Treatment tactics
Treatment of pulmonary artery diseases depends on the severity of the process. As for stenosis, in the absence of pronounced manifestations, there is no need for surgical intervention, but clinical observation and symptomatic therapy are required.
As the pathology progresses, the question of surgical treatment arises. When the pressure gradient increases above 50 mmHg, the question of surgery is not discussed - it must be performed immediately. Operation options are different. Valvuloplasty can be open, closed, endoscopic - balloon. Indications for a specific intervention are determined by a specialist.
The main directions in the treatment of pulmonary hypertension are the prevention of thrombosis, elimination of spasm of vascular smooth muscle fibers, stopping the proliferation of connective tissue structures of the vascular wall. In this case, the following application is indicated:
· drugs that normalize blood clotting;
· diuretics;
cardiac glycosides;
· vasodilators;
· oxygen therapy.
In case of hypertension, called secondary, complex measures should correct the underlying pathology - the root cause of the increase in pressure in the artery. The list often includes bronchodilators and corticosteroids.
Surgical treatment for hypertension: embolectomy, lung transplant, pulmonary-cardiac complex transplant.
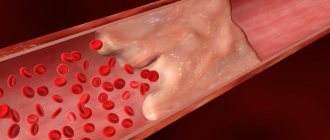
Pulmonary embolism (PE)
The symptoms of pulmonary embolism depend on the number and size of thrombosed pulmonary arteries, the rate of development of thromboembolism, the degree of disturbances in the blood supply to the lung tissue, and the initial condition of the patient. With PE there is a wide range of clinical conditions: from practically asymptomatic to sudden death.
The clinical manifestations of pulmonary embolism are nonspecific; they can be observed in other pulmonary and cardiovascular diseases; their main difference is the sharp, sudden onset in the absence of other visible causes of this condition (cardiovascular failure, myocardial infarction, pneumonia, etc.). The classic version of PE is characterized by a number of syndromes:
1. Cardiovascular
:
- acute vascular insufficiency. There is a drop in blood pressure (collapse, circulatory shock), tachycardia. Heart rate can reach more than 100 beats. in a minute.
- acute coronary insufficiency (in 15-25% of patients). It manifests itself as sudden severe chest pain of various types, lasting from several minutes to several hours, atrial fibrillation, and extrasystole.
- acute cor pulmonale. Caused by massive or submassive pulmonary embolism; manifested by tachycardia, swelling (pulsation) of the neck veins, positive venous pulse. Edema does not develop in acute cor pulmonale.
- acute cerebrovascular insufficiency. General cerebral or focal disorders, cerebral hypoxia occur, and in severe cases - cerebral edema, cerebral hemorrhages. Manifested by dizziness, tinnitus, deep fainting with convulsions, vomiting, bradycardia or coma. Psychomotor agitation, hemiparesis, polyneuritis, and meningeal symptoms may be observed.
2. Pulmonary-pleural
:
- acute respiratory failure is manifested by shortness of breath (from a feeling of lack of air to very pronounced manifestations). The number of respirations is more than 30-40 per minute, cyanosis is noted, the skin is ashy-gray and pale.
- moderate bronchospastic syndrome is accompanied by dry wheezing.
- pulmonary infarction, infarction pneumonia develops 1–3 days after pulmonary embolism. There are complaints of shortness of breath, cough, chest pain on the affected side, aggravated by breathing; hemoptysis, increased body temperature. Fine bubble moist rales and pleural friction noise become audible. Patients with severe heart failure have significant pleural effusions.
3. Fever syndrome
- subfebrile, febrile body temperature. Associated with inflammatory processes in the lungs and pleura. The duration of fever ranges from 2 to 12 days.
4. Abdominal syndrome
caused by acute, painful swelling of the liver (in combination with intestinal paresis, peritoneal irritation, hiccups). Manifested by acute pain in the right hypochondrium, belching, vomiting.
5. Immunological syndrome
(pulmonitis, recurrent pleurisy, urticaria-like skin rash, eosinophilia, the appearance of circulating immune complexes in the blood) develops at 2-3 weeks of the disease.
