to drug therapy, even if it helps to get rid of pain, is the height of recklessness. With this approach, a hernia of the cervical spine will soon remind itself, and next time in a more vivid manifestation. But the worst thing is that, living only on painkillers, intervertebral pathogenesis will actively progress, increasing the risk of disability more and more every day.
Achieving stable remission through a drug regimen in complex combination with other conservative methods, as observations show, is not always achievable. If the initially prescribed complex treatment for 3 months, maximum 6 months, does not lead to tangible and lasting improvements, the patient is recommended to undergo surgery.
Long-term internal use of pain medications or their injection method is fraught with the development of side effects - stomach ulcers, liver and kidney diseases, hematopoietic and immune systems. External agents - gels, creams, ointments - have less negative reactions. But in terms of the strength of the analgesic effect they provide, they are significantly inferior to oral medications and injections.
It is impossible not to say a few words about popular chondroprotectors, the action of which is aimed at improving metabolism and activating nutrition in osteochondral structures. Remember, their benefits have been clinically confirmed exclusively for osteochondrosis that has not developed into a cervical hernia. It is acceptable to use such drugs for small protusions as a preventive measure for further degeneration of the cervical intervertebral disc. But! When hernia has already occurred, chondroprotectors are ineffective or “don’t work” at all. When a global restructuring of the disk contents into an irreversible (!) non-viable state has already occurred, they do not provide any therapeutic or prophylactic benefit.
General clinical recommendations
Patients with a cervical hernia are recommended to:
- eat properly regularly, but do not overeat, exclude sweets, baked goods, and high-calorie foods from the diet; eat more vegetables and fruits; healthy dishes that include animal cartilage tissue and gelatin - jellied meats, jelly;
- move more, do morning exercises, swim, just walk;
- to the extent possible, cure all concomitant diseases;
- monitor your weight;
- you cannot: run, jump, ride a bicycle, hang on a horizontal bar, or lift weights.
Prevention of exacerbations
In order to prevent relapse of the disease, you need to lead an active healthy lifestyle, follow all the doctor’s recommendations and carry out a course of anti-relapse treatment several times a year.
We use non-surgical hernia treatment techniques
Read more about our unique technique
What complications can this disease cause?
Complications always occur from complete disregard for treatment or unscrupulous implementation of the treating doctor’s recommendations. In such cases, the disease rapidly progresses and can lead to the development of ischemic stroke, vertebrobasilar insufficiency, radiculitis or complete paralysis.
As it progresses rapidly, the intensity of the pain syndrome constantly increases, performance and normal lifestyle are disrupted, and this can lead a person to disability.
FAQ
How to sleep with a hernia in the neck?
It's better to sleep on your back, but if you're comfortable on your side, you can too. The bed should have a hard base and a fairly soft mattress. Orthopedic pillow with a bolster at neck level.
Is it possible to do yoga?
It is possible, but only after consulting with your doctor.
How to strengthen the neck muscles with a hernia?
Regular performance of special exercises selected during exercise therapy classes.
Only the attending physician can answer the question of how to treat a herniated cervical spine after an examination. You should not delay your visit to the clinic, because the sooner you seek help, the easier it will be to cure you.
Specialists from the Paramita clinic in Moscow are waiting for you!
Literature:
- Levin O.S. Diagnosis and treatment of pain in the neck and upper extremities. RMZh.2006.9. 713 – 718.
- Bubnovsky S.M. Spinal hernia is not a death sentence! - M.: Eksmo, 2010. - ISBN 978-5-699-41232-7.
- Adams AC Neurology in Primary Care. F. A. Davis, Philadelphia, 2000, p. 83.
- Eubank JD Cervical Radiculopathy: Nonoperative Management of Neck Pain and Radicular Symptoms // Am. Fam Physician. 2010. Vol. 81. P. 33–40.
Themes
Intervertebral hernia, Spine, Pain, Treatment without surgery Date of publication: 07/28/2020 Date of update: 03/16/2021
Reader rating
Rating: 5 / 5 (2)
Which doctor should I contact?
Many specialists deal with diseases of the spine, one of the main ones is a neurologist. An experienced and qualified specialist not only knows how to cure a cervical hernia, but always tries to do everything possible to cure it without surgery. The doctor's task is to:
- relieve pain syndrome;
- relax your neck muscles;
- improve nutrition of the fibrous ring of the damaged disc;
- ensure balance of the spine and strengthen the neck muscles.
After treatment, the patient is given recommendations to prevent relapses and maintain the results obtained. If you are overweight, it is recommended to lose it, it is also advisable to get rid of bad habits, improve your diet and begin to strengthen your muscle corset.