Neck pain can have many causes. But in many cases, pain occurs due to old age. Like other bones in the body, the bones of the spine degenerate with age and cause various problems in the structure of the spine. If this injury occurs in the neck area, it is called cervical spondylosis.
Cervical spondylosis is very common. More than 85% of people over 60 years of age suffer from this disease. This condition often causes pain and stiffness in the neck. Familiarity with the symptoms, methods of prevention, treatment and prevention of the growth of this disease will improve the quality of life of people.
What are the most important causes of neck osteoarthritis?
Cervical spondylosis is caused by age-related changes in the bone tissue of the spine. These changes are completely normal and occur in all older people. About half of middle-aged and older people have degenerative bones in the spine but do not have annoying or painful symptoms. Some of the most important causes of cervical spondylosis are:
Disc degeneration
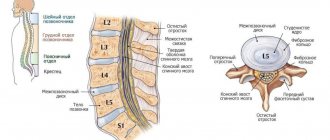
As we age, the intervertebral discs in the spine lose their thickness and become deformed. In some cases, the water inside them dries out and its thickness decreases. In this case, the lateral pressure of the discs and vertebrae gradually increases, causing destruction and spondylosis of the cervix.
Disc herniation
Natural aging can cause the outer part of the spinal disc to crack. In this condition, the inner part of the disc is removed, which is called a herniated disc or herniation. The hernia puts pressure on nearby tissue or the spinal nerve, and this pressure is the main cause of pain, tingling or numbness.
Osteophyte
Smooth and slippery articular cartilage covers and protects joints. This cartilage will also gradually wear down as you age. If the cartilage is completely worn down, the bones can wear against each other. To replace the lost cartilage, new bone is made to replace the joints to support the vertebrae. Over time, this bone grows so large that it is called a bone spur. Excessive growth of bone spurs can narrow the passage of nerves and the spinal cord and cause cervical spondylosis.
Neck injuries
Injuries to the neck due to accidents such as falls or accidents can lead to faster destruction of the vertebrae and premature aging, leading to osteoarthritis of the neck.
Ligament stiffness
Ligaments are strong cords that connect the bones of your spinal cord. If the ligaments become tight over time, they will affect the movement of your neck, causing pain and cervical spondylosis.
Excessive pressure on the neck
Some jobs or sports involve repetitive, heavy movements of the neck, which place additional stress on the spine, leading to premature wear and tear and osteoarthritis of the neck.
Pathogenesis
The cervical spine consists of 7 vertebrae. Between them are intervertebral discs that are elastic. They are necessary to cushion the vertebrae during movement. The discs have a rigid fibrous ring and a core that is supported by it, thereby preventing protrusion.
The spine is protected and strengthened by muscles. The anterior longitudinal ligament, which is considered one of the largest, runs along the anterior surface of the vertebrae. During the development of cervical spondylosis, the fibrous ring gradually loses its rigidity, and the nucleus pulposus protrudes towards this ligament. This leads to the appearance of ossification on the vertebra, and then bone growths.
Discomfort in this case is associated with an increase in the tone of nearby muscles, inflammation in the area of fascia, ligaments, as well as joint blockades. Over time, the height of the intervertebral discs decreases, mobility is limited, and ankylosis of small joints occurs. Nerve roots may also be compressed, causing neurological symptoms.
Who is most at risk for cervical spondylosis?
Older people are more likely to get cervical spondylosis because it is associated with old age. But other people are also susceptible to diseases. Including:
- Those who smoke.
- Depressed and anxious people
- People with genetic ancestry
- People with a history of previous injuries from an accident
- Construction painters who stare at your head for hours every day, or plumbers and floor installers who keep their heads down for long periods of time.
- People who hold their head in an awkward position for a long time, for example, stare at a computer screen for a long time.
- Construction workers do hard work.
- Bus or truck drivers who are exposed to vibration for long periods of time.
Possible complications
In the absence of timely treatment, thoracic spondylosis can cause respiratory dysfunction and compression of internal organs. In addition, other complications are also dangerous:
- Unbearable pain that can only be relieved by epidural blockades.
