Causes of crunching in joints
Causes of “crunching in the bones” - the so-called. crepitus - can be as follows:
- Congenital features of connective tissue. The elasticity of the ligaments and joint capsule is determined genetically. Some people have joint hypermobility - they say that they bend in all directions. If you can, for example, extend your arm at the elbow more than 180°, an anatomical feature may cause clicks in the joint. Another “hereditary” reason is insufficient production of joint lubrication.
- Gas bubbles. The viscous synovial fluid that lubricates the joint can form dioxide bubbles when pressure on the joint surfaces is suddenly released. You suddenly unloaded a limb, and when you took the next step you heard a pop in your knee? Don't worry, it's harmless.
- Tendon movement. When the joint flexes and extends, the tendon also shifts. It sometimes clicks into place when it clicks into place. Most often observed at the age of 10-19 years.
- Teenagers grow too fast. During adolescence, children grow in leaps and bounds, which is why the proportions of their body may be disrupted and their joints may not have time to “adjust.” In the absence of other pathologies, teenage cracking in the joints will go away on its own by the age of 16-24.
- Developmental anomalies. The articular surfaces may not coincide - the edges of the bones protruding from the articular capsule provoke a characteristic sound. Most abnormalities of the musculoskeletal system, which can cause crunching in the joints of the legs, are diagnosed by doctors in the first 7 years of a child’s life. For example, crunching when rotating the foot can cause flat feet.
- Hormonal and metabolic disorders. Age-related hormonal changes (male and female menopause), thyroid diseases and other factors of hormonal imbalance affect the elasticity of the joint. Also, crunching in the joints can be caused by uric acid deposits due to gout, arthropathy due to diabetes mellitus and other metabolic pathologies.
- Taking hormonal drugs. Oral contraceptives and drugs based on glucocorticosteroids can cause joint cracking. It disappears after completing the course or changing the drug.
- Injuries. If crunching and pain in the joints occurs after an injury or strenuous physical activity, you should consult a doctor. Sometimes the joint simply “dries out” due to a lack of synovial fluid, in which case it needs rest and supportive care for 2-3 weeks. And sometimes an already worn-out joint crunches - you need to rush to a rheumatologist to save it.
- Long immobility. For normal production of joint lubrication, the joint must experience moderate physical stress. With a sedentary lifestyle, the joint glides poorly and begins to crunch, and weakness of the ligamentous apparatus is observed. If the cause of joint immobility was an injury, you should consult a rehabilitation doctor who will help restore its functionality without consequences.
- Age-related changes and diseases. Among patients over 60 years of age, inflammatory or degenerative diseases in the joints and adjacent muscles are common. They are less commonly diagnosed in young people.
Excess weight, uncomfortable shoes, and an uncomfortable workplace can also cause crunching and pain in the joints due to improper load distribution.
Associated symptoms
The appearance of a crunching sound in the knee area is not the only sign of the development of pathologies. Most often, in this case, the development of other accompanying symptoms is noted:
- pain syndrome of aching nature or sharp pain;
- hyperemia of the skin in the painful area;
- creaking in the knee area when changing position;
- burning sensations;
- feelings of numbness of the skin in the knee joint;
- the leg becomes completely swollen or swelling is observed in the area of the knee joint.
In some cases, accompanying symptoms are absent or mild. Occasionally, it manifests itself only partially, this is due to the pathology that caused the crunch.
How do you know when it's time to see a doctor?
In itself, crunching in the joints is not a pathology and is even reassuring - with advanced joint diseases it is physiologically impossible.
You need to be concerned about a cracking sound in a joint if it is accompanied by:
- a feeling of friction - as if sand had gotten between the heads of the bones;
- pain that intensifies with movement;
- unusual tension, twitching in the muscles even at rest;
- swelling of the joint and increase in its volume, engorged soft tissues;
- limitation of mobility in the joint;
- a feeling that the joint is “jammed” - possibly a foreign body in the joint capsule;
- redness of the skin over the joint, local increase in temperature;
- a feeling of numbness in the muscles, their weakness, up to impairment of gait or fine motor skills.
