Serious spinal disease is often called humanity's price for evolution. Since our distant ancestors became upright, the load on the spine has increased many times over. The anatomical structure of the spine ensures its mobility, but at the same time creates the preconditions for osteochondrosis, the indispensable companion of which is severe pain.
General information
It is believed that osteochondrosis of the cervical spine is more common than in other parts. In fact, this is not so - degenerative phenomena develop evenly at all points of maximum load - in the area of the main bends of the spinal column (the lower the department is located, the greater the load it bears). However, the symptoms of cervical osteochondrosis are more pronounced and therefore seem to be a more common occurrence. This is due to the high mobility of the vertebrae of the neck, which at the same time support the head, as well as the peculiarity of the location of the exits of the spinal cord roots.
On a note!
According to statistics, the disease affects more than 60% of middle-aged and older people. However, recently there has been a rejuvenation of the pathological process - pathology occurs in young people and even adolescents. This is due to the widespread computerization of study and work, as well as a decrease in physical activity and a deterioration in the quality of nutrition.
Taking into account the age audience, 2 forms of cervical osteochondrosis can be distinguished - physiological and pathological.
The physiological process is associated with the natural aging of the body, when the symptoms of the disease are a consequence of the gradual wear of the intervertebral discs. The process occurs under the influence of the endocrine system and is a consequence of menopausal changes. The destruction of cartilaginous structures begins from the center of the intervertebral disc and is accompanied by the gradual replacement of cartilaginous tissue with fibrous tissue. The pathology is irreversible, but can be compensated with special medications.
The pathological process is associated with abnormal destructive changes in the body - immune, dystrophic, inflammatory, metabolic. First of all, pericartilaginous tissues are involved - salt deposits appear on bone structures, nerve roots become inflamed, atrophy or hypertonicity of skeletal muscles occurs, which leads to impaired blood circulation in the head-neck-chest area. With timely diagnosis, the pathology can be treated and ends with the complete restoration of the healthy function of organs and tissues.
Stages of cervical osteochondrosis and their symptoms
There are 4 main stages of the pathological process:
- Stage 1 – expressed by mild discomfort and muscle strain in the affected area, cartilage discs lose their stability;
- Stage 2 – local pain appears, especially when moving the head. Intervertebral discs are deformed, the fibrous ring begins to collapse, the distance between the vertebrae is reduced;
- Stage 3 – pain intensifies and becomes constant, movements are limited. Turning the head can provoke attacks of dizziness, nausea, impaired blood supply to the brain leads to general lethargy, fatigue, impaired concentration, cartilage tissue becomes thinner, the vertebrae close, the fibrous ring is completely destroyed with the risk of intervertebral hernia;
- Stage 4 – pain syndrome completely immobilizes the neck area; cerebral circulation is impaired and requires constant medication support; the vertebrae begin to fuse.
Types of treatment
Like diagnosis, treatment of cervical osteochondrosis requires an integrated approach. The therapeutic volume is selected individually. It depends on the segment of the lesion, the severity of the disease and the severity of clinical symptoms. The main treatment methods are:
- taking medications;
- physiotherapy;
- Healing Fitness;
- massage;
- surgery.
Among the medicinal methods of treatment, several groups of drugs are used:
- Painkillers. They are used to reduce the severity of pain.
- Nonspecific anti-inflammatory drugs. Used to reduce tissue swelling and inflammatory syndrome. Prescribed in various forms (tablets, products for external use).
- Antispasmodics. Relieves spasms and reduces pain.
- Chondroprotectors. Restore the structure of intervertebral discs.
- B vitamins. Positively affect the state of the nervous system.
Cervical osteochondrosis: signs, symptoms, treatment of pathology
In the first stages, osteochondrosis is asymptomatic. As the disease develops, a distinctive feature becomes the presence of painful or uncomfortable sensations in the head, neck and chest, and less often in the upper extremities.
All possible symptoms can be roughly classified into 4 types of syndromes: cardiac, vertebral, radicular (nervous) and vertebral artery syndrome (with circulatory disorders).
Spinal syndrome:
- crunching in the neck when turning/tilting the head;
- as the disease progresses, pain and difficulty moving occur;
- morphological structural disturbances in the vertebral body and intervertebral space (visible on x-ray).
Cardiac syndrome:
- shortness of breath, weakness;
- feeling of incomplete inspiration, lack of air;
- spontaneous phenomena from the cardiovascular system - angina pectoris, chest pain, burning sensation;
Radicular syndrome:
- numbness of the tongue, shoulders, fingers, occipital region;
- difficulty swallowing;
- discomfort in the area between the shoulder blades;
- headache in the back of the head and forehead.
Vertebral artery syndrome:
- unreasonable jumps in blood pressure;
- dizziness, up to loss of consciousness;
- tinnitus, feeling of cotton wool in the head;
- temporary one-sided blindness, “spots” in the eyes;
- periodic attacks of nausea, especially when moving the head;
- headaches - mainly in the back of the head, as well as migraines;
- drowsiness, decreased performance, memory, concentration, depression.