- Formation of protrusions and intervertebral hernias.
- Impaired motor activity, paralysis.
- Urinary incontinence or spontaneous bowel movements.
- Spinal stenosis.
- Sexual dysfunction.
The degenerative processes that spondylosis provokes are irreversible, so treatment can be started as early as possible. Conservative treatment, physiotherapy and exercise therapy can only temporarily slow down the process and ensure stable remission.
Recognize the symptoms of cervical spondylosis
Most people have no symptoms of cervical spondylosis, but it usually presents with neck pain and stiffness if symptoms do occur. This pain can be mild or severe.
Sometimes the pain gets worse when you look up, look straight ahead, or do activities that require your neck to remain in that position for a long time, such as driving a car or reading a book. These pains intensify when resting or lying down.
But other symptoms may indicate neck osteoarthritis. Such as headache, dizziness, splitting sound when turning, muscle spasms in the neck and shoulders.
A common symptom of cervical spondylosis is pain around the shoulder blade. Some complain of pain in the arm and fingers. This pain may worsen with standing, sitting, sneezing, coughing, and bending the neck backward.
In some cases, cervical spondylosis leads to narrowing of the spinal cord and nerve roots. In this case, it will be accompanied by symptoms such as numbness and weakness in the arms, hands and fingers, difficulty walking, loss of balance, lack of control over urination and bowel movements, and weakness in the arms or legs.
Symptoms
There are no characteristic signs of the disease, so it is often confused with osteochondrosis or spondylitis. At the initial stage there are practically no manifestations. It is often discovered by accident, during a medical examination or professional medical examination. As it progresses, patients may notice the following symptoms:
- Unpleasant sensations in the area of the ribs or shoulder blades.
- Piercing pain in the region of the heart.
- Heaviness, tightness and pain, reminiscent of angina pectoris.
- Feeling of lack of air, shortness of breath even with minimal exertion.
- Numbness or tingling of fingers.
- Muscle tension and tightness in the upper back.
- Decreased motor function of the upper limbs.
- Deterioration of general condition when the weather changes.
- Rapid fatigue, even with minor exertion.
- Increased symptoms in the evening.
The symptoms of the disease are similar to spondylopathy, so without specifying the condition, this is exactly the diagnosis they make. As the pathological process develops, it may affect the functioning of the heart muscle, or neighboring organs, or the pulmonary part. The pain syndrome varies; some patients complain of acute attacks, others of an unpleasant aching sensation. As the lesion spreads, the pain is accompanied by squeezing or slight tingling in the chest.
Osteophytes are clearly visible on x-ray
Methods for diagnosing cervical spondylosis by doctors
When a person consults an orthopedist with neck pain, the first step, after a medical history, is that the doctor conducts a clinical examination of the shoulders, neck, arms and legs. It tests hand and finger strength, strength of touch, reflexes, blood flow, gait balance and more. He then creates a pain history.
In the second step, the doctor may order diagnostic tests to make sure that the patient has cervical spondylosis. These tests include the following.
- X-rays show the neck bones, their alignment, bone loss, and bone spurs.
- Computed tomography (CT) scans provide more detail than X-rays. This scan will help you see the spinal cord and bone spurs better.
- MRI images show details of soft tissues such as cartilage, nerve roots, muscles, spinal cord and discs. This test can show spinal compression or a herniated disc more clearly than x-rays. MRI electromyography can help determine the source and location of pain.
- Other tests may include myelograms (computed tomography scans) or electromyograms (nerve function tests). These tests provide more detailed information about the effects of cervical spondylosis on your nerves.
Physical examination
First, the doctor finds out the presence of symptoms, their intensity, location, and history of the disease. A neurological examination is then performed, which includes examining reflexes, testing muscle strength, and determining sensory deficits and range of motion in the neck. A doctor may perform a gait analysis to determine how much damage to the spinal cord is present.
If a doctor suspects cervical spondylosis, he will order imaging tests and neurophysiological studies to verify the diagnosis.
Treatment of cervical spondylosis
When a doctor diagnoses cervical spondylosis, patients are given various treatments depending on the severity of the disease.
