What is radiculopathy
Against the background of lumbar osteochondrosis, a disease such as radiculopathy of the lumbosacral spine very often develops.
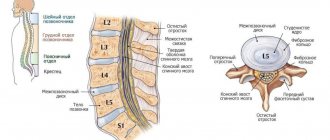
This is a clinical syndrome that occurs due to compression and damage to the nerve roots. A synonym for radiculopathy is radiculitis. Radiculitis (radiculopathy, from the Latin radicula - root) is a disease of the human peripheral nervous system that occurs as a result of damage, inflammation or pinching of the spinal nerve roots.
Radiculitis is a widespread disease, it affects more than 10% of the population of our planet over 40-50 years of age, and in the last decade, radiculitis has become younger, occurring in the young age group from 25 to 35 years old, people involved in professional sports, as well as those who are especially susceptible, are especially susceptible. who sits at a computer or driving a car for a long time.
Preventive measures:
- active lifestyle, regular sports and swimming;
- avoiding hypothermia and excessive stress;
- correct load distribution when lifting and carrying heavy objects;
- balanced healthy diet;
- proper organization of the workplace, purchasing ergonomic furniture;
- timely seeking help for diseases of the musculoskeletal system.
At the CELT clinic they know how to return you to normal life! If you are tired of enduring pain, contact us!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Causes of radiculitis
The cause of the development of radiculitis is pathological processes occurring in the spine, namely:
- Degenerative-dystrophic processes - osteochondrosis and its complications: protrusion and herniation of intervertebral discs
- Malformations of the musculoskeletal system, accompanied by changes in muscle tone
- Poor posture, curvature of the spine - scoliosis
- Incorrect distribution of physical stress on the spinal column during a person’s professional activity (when driving a car, office workers and loaders - when they stay in one position for a long time, loaders)
- A sedentary lifestyle, in which disturbances in the blood supply to the muscles of the lumbar region gradually increase
- Improper drinking regime throughout the day and for several months
- Deficiency of vitamins and minerals leads to osteoporosis and trophic lesions of the nerve fiber
- Tuberculosis, osteomyelitis, chronic syphilis and other types of infectious lesions of the spinal cord
- Regular injuries to the vertebrae and surrounding soft tissues (impacts, sharp twists, compression when jumping, sprains of the ligaments)
- Overweight with obesity of 1-2 degrees and the presence of bad habits such as smoking, abuse of tea, coffee and alcoholic beverages
Surgical intervention
Operations for diseases of the spine
- Cost: 100,000 - 250,000 rubles.
- Duration: 40-60 minutes
- Hospitalization: 2-3 days in hospital
More details
Surgical intervention is carried out exclusively according to indications:
- lack of effect from conservative treatment;
- inhibition of tendon reflexes;
- feeling of weakness in the lower limb;
- decreased sensitivity of the lower limb.
Neurosurgeons at the CELT multidisciplinary clinic perform gentle operations through micro-incisions or punctures while preserving all supporting structures of the spine. Three-dimensional modeling of the operation and planning of each stage are carried out in advance. The process uses microsurgical and endoscopic techniques, laser and ultrasound, which allows our patients to quickly recover and return to work within two to three weeks after surgery.
Symptoms of radiculitis
The first manifestations and main permanent symptoms of radiculitis of the lumbosacral spine are pain, impaired sensitivity and muscle weakness.
The affected area corresponds to the innervation zone. Depending on the affected area, pain can be observed in the lumbar and gluteal regions, the posterolateral and anterior part of the thigh, along the anterior outer surface of the lower leg, on the dorsum of the foot, big toe, in the calf muscle, in the area of the outer ankle and heel.
Lumbosacral radiculitis is often chronic, with acute relapses. Lumbosacral radiculitis is characterized by increased pain when the body suddenly changes from a horizontal to a vertical position or vice versa, as well as when engaging in an active lifestyle (sports, walks, fitness classes).