Attention!
All of these syndromes must be combined with each other. The absence of symptoms of one of them may be a reason for differential diagnosis with other groups of diseases.
Massage
A properly performed massage of the cervical-collar area can alleviate the condition, relieve muscle spasms, and improve mobility. Restrictions for the procedure are:
- pathology of the cardiovascular system in the stage of decompensation;
- tumor formations;
- skin diseases;
- exacerbation of chronic somatic pathologies;
- osteomyelitis.
Experienced massage therapists work at the Yusupov Hospital. The course of treatment is selected individually. Its average duration is 10-15 sessions.
Causes of cervical osteochondrosis
Dystrophic phenomena in the cervical spine are associated with the vertical position of the skeleton and the specific distribution of static and dynamic loads, which largely depend on the prevailing posture and the degree of development of skeletal muscles.
Main reasons:
- lack of movement - what does not develop - degrades: muscles weaken, tissues are destroyed;
- incorrect static postures - muscle tension leads to poor circulation with subsequent tissue degeneration;
- lack of nutrition or unbalanced diet - the body must receive everything it needs to build and renew the bone and cartilage structures of the skeleton, maintain muscle tone;
- obesity, overweight, carrying heavy loads – increases the load on skeletal structures;
- constant nervous tension and nervous stress;
- hypothermia of the cervical region - “got a cold”, “bloated” - provokes hidden inflammatory processes;
- the presence of autoimmune diseases involving cartilage tissue leads to its premature destruction;
- endocrine pathologies disrupt mineral metabolism, reduce the absorption of calcium, silicon, phosphorus and other elements of osteochondral tissue;
- cervical injuries;
- congenital anomalies of the spine and adjacent muscles.
Contraindications to osteotherapy.
Osteopathic science uses gentle means of regulating the internal processes of the spinal region. Limitations in its use are due only to the presence of chronic diseases and the individual characteristics of the patient’s body.
Osteopathy is used with caution when:
- Oncological processes.
- Foci of infection.
- Some types of psychiatric disorders
An alternative to osteopathy for these contraindications can be massage or therapeutic exercises.
Diagnostics
Making a diagnosis of “osteochondrosis of the cervical vertebra” is complicated by the low specificity of symptoms and the wide variety of their manifestations. During the examination, you will need to consult a neurologist, surgeon, orthopedist, and cardiologist.
A physical examination is performed by a doctor and the patient is interviewed. The main diagnostic burden lies on instrumental and laboratory research methods.
Instrumental diagnostics:
- X-ray of the cervical spine; at the initial stage of the process, an MRI of the cervical spine will be more informative - it will provide high-quality visualization of hard and soft tissues - it will show the condition of the intervertebral discs, the presence of osteophytes, deformations, damage to nerve roots and blood vessels; assess the condition of ligaments, muscles, bone tissue;
- Ultrasound shows the dynamic state of soft tissues;
- Dopplerography of the neck vessels will help assess hemodynamics and the degree of damage to the blood vessels (in particular, the condition of the vertebral artery);
- contrast myelography - will help if there is a suspicion of pinched nerve processes;
- ECG and echocardiography of the heart are used in the differential diagnosis of cardiac syndrome and cardiovascular diseases.
How to treat cervical osteochondrosis
A set of therapeutic measures is formed taking into account the stage of the disease (acute, chronic), the degree of damage and the causes of the development of pathology. Conservative treatment, surgical intervention, and a mixed approach are used.
Conservative impact
It represents a gradual restoration or compensation of damage against the background of symptomatic treatment. Includes drug therapy, physiotherapy, exercise therapy and massage methods.
Drug treatment:
- painkillers - mainly local gels and ointments; in severe cases - general painkillers in the form of tablets;
- anti-inflammatory drugs - NSAIDs, as well as corticosteroids (short course if necessary);
- medications to improve microcirculation and blood circulation in general;
- chondroprotectors – means for the protection and restoration of cartilage tissue;
- muscle relaxants - to eliminate muscle tension and spasms;
- vitamin and microelement complexes - necessary for nutrition and support of tissues with building elements.
As acute symptoms subside, methods of physiotherapy, exercise therapy and self-massage are used.
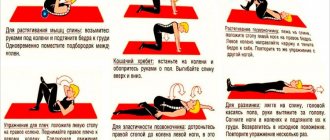
Therapeutic exercises improve the nutrition of cartilage and bone tissue by restoring blood supply to the damaged area. To avoid complications, it is recommended to use the method of isometric movements, when instead of real turns and tilts of the head, which can cause damage, their imitation is used.
Attention!
All actions should be performed only after diagnosis and consultation with a doctor.
The technique allows you to develop and strengthen the atrophied short muscles of the neck and stabilize the position of the cervical spine. Sequence of basic exercises:
- Place the palm of your right hand on the side of your head - for 10 seconds, press your palm on your head, while simultaneously straining the muscles of your head and neck for resistance - your head should remain motionless.