Healthy crackling occurs periodically. A simple example: if a gas bubble collapses in a joint, when you move again, there will be no more crunching noise, no matter how much you bend the limb. But the pathological one is heard constantly and only intensifies over time. The specificity of the sound also differs. A loud, dry crunch is quite normal. But if you hear something rough, “with a grinding sound,” check with your doctor for the causes and treatment of crunching in the joints.
Which doctor should I contact for knee pain?
With knee pain, it is best to consult an orthopedic traumatologist or surgeon. In case of chronic knee pain, help can be provided by a rheumatologist. In order to relieve pain, people also consult a physiotherapist, massage therapist or chiropractor.
In which joints is the crunch heard?
Almost all joints can crackle - from the temporomandibular joints to the interphalangeal joints and even the intervertebral joints. For some joints, dry crunching is a physiological norm due to their active load and specific axis of rotation. Therefore, you should not worry about how to get rid of crunching in the joints if “healthy” crackling is heard in the ankles, knees, fingers and spine.
Crunching in the hip joint
Crunching in the hip joint is common among athletes, dancers, and people involved in physical labor. It is often caused by the so-called. snapping hip syndrome - a sound that occurs when tendons roll over bones as the joint flexes and extends.
The hip joint can crunch when there is excess protein in the diet or dehydration. Increasing crunching and pain in the joints may indicate the development of arthritis or arthrosis of the hip joints, or other inflammatory diseases in the muscles and ligaments.
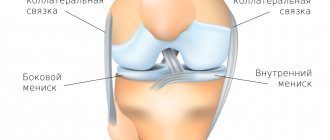
Crunching in the knee joint
Crunching in the knees usually occurs as a result of stress, changes in the periarticular tissues (muscles, ligaments, tendons). Frequent squats, sitting too low or too high, and the habit of tucking your legs can interfere with blood circulation and cause congestion, which is accompanied by a crunch in the knee joint. They are not a pathology, although they can contribute to cartilage degeneration.
Actually, the destruction of the knee joint is accompanied by swelling, discomfort when moving, pain when squatting and other loads.
Crunch in the shoulder joint
Clicking and crunching sounds in the shoulder joint are rarely observed when the joint capsule and soft tissues are healthy. In patients under 35 years of age, they usually occur due to injury—usually while attempting to bench press at the gym. With proper treatment, crunching and other symptoms disappear within 2-4 months. Arthritis of the shoulder joint is more common among people over 60 years of age.
Crunching in fingers
The joints of the fingers are the “crispiest” in the human body. The articular surfaces of the fingers move away from each other more often than others, forming gas bubbles, and ligaments and tendons (there are especially many of them in the hands) more often rub against the protrusions of the bones. How to remove crunching in hand joints? No way. This is an absolutely normal phenomenon - a tribute to developed fine motor skills.
But if your fingers bend worse and become swollen, it’s time to see a doctor.
University
→ Home → University → University in the media → “I’m worried about crunching and clicking in the joints, pain in the knees.” Rheumatologists answered readers' questions
How to minimize seasonal rheumatic attacks? What complications are possible after tonsillitis and how to avoid them? What causes pain and aches in joints? What blood test indicators can indicate joint problems? Is it worth visiting a rheumatologist if someone in your family suffers from rheumatoid arthritis? The online conference “Diagnostics and treatment of rheumatic diseases in children and adults” was held on the information portals “Healthy People” (24health.by) and TUT.BY.
The questions were answered:
Irina Dmitrievna Chizhevskaya, chief freelance pediatric cardiorheumatologist of the Ministry of Health, head of the Department of Pediatrics of BelMAPO, Ph.D.;
Natalya Albertovna Martusevich, chief freelance rheumatologist of the Ministry of Health, associate professor of the Department of Cardiology and Internal Diseases of the Belarusian State Medical University, Ph.D.
— At the age of 15, I was diagnosed with chronic tonsillitis. I am worried about crunching and clicking in the joints, pain in the knees. What examinations and how often do I need to undergo?
Irina Chizhevskaya : Knee pain can occur with flat feet. If it is not corrected at an early age, it can cause joint pain and even cause osteoarthritis. Crunching and clicking in the joints is normal for a growing body, if not accompanied by pain. For chronic tonsillitis, you need to visit an ENT doctor twice a year and determine the ASL-O level at least once a year. If it is elevated, then the doctor will then give recommendations.