Exacerbation of pain syndrome in radiculopathy of the lumbosacral region is observed when the interradicular nerve is compressed by an intervertebral hernia.
According to the types of radiculopathy of the lumbosacral spine, there are:
- Lumbago (lumbodynia) is acute pain in the lower back during sudden physical exertion, and also provoked by overheating or hypothermia of the body. The painful attack itself can last in different ways: from several minutes to several hours and even days. The main cause of this type of radiculopathy is muscle strain in the lumbar region, intervertebral hernia or displacement of the vertebrae relative to each other.
- Sciatica (sciatica) - with this type of radiculitis, pain is localized in the buttock, on the back of the thigh and lower leg and can reach the foot. Sometimes, in addition to pain, muscle weakness is noted. This is due to damage or irritation to the sciatic nerve, the largest nerve in the body. The pain with sciatica is shooting, like an electric shock; burning, tingling, “pins and needles” and numbness are also possible at the same time. Pain of varying degrees of intensity is possible: from mild to very intense, such that the patient cannot sleep, sit, stand, walk, bend or turn.
- Lumboischialgia is lower back pain radiating to the leg or legs. With this type of radiculitis, the pain spreads mainly along the buttock and along the posterior surface of the leg, without reaching the toes; most often it is an aching, burning, growing pain.
Drug treatment
Non-steroidal anti-inflammatory drugs (NSAIDs) are prescribed to relieve acute pain, inflammation and muscle spasms. These are drugs based on diclofenac, nimesulide, ibuprofen, meloxicam. The choice of dosage form depends on the intensity of the symptoms: severe pain is eliminated with intramuscular injections, moderate pain can be relieved with tablets. In the acute period, local agents - ointments, gels and creams - can additionally be used. The second choice drugs are steroids - Hydrocortisone, Dexamethasone, Diprospan. They have a powerful anti-inflammatory effect. If NSAIDs with hormones are ineffective, then therapeutic blockades with Lidocaine and Novocaine are performed.
Antispasmodics and muscle relaxants (Mydocalm) help relax spasmodic muscles. If swelling is present, diuretics and magnesium sulfate are prescribed. Swollen tissues put additional pressure on the nerve, so removing excess fluid greatly alleviates the condition. To enhance the effect of analgesics and normalize the functioning of the nervous system, sedatives are added. Treatment of lumbar radiculitis also includes B vitamins, which improve nerve conduction. The most commonly used are Milgamma and Neuromultivit. If the disease is of non-infectious origin, then ointments with a warming effect can be prescribed - based on turpentine, snake and bee venoms, camphor. They relieve pain due to local irritant action.
Diagnostics
For the diagnosis of radiculopathy, the presence of tension symptoms is important. For example, Lasegue's symptom is typical - when you try to raise a straight leg while lying on your back, pain in the lower back increases.
An MRI or CT scan of the lumbosacral spine is important for making a correct diagnosis, because only these studies will allow the attending physician to identify the presence of diseases such as intervertebral hernias or other diseases of the spine (spondylitis, compression fractures, neoplasms).
Which doctor should I contact?
Neurologists are involved in the diagnosis and treatment of radiculitis; if necessary, other specialized specialists are involved - vertebrologists, orthopedic traumatologists, and neurosurgeons. Complex therapy can be carried out with the participation of a chiropractor, physical therapist and reflexologist.
1.General information
In everyday life, you can often meet a person who winces from a sudden pain, say, in the neck and involuntarily rubs the sore spot with the doomed and vexed words: “Osteochondrosis has tormented me” (sometimes even such a fantastic diagnosis as “acute melancholy” sounds). We call similar sensations in the lower back “lumbago,” “lumbago,” or “sciatica.” The last word, which has long migrated from medical vocabulary into common use, fairly closely (albeit incompletely) reflects the essence of the problem: the suffix “-itis” indicating inflammation follows the Latin stem, which means “root” and from which the word “radical” is also derived. (in mathematical, political and any other sense). Hence the synonymous name: radicular syndrome.