Contraindications to CT angiography of the pulmonary arteries
If the patient is pregnant or suspects that she may be pregnant, the doctor must be notified about this, because CT angiography can harm the fetus. CT angiography is also not recommended for women who are currently breastfeeding.
In addition, there is a risk of allergies if there is an individual intolerance to the components of the contrast agent. Patients who experience an allergic reaction to iodine should inform their doctor. Patients suffering from renal failure or other kidney diseases should also tell their radiologist in advance. In addition, the doctor should not be left in the dark if the patient is taking medications and herbal supplements. Contraindications to CT are people with elevated creatinine levels, diabetes mellitus (type II), thyrotoxicosis, and blood clotting problems.
Symptoms of pulmonary hypertension
Signs of pulmonary hypertension appear slowly. They may go unnoticed for months or even years. Symptoms get worse (or more pronounced) as the disease progresses. These include:
- shortness of breath, first during physical activity, and then at rest;
- fatigue;
- dizziness;
- fainting;
- chest pressure or pain;
- swelling of the ankles, legs and eventually the abdomen (ascites);
- bluish color of lips and skin (cyanosis);
- increased pulse and heart rate.
Degrees of pulmonary hypertension
Depending on the stage of development of the disease, its degrees are distinguished.
- Pulmonary hypertension stage 1. There are no clinical manifestations, physical activity is well tolerated, but in some areas of the pulmonary artery there are signs of circulatory disorders that can only be detected with a special examination.
- Pulmonary hypertension 2 degrees. Physical activity begins to bring discomfort. Worried about shortness of breath, weakness, dizziness. At rest I feel normal.
- Pulmonary hypertension grade 3. Even light physical activity causes severe discomfort.
- Pulmonary hypertension grade 4. All symptoms of pulmonary hypertension are felt even at rest; a person cannot lead a normal lifestyle.
Causes and pathogenesis
Pulmonary hypertension is divided into congenital and acquired. Otherwise, these forms are called primary and secondary. Among the causes of increased pressure in the pulmonary artery are the following:
- chronic lung diseases (bronchial asthma, COPD, sarcoidosis, interstitial pulmonary fibrosis, tuberculosis, silicosis, asbestosis)
- heart diseases (heart failure, acquired and congenital heart defects)
- stay in the highlands
- vasculitis
- effects of drugs on the body
- TELA
Pulmonary hypertension without a known cause is called primary hypertension. The cause of PH may be an increase in pressure in the pulmonary veins. Growth is provoked by the following factors:
- left ventricular failure
- mitral valve defects
- pulmonary vein compression
- left atrium myxomas
Increased pulmonary blood flow can also trigger pulmonary hypertension:
- patent ductus arteriosus
- ventricular septal defect
- atrial septal defect
Among the causes of the disease in question is an increase in pulmonary vascular resistance, which can be caused by:
- taking drugs that reduce appetite (fenfluramine) or chemotherapy drugs
- obstruction of the pulmonary artery and its branches
- inflammatory changes in the lung parenchyma
- destruction of the pulmonary vascular bed (with chronic destructive lung diseases, pulmonary emphysema)
- chronic alveolar hypoxia (for example, when staying high in the mountains)
Valvular defects lead to the occurrence of passive PH as a result of the transfer of pressure from the left atrium to the pulmonary veins and then to the pulmonary artery system. With mitral orifice stenosis, there can sometimes be a reflex spasm of the pulmonary arterioles due to increased pressure at the mouths of the pulmonary veins and in the left atrium. Long-term development of PH leads to irreversible sclerotic changes in arterioles and their obliteration.
If a person has congenital heart defects, PH results from increased blood flow in the pulmonary artery system and resistance to blood flow in the pulmonary vessels. Left ventricular failure, which occurs with dilated cardiomyopathy, coronary heart disease, and hypertension, can also cause pulmonary hypertension because the left atrium and pulmonary veins become higher than normal.