— A 6-year-old child is diagnosed with reactive arthritis. Compresses and non-steroidal anti-inflammatory drugs (NSAIDs) do not help. What is the reason and how to treat it? The child is often sick.
Irina Chizhevskaya : To understand what the reason is, you need to be tested for pathogens of enterocolitic and urogenital infections, for example yersiniosis, salmonellosis, chlamydia, mycoplasmosis. If positive results are obtained, antibacterial therapy is necessary taking into account the pathogen. Perhaps the dose and duration of treatment with NSAIDs was insufficient. Typically, NSAIDs are prescribed for 3-4 weeks. If symptoms of the disease persist after this course, it may no longer be reactive arthritis. And you need to see a rheumatologist.
My daughter (7 years old) has juvenile rheumatoid arthritis. The disease began in February 2021. Takes the drug intramuscularly once a week. Since May 2021, she has been in remission (this is according to the documents; in fact, the last exacerbation was in September 2017). The attending doctors say that the injections will continue until adolescence. Although they previously said that the drug would be discontinued after 3-4 years of remission. She is having a hard time with the treatment (her hair is falling out, she vomits on the day of the injection). How do you know when to stop taking the drug? The child is in a state of stress due to the injections and their consequences. Is it possible to switch to tablet form? Isn't this dangerous?
Irina Chizhevskaya : There is no consensus in the world when to stop the drug. The general recommendation for the earliest discontinuation is 2 years of stable remission, confirmed by laboratory and radiographic research methods. We can talk about the state of remission only after 6 months after the last exacerbation of the disease. And then we count down the drug remission. After discontinuation of the drug, an exacerbation of the disease is possible, which can occur at different times. If symptoms of the disease return, all therapy should be returned. It has been proven worldwide that subcutaneous administration of the drug is more effective than tablets. But since the child is in remission of the disease and does not tolerate injections well, you can switch to the tablet form. This is not dangerous.
— A daughter with JRA (juvenile rheumatoid arthritis) from twins, is there a risk of the twin sister or older sister getting the disease? Is it possible to somehow prevent the development of the disease? Can healthy sisters get vaccinated?
Irina Chizhevskaya : There is a risk, since JRA has a genetic predisposition. But this does not mean that all family members will have this disease. Among all the children we see with JRA, there are only two familial cases. There is no prevention. Lead a healthy lifestyle and avoid stress. Healthy sisters definitely need to be vaccinated.
My son is 2.5 years old. After an acute respiratory viral infection (there was only a runny nose, no fever), I could not step on my foot in the evening for half an hour, and the next day I could not do so for about 3 hours. No pain was detected upon palpation. This is an isolated case; after the next ARVI, this did not happen again. What could be the reason for this, and what tests need to be done?
Irina Chizhevskaya: It’s difficult to answer unequivocally. But since this was an isolated incident, there is no need to worry. If this happens again, you should consult a rheumatologist.
“Blood biochemistry showed an increase in uric acid”
- I am 36 years old. Blood biochemistry showed an increase in uric acid - 371 (normal 155-357), a year ago it was 365. For the last six months, my right knee has hurt when I squat completely, both knees crunch, my lower back hurts when I walk for a long time. I changed my diet, completely gave up white and red meat, and started drinking more water. A month later I did biochemistry again, uric acid was 247! Is it possible to reduce this indicator with diet and so quickly? Should this kind of nutrition become a way of life? Can the knee be checked using an ultrasound or is an MRI necessary? How often should uric acid levels be monitored? (all other indicators are normal, antistreptolysin - 131, creatinine - 65).
Natalya Martusevich : The diet could reduce the level of uric acid, since it is the end product of protein metabolism. And reducing meat consumption reduces uric acid levels. The level of 371 is not significant from the point of view of assessing the level of uric acid, since even with very serious disorders of purine metabolism, the target level during treatment is the level of 360. 371 - can be regarded as a slight excess only if the analysis is carried out correctly (within three days the patient does not should take meat foods or a lot of protein foods).