In its full version, the diagnosis sounds most accurate: vertebrogenic (discogenic) radiculopathy. A reader who has long and carefully been interested in medicine will immediately notice that in this terminological evolution the “inflammatory” suffix has disappeared - instead, “-pathy” has appeared, that is, suffering, illness, pathology itself. Indeed, in the light of modern nosological concepts, inflammation is not an obligatory, obligatory symptom for radiculopathy: almost the same clinical picture develops with any compression, pinching, failure of conduction functions, or circulatory disorders in the radicular nerve endings of the spinal cord.
And if earlier the word “radiculitis” was steadily associated with the image of an elderly man, bent in an unnatural forced position and holding his lower back with his palm, wrapped in a warm scarf, then modern radiculopathy is rapidly “rejuvenating”. To date, the prevalence of vertebrogenic radiculopathies, according to WHO statistics, has exceeded 12%; The proportion of young people among those initially ill is constantly increasing, and this alarming trend, alas, is quite natural.
A must read! Help with treatment and hospitalization!
Risk factors
Those most at risk of developing radiculitis are:
- representatives of professions characterized by high physical activity (athletes, miners, loaders);
- specialists whose work involves standing in one place for a long time (dentists, surgeons, machine operators, salespeople, managers, etc.);
- office workers who have to sit for long periods of time;
- drivers whose spine is exposed to prolonged vibration, etc.
Forecast and prevention of the disease
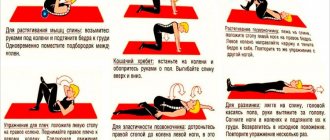
It is necessary to recommend that the patient return to normal daily activities as quickly as possible, since maladaptive pain behavior is the main barrier to recovery. In addition, comorbid depression also negatively affects treatment outcomes. If pain persists for >4–6 weeks, it is advisable to add antidepressants to analgesic therapy. Pathogenetically, it is most justified to use antidepressants that act on both neurotransmitter systems (serotonin and noradrenergic) for the treatment of pain symptoms. Tricyclic antidepressants (TCAs), which block the reuptake of serotonin and norepinephrine, have greater potential than selective antidepressants. TCAs are more successful in treating pain symptoms and leading to more complete remission of depression. A new class of drugs, dual-action antidepressants that block the reuptake of serotonin and norepinephrine, have high analgesic efficacy and a more favorable spectrum of side effects than TCAs. The effectiveness/safety ratio is optimal for dual-acting antidepressants (duloxetine, venlafaxine). During the recovery period, active exercises are recommended to strengthen the muscle corset.
Treatment of radiculitis at home using the NANOPLAST forte therapeutic patch
used in the therapeutic treatment of radiculitis , such as NSAIDs, muscle relaxants, etc., certainly alleviate the patient’s condition, but with prolonged use they can cause harm to the body. And for some gastrointestinal diseases, many drugs are generally contraindicated.
But now it is possible to minimize side effects and at the same time increase the effectiveness of sciatica treatment. A new generation drug can help with this - the pain-relieving anti-inflammatory medical patch NANOPLAST forte .
In the treatment of radiculitis, the therapeutic plaster NANOPLAST forte in many cases shows very good results:
- helps relieve pain and inflammation,
- improve blood circulation in the affected area, which ensures active restoration of damaged tissues;
- makes it possible to reduce the dose of painkillers and anti-inflammatory drugs, and in some cases, cancel them altogether.
For radiculitis , the therapeutic plaster NANOPLAST forte is applied to the neck, cervico-brachial region, lower back or intercostal area - depending on the location of the pain. It is usually recommended to use the patch in the morning for 12 hours, but it can also be used at night. The duration of the course of treatment of radiculitis with a medicinal patch is from 9 days
High efficiency, absence of harmful side effects, long-term (up to 12 hours!) therapeutic effects, ease of use and affordable price make NANOPLAST forte the drug of choice in the treatment of radiculitis.
Read more about NANOPLAST forte