In chronic diseases of the respiratory organs, PH for a long period of time has a compensatory nature, because hypoxic pulmonary vasoconstriction turns off non-ventilated areas of the lungs from perfusion, which eliminates the shunting of blood in them, and hypoxemia decreases. At this stage, the use of a drug such as aminophylline reduces pressure in the pulmonary circulation, reduces compensatory vasostriction, and reduces intrapulmonary shunting of blood with deterioration of oxygenation. As lung disease progresses, PH becomes a factor in the pathogenesis of the formation of chronic “pulmonary heart.”
Non-invasive diagnostics
Electrocardiography (ECG) reveals signs of hypertrophy and overload of the right ventricle, dilatation and hypertrophy of the right atrium (p-pulmonale), deviation of the electrical axis of the heart to the right.
Chest X-ray allows you to clarify the etiology of PH: identify interstitial lung diseases, acquired and congenital heart defects, and also judge the severity of PH. The main radiological signs of PH are bulging of the trunk and left branch of the pulmonary artery, which form the second arch in the direct projection along the left contour of the heart, expansion of the roots of the lungs, and enlargement of the right parts of the heart. In patients with post-embolic pulmonary hypertension, signs can be identified that indicate the presence of blood clots in the large branches of the pulmonary artery (PA) - dilation of the trunk and main branches of the PA, a symptom of deformation and shortening of the root. A specific symptom is the depletion of the pulmonary pattern in the area of impaired blood supply.
Echocardiography (EchoCG) - Ultrasound of the heart is considered the most valuable non-invasive method for diagnosing PH, as it not only allows one to assess the level of pressure in the pulmonary artery, but also provides important information about the cause and complications of PH. Using this method, it is possible to exclude damage to the mitral and aortic valves, myocardial disease, congenital heart defects with blood shunting, leading to the development of PH. Unfortunately, the method does not allow differentiating post-embolic pulmonary hypertension from other forms of precapillary PH. The exception is rare cases of the presence of massive thrombi in the trunk and main branches of the pulmonary artery in the immediate vicinity of the bifurcation.
Causes of pulmonary hypertension
Pulmonary hypertension is classified into five groups depending on the cause.
Group 1: pulmonary arterial hypertension.
Reasons include:
- Unknown cause (idiopathic pulmonary arterial hypertension).
- Genetic mutation (hereditary pulmonary arterial hypertension).
- Use of certain prescription diet drugs or illicit drugs.
- Heart problems from birth (congenital heart disease).
- Other conditions such as connective tissue diseases (scleroderma, lupus, etc.), HIV infection, or chronic liver disease (cirrhosis).
Group 2: pulmonary hypertension caused by left-sided heart disease.
Reasons include:
- Left-sided heart valve disease.
- Failure of the lower left chamber of the heart (left ventricle).
Group 3: pulmonary hypertension caused by lung disease.
Reasons include:
- Chronic obstructive pulmonary disease.
- Pulmonary fibrosis.
- Obstructive sleep apnea.
- Prolonged exposure to high altitude in people who are at higher risk of pulmonary hypertension.
Group 4: thromboembolic pulmonary hypertension caused by chronic blood clots.
Reasons include:
- Chronic blood clots in the lungs (pulmonary embolism).
- Other blood clotting disorders.
Group 5: secondary pulmonary hypertension caused by other diseases.
Reasons include:
- Blood diseases.
- Inflammatory diseases.
- Metabolic disorders, including glycogen storage disease.
- Kidney diseases.
- Tumors pressing on the pulmonary arteries.
- Eisenmenger syndrome.
Pulmonary hypertension in children can be of all the forms described above. However, the most common pulmonary arterial hypertension that develops as a result of heart defects and idiopathic pulmonary hypertension occurs in them.
Preparation for CT angiography of the pulmonary arteries
— Three hours before the procedure, you must stop eating or taking pills; only light drinking is allowed.
— The doctor must be provided with the necessary medical documentation and statements with the results of ultrasound, previous CT or MRI studies. This is necessary to ensure that CT angiography is performed with high quality.
— The patient should take care of preliminary blood donation in order to conduct a biochemical analysis that reveals the level of urea and creatinine. To do this, you can provide analysis results no more than two weeks old or take a rapid analysis.
— To get the most accurate result, the patient should remove metal objects and things from the chest area. We are talking about jewelry, clothes with metal fittings or thread, and mobile phones.