Non-surgical treatment
In most cases, treatment for cervical spondylosis is non-surgical.
During the first stage of treatment, the doctor prescribes several medications to relieve both pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are often prescribed along with acetaminophen to relieve pain. Medicines such as cyclobenzaprine or carisoprodol are used to treat painful muscle spasms.
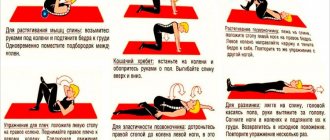
Physical therapy is a non-surgical treatment option recommended by doctors. Specific exercises can help relieve pain and strengthen and stretch weak muscles.
Home treatments for cervical spondylosis include the use of cervical guards, which restrict neck movement, as well as massage and hot and cold compresses to relieve pain.
Steroid injections are also one way to reduce inflammation and pain in the neck, which is very rare and is recommended by doctors for certain conditions.
Why do osteophytes appear?
If the muscles and ligaments are weakened, then the neighboring vertebrae become unstable and begin to “play” - shift relative to each other. The receptors are constantly irritated, causing pain. To avoid this discomfort, the body tries to cope with the problem on its own by fixing the spine, increasing the contact area of the vertebrae by building up bone tissue and compressing muscles. Thus, the course of the disease provides the key to the solution - improving the condition of the muscles is very important in order to avoid the formation of osteophytes.
Surgery
Surgery is not usually used for cervical spondylosis unless the condition is specific. For example, when the spinal cord and nerves are under pressure and the patient has progressive neurological symptoms such as arm weakness and anesthesia.
Surgery may also be recommended if you have severe pain that does not improve with non-surgical treatments. However, some patients with severe neck pain will not be candidates for surgery, which may be due to the advanced nature of their osteoarthritis, other medical problems, or other causes of their pain, such as fibromyalgia.
Types and stages of the disease
There are many varieties of this disease. According to the presence of complications, spondylosis is distinguished:
- Uncomplicated – the disease does not progress quickly and has mild symptoms.
- Complicated - osteophytes grow rapidly, the vertebrae are destroyed at a high rate.
Treatment and prevention of cervical spondylosis are necessary in any situation, but the uncomplicated form will be easier to respond to therapeutic interventions. According to the nature of the pathology, spondylosis can be distinguished:
- slow;
- moderate;
- fast;
- fulminant.
The last type is the rarest, but it is also the most dangerous. It is the most difficult to treat because it is the least responsive to medical treatment. There are also two stages of the disease:
- X-ray – here you can identify violations of the structure of the vertebrae and discs, the occurrence of osteophytes.
- Functional deficiency - here everything is assessed as a whole, all internal consequences. A commission often meets to determine a person’s level of ability to work.
If the condition is advanced, then conservative treatment will most likely not produce results and you will have to resort to radical measures.
How can you prevent cervical spondylosis?
Cervical spondylosis caused by aging cannot be prevented, but you can reduce your risk of developing it if you follow some guidelines.
- Try to be in the best physical position when standing, sitting and sleeping
- Exercise regularly When playing sports, always use appropriate sports equipment. supervision of a trainer.
- Beware of blows to the neck.
Facts About Cervical Spondylosis
Cervical spondylosis is more common in older people, but in many cases there are no symptoms and the person will never notice the disease.
Patients with cervical spondylosis are usually not disabled and do not require extensive treatment, and if pain occurs, it can be treated with physical therapy and certain medications. But sometimes changes in the spine can compress the spinal cord or the nerve roots attached to it, in which case the person will suffer from numbness, imbalance and similar problems. In these cases, doctors use surgical methods to solve the patient's problem, which is very rare.
In what cases should you visit a specialist?
If shoulder numbness or tingling suddenly appears, paresthesia in the upper or lower extremities, or loss of bowel control, it is important to visit a doctor as soon as possible for diagnosis and appropriate treatment.
If pain and discomfort are so severe that they interfere with a person’s ability to live fully, an early consultation with a neurologist is needed. Even despite the age-related changes, there are currently medications and other measures that can make a person’s life easier and restore his ability to work.