Pseudomembranous colitis
The cause of pseudomembranous colitis is a disruption of the normal intestinal microflora, accompanied by excessive proliferation of the opportunistic bacterium Clostridium difficile. In the vast majority of cases, dysbiosis that precedes the development of pseudomembranous colitis occurs while taking antibiotics, but in some cases the composition of the intestinal microflora can change under the influence of cytostatics, immunosuppressants and laxatives.
Most often, pseudomembranous colitis is caused by antibiotics such as clindamycin, amoxicillin, ampicillin, lincomycin and drugs from the cephalosporin group. Less commonly, pseudomembranous colitis develops when taking chloramphenicol, erythromycin, tetracycline and penicillin. Due to the suppression of symbiont microbes, Clostridium difficile begins to multiply in the intestines. These bacteria are found in small quantities in the gastrointestinal tract of approximately 3% of the population.
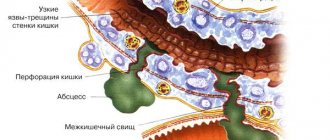
Reproducing clostridia release toxic substances that have a negative effect on the intestinal mucosa and cause the development of pseudomembranous colitis. Some antibiotics enhance the damaging effects of toxins, which further aggravates the resulting disorders. The intestinal wall loses its barrier properties and begins to intensively secrete fluid into the intestinal lumen. Toxic compounds are absorbed into the body, causing the development of intoxication. Fluid moves into the intestinal lumen, dehydration develops, and electrolyte disorders occur.
In severe cases, protein metabolism disorders are detected in patients with pseudomembranous colitis. The cardiovascular system suffers. It is possible to form a toxic megacolon and perforate the intestinal wall with spillage of intestinal contents into the abdominal cavity. The cause of death in pseudomembranous colitis can be peritonitis caused by infection of the abdominal cavity with microorganisms contained in the stool, or dehydration and dysfunction of various organs and systems as a result of intoxication and gross metabolic disorders.
Pseudomembranous colitis can be considered a nosocomial infection. The disease often develops during treatment in a hospital setting, especially when staying in the same ward with patients suffering from this pathology. Factors that increase the likelihood of developing pseudomembranous colitis and at the same time aggravate its course are old age, decompensated somatic diseases, gastrointestinal diseases, uncontrolled use of antacids, renal failure, malignant tumors, immune disorders (including AIDS), weakening of the body after extensive surgical interventions, as well as conditions of various origins requiring intensive care.
Literature
- Alfa MJ, Dul T., Beda G. Survival of incidence of Clostridiulm difficile infection in Canadian hospitals and diagnostic approaches// J. Clin. Microbiol. 1998. V. 36. P. 2076-2080.
- Barbut F., Kajzer C., Planas N., Petit JC Comparison of three enzyme immunoassays, a cytotoxicity assay, and toxigenic culture for the diagnosis of Clostridium difficile-associated diarrhea. J Clin Microbiol 1993;31:963-7.
- Bartlett JG ANTIBIOTIC-ASSOCIATED DIARRHEA N Engl J Med, Vol. 346, No 56: 334-339.
- Dallal MR Fulminant Clostridium difficile: An Underappreciated and Increasing Cause of Death and Complications. Ann Surg. March 2002; 235(3): 363–372.
- Fekety R. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. Am J Gastroenterol 1997;92:739-50.
- George RH, Symonds JM, Dimock F., et al. Identification of Clostridium difficile as a cause of pseudomembranous colitis. BMJ 1978;1:695.
- Hall IC, O'Toole E. Intestinal flora in newborn infants with a description of a new pathogenic anaerobe, Bacillus difficilis. Am J Dis Child 1935; 49:390-402.
- Jacobs J., Rudensky B., Dresner J., et al. Comparison of four laboratory tests for diagnosis of Clostridium difficile–associated diarrhea. Eur J Clin Microbiol Infect Dis 1996;15:561-6.
- Johnson S, Kent SA, O'Leary KJ, et al. Fatal pseudomembranous colitis associated with a variant Clostridium difficile strain not detected by toxin A immunoassay. Ann Intern Med 2001;135:434-8
- Kelly CP, Pothoulakis C, LaMont JT Clostridium difficile colitis. N Engl J Med 1994;330:257-62
- Kelly CP, LaMont JT. Clostridium difficile infection. Annu Rev/Med 1998;49:375-90.
- Kreutzer EW, Milligan FD Treatment of antibiotic-associated pseudomembranous colitis with cholestyramine resin. Johns Hopkins Med J 1978;143:67-72.
- Malnick S., Zimhony O. Treatment of Clostridium difficile–Associated Diarrhea. Ann Pharmacother 2002;36:1767-75.
- Manabe YC, Vinetz JM, Moore RD, Merz C., Carache P., Bartlett JG Clostridium difficile colitis: an efficient clinical approach to diagnosis. Ann Intern Med 1995;123:835-40.
- Mylonakis E., Ryan ET, Calderwood SB Clostridium difficile–associated diarrhea. A review. Arch Intern Med 2001;161:525-33.
- Staneck JL, Weckbach LS, Allen SD, et al. Multicenter evaluation of four methods for Clostridium difficile detection: immunoCard C. difficile, cytotoxin assay, culture, and latex agglutination. J Clin Microbiol 1996;34:2718-21.
- Teasley DG, Gerding DN, Olson MM, et al. Prospective randomized trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhea and colitis. Lancet 1983;2:1043-1046.