- Lower your hand and relax the muscles of your head and neck as much as possible for 20 seconds.
- Repeat the exercise with your left hand.
- Place both hands with your palms on your forehead - for 10 seconds, press on your forehead as if trying to tilt your head back, while simultaneously straining your neck muscles to resist the movement. The head should remain motionless.
- Lower your arms, relaxing your muscles as much as possible, similar to the previous exercise.
- Place both palms in the area above the back of your head. By analogy, apply pressure to the neck muscles, trying to tilt your head forward - it should still be motionless.
- Lower your arms, relax the muscles of your neck and head. Repeat the set of exercises 4-10 times.
After strengthening the short neck muscles, you can begin performing dynamic exercises.
On a note!
Swimming and water gymnastics have proven themselves well as methods for restoring mobility of the cervical spine.
Self-massage allows you to reduce the intensity of local reactions and relieve muscle tension during static work. Execution rules:
- area of influence - the back of the head, back and sides of the neck;
- carry out the procedure in a sitting position;
- movements should be performed in the direction from the spine;
- use only your fingertips;
- avoid putting pressure on inflamed areas;
- Perform movements smoothly - sudden pressure can cause harm.
Physiotherapy procedures are typical for inpatient treatment and sanatorium-resort rehabilitation. Well proven:
- electrophoresis – warms up the area, improves microcirculation, and is used for deeper penetration of topical drugs;
- magnetic therapy;
- amplipulse;
- UHF.
Surgical intervention is indicated for complicated extrusions, spinal cord entrapment and intractable pain syndromes.
Prevention and rehabilitation for neck osteochondrosis.
Cervical osteochondrosis is a multifaceted problem that affects many organic elements. Preventive actions concern the system as a whole. At the first signs of cervical osteochondrosis, you need to go to a therapist, he will conduct an examination, prescribe a diagnosis and refer you to one of the specialized specialists, including a traumatologist, neurologist, or orthopedist. You must take the test results with you to the Osteopathy Clinic.
The disease can be eliminated not only with specific treatment, but also with the right lifestyle and auxiliary means: exercise therapy, massage, therapeutic exercises.
To cure or eliminate the negative consequences of the disease, it is important to ensure:
- Active lifestyle, physical education. During the remission stage, moderate gymnastics and a complex of physical therapy (physical therapy) are useful. Classes are best done under the guidance of an instructor.
- Regular meals, diet. There are a number of foods you should avoid. Salty, fatty, spicy foods are excluded from the diet.
- Reducing excess weight reduces the load on the cervical segment of the skeleton and increases joint mobility.
- Protection against colds and inflammation in the cervical direction
- Be careful during physical labor and sports exercises. A sharp or awkward movement of the cervical section injures the joints and blocks the mobility of the skeletal structure.
- If osteochondrosis of the neck is in the acute stage, you should consult a doctor to treat the disease: he will decide which option of auxiliary support is preferable.
If you have injuries or if symptoms of chronic or inflammatory processes appear, you should contact a specialized specialist.
Why is cervical osteochondrosis dangerous?
The neck area concentrates a dense interweaving of major blood vessels, nerve processes and dynamic skeletal structures. Without treatment, serious pathological changes can be observed:
- weakening of the fibrous ring provokes dislocations and subluxations in the area of the most mobile vertebrae;
- the presence of osteophytes and muscle spasms leads to pinching of nerve roots and blood vessels with the formation of compression syndromes;
- destruction of cartilaginous discs and convergence of the vertebrae leads to intervertebral hernia with pinching of nervous tissue.
Each of these phenomena is followed by a pronounced negative reaction from the whole organism.
Possible complications and consequences
The list of the most common complications of cervical osteochondrosis includes:
- vegetative-vascular dystonia;
- hypertension;
- oxygen starvation of the brain and its structures;
- retinal dystrophy with visual impairment;
- malfunction of the thyroid gland;
- dysfunction of the esophagus and trachea - difficulty swallowing and respiratory spasms;
- intractable pain syndrome in the head, neck, chest, upper limbs;
- cramps and numbness of the face, hands;
- disruption of the hypothalamic-pituitary system, which entails a disruption of all hormonal activities of the body.
Preventive measures
The most effective treatment is disease prevention. Prevention will help you with this. It is enough to follow a few basic recommendations:
- correct your posture,
- create a comfortable workplace;
- during sedentary work, take breaks for “physical education”;
- include in your diet foods rich in calcium, magnesium, phosphorus, silicon - fish, nuts, seeds, legumes, dairy products, fresh vegetables, fruits; limit the consumption of salt, sweets, flour and spicy foods;
- for sleep and rest, use an orthopedic mattress and pillow;
- take up a non-strength sport - it is better to give preference to swimming.
Even if you are not able to take into account all the requirements, moderate physical activity, proper nutrition and careful attention to your posture can significantly reduce the risk of developing pathology.