- Wenisch C., Parschalk B., Hasenhundl M., Hirschl AM, Graninger W. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis 1996;22:813-8.
- Young G., McDonald M. Antibiotic-associated colitis: why do patients relapse? Gastroenterology 1986;90:1098-1099.
Treatment of the disease at ON CLINIC in Ryazan
Our qualified specialists first of all determine which medications resulted in a side effect in the form of the development of pseudomembranous colitis in the patient. After emergency withdrawal of this drug, it is necessary to suppress the activity of the pathogenic bacteria with the help of antibacterial agents and populate the intestines with normal microflora. In addition, the doctor prescribes medications to restore normal protein metabolism and eliminate imbalances in water and electrolyte disorders. In cases of particularly severe disease with perforation of the intestinal walls, the affected areas of the intestine are surgically removed. If you contact an experienced specialist in a timely manner, the prognosis for the disease is favorable.
Treatment
If the situation is not advanced, the patient is treated with conservative methods - first of all, the fluid supply in the body is restored. Treatment for pseudomembranous colitis also includes:
- Symptomatic treatment. It involves eliminating the symptoms of intoxication, restoring water balance, electrolyte and protein metabolism. Anti-diarrhea medications are not used because they can cause serious side effects.
- Special diet for pseudomembranous colitis. It is immediately therapeutic, and then supportive. For example, at the maintenance stage it is necessary to exclude pickled, fried, smoked, fatty foods, white bread and soda. The doctor will provide the patient with a complete list of prohibited and permitted products.
- Medicines to eliminate the cause of the disease (antibacterial drugs).
- Correction of dysbiosis: prescribing bacterial drugs.
- Surgical intervention. It is used if serious complications begin or conservative methods do not work. During surgery, part of the intestine may be removed, and the intestine itself may be brought into the abdominal cavity - the type of operation depends on the situation.
We recommend entrusting the checking of symptoms and treatment of pseudomembranous colitis to the specialists of JSC "Medicine" - first you need to seek advice from a gastroenterologist or proctologist. Remember that this is an extremely dangerous disease that is much easier to treat in the early stages. The longer the problem develops, the higher the risks of dangerous complications.
Symptoms
In the initial stages, the symptoms of pseudomembranous colitis may not be very varied - usually abdominal pain and diarrhea. As the disease progresses, the number of symptoms increases, so the following appears:
- Regular diarrhea, which debilitates the patient, greatly reduces his quality of life.
- Change in color of stool. They take on a green tint. They also often contain admixtures of mucus and blood.
- Increased amount of urine.
- Dehydration - due to constant diarrhea.
- Increased body temperature, convulsions.
- Weakness, fatigue, headaches.
- Problems with appetite - often the patient simply cannot eat.
- Bloating, cramping pain - as a rule, they are localized on the left side.
- Increased heart rate, decreased blood pressure.
Obviously, such symptoms of pseudomembranous colitis are not specific - they can also occur with other gastrointestinal diseases, so an accurate diagnosis will require a comprehensive, very thorough examination.
Diagnostics
Diagnosis of pseudomembranous colitis begins with examination of the patient and collection of anamnesis. Depending on the complaints the patient presents, the examination is carried out either by a gastroenterologist or a proctologist.
Diagnostics includes taking a smear from the anus, colonoscopy, sigmoidoscopy, endoscopy, abdominal ultrasound (or MRI), and radiography. It is not necessary that all studies be carried out at once - in some cases, diagnostic methods can be expanded or, conversely, used in limited quantities.
The patient is also given a general blood test and stool to examine its composition.
How to treat?
Pseudomembranous colitis, the treatment of which is highly effective, requires long-term and continuous therapy. The most important component of a successful recovery is the abolition of the antibiotic (if a connection is identified between its use and the development of pathology). For mild cases of the disease, this may be sufficient.
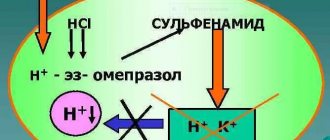
If the disease occurs in a more severe form, the patient is prescribed medications aimed at suppressing the activity of Clostridium difficile (Metronidazole, Vancomycin, etc.). On average, the duration of therapy is from 10 to 14 days. The classic treatment regimen for pseudomembranous colitis looks like this:
- Cancellation of antibacterial drugs.
- Discontinuation of all antiperistaltic drugs.
- Estimate (in standard dose).
- Linux or Hilak-Forte.
- Metronidazole or Vancomycin.
- Elimination of water and electrolyte imbalances (that is, symptomatic treatment selected for each patient separately).
The lack of the desired effect from conservative treatment leads to the need for surgical intervention. Most often this occurs with peritonitis and toxic dilatation of the intestine with an increased risk of perforation. Surgeons prefer subtotal colectomy. Its essence is the complete removal of the affected area of the intestine. The disadvantage of this operation is the high risk of mortality, reaching 58%.
Prevention
Preventive measures include:
- Responsible and competent use of antibiotics. This should be done only as prescribed by a doctor and in accordance with the instructions. It is extremely dangerous to prescribe such drugs to yourself.
- The use of drugs that restore intestinal microflora after antibacterial therapy.
- Strengthening the immune system on an ongoing basis - maintaining a healthy lifestyle, giving up bad habits.
- Maintain personal hygiene. This includes not using other people’s funds or personal belongings.
There is no specific prevention in this case - you just need to take a responsible attitude towards your own health.