Without knowing the concomitant diseases and without seeing the type of constitution, it is impossible to answer the question of whether it is necessary to continue to adhere to this way of eating. For people with a thin build, eating meat, on the contrary, can be a way to improve their well-being. An MRI of the knee is ideal because it will give you information about the condition of the subchondral bone and structural changes in the joints.
On the right is Natalya Martusevich
I am 50 years old. The disease is ankylosing spondylitis, third group of disability. Six years ago I underwent treatment with Remicade. There was a remission for 2 years. After a new exacerbation, the hospital prescribed Humira. After the second injection, an allergic reaction occurred. Humira was discontinued and Enbrel was recommended. We have been purchasing Enbrel in Moscow for about 2 years now with our own money. Helps great. Is it possible to get Enbrel for treatment at the expense of the budget and where to go for it?
Natalya Martusevich: Enbrel or any genetically engineered immunobiological drug can be prescribed to a patient at the expense of the state budget in a situation where he has exhausted all possible methods of treating this disease with standard drugs used for this disease, which have shown ineffectiveness/intolerance. In this case, the patient continues to have high disease activity or has developed life-threatening complications (amyloidosis). The decision is made by a special commission of the Ministry of Health, which is appointed by order of the ministry. The patient is sent to this commission on the recommendation of the chief rheumatologist of the region (Minsk).
I have adult-onset Still's disease. I take Methylprednisolone. The work often involves night shifts. I noticed that I feel worst in the evenings. If you take, in addition to the morning dose (4 mg), a small dose of methylprednisolone (1-2 mg) in the evening, then the next day I feel much better. However, everywhere they write that it is recommended to take Prednisolone only in the morning. Is it possible in my case to take a small dosage at night, at least during night shifts, or should I avoid taking it in the evening and take the entire dose in the morning?
Natalia Martusevich: Despite the fact that the classic dose is as early as possible in the morning, taking a small dose of methylprednisolone at night is possible. At night, you are awake and your biorhythms are shifted, releasing your hormones. Night work is not recommended for patients with Still's disease.
- I am 45 years old. Diagnosis: rheumatoid arthritis. What modern medicine can replace Methotrexate? It doesn’t suit me: the gastrointestinal tract is already weak.
Natalya Martusevich: You can replace it with Sulfasalazine or Leflunamite. The choice of drug is determined by the doctor and depends on the activity of the disease, concomitant pathology, seropositivity/seronegativity of the disease. Before changing methotrexate, it is usually recommended to take it subcutaneously, which has minimal complications in the gastrointestinal tract.
— Should you trust the drug Instaflex (advertised on the Internet) for the treatment of arthritis/arthrosis?
Natalya Martusevich: It’s not worth it, because the information on the Internet about this medicine is fake. If this information is discovered, the Ministry of Antimonopoly Regulation closes the site. Despite this, advertising appears again from time to time.
- I am 53 years old. I have been suffering from chronic glomerulonephritis since 2002. Over the past year, severe pain in the ankle joints and elbows has become more frequent, I regularly take blood tests, they are within normal limits. At the Central District Hospital they diagnosed arthritis of the ankle joints, prescribed melaxipol and electrophoresis, during the procedures the pain subsided, then after a while the pain returned. The central district hospital doesn’t have its own rheumatologist; I live in a small village. What do you advise?
Natalya Martusevich: I would advise you to see a rheumatologist at the regional rheumatology center, since rheumatological care is provided at the regional and republican level.
“After the fracture, all joints began to hurt”
- I am 35 years old. At the age of 30, I broke my leg in several places and had surgeries. As a result, all joints began to hurt very much - from the fingers to the ankle. They ache and twist at any time of year and weather. What doctors and what tests are needed to solve the problem?
Natalya Martusevich: If the fractures occurred as a result of a fall from the height of one’s own body, then it is advisable to perform densitometry of the axial skeleton to clarify bone mineral density. The results of the study will show the feasibility of further examination. In the case of normal bone mineral density, the emphasis should be on a non-drug treatment method (physical therapy, massage, if there are no contraindications, swimming, sanatorium treatment, physiotherapy). Because the pain syndrome is based on a change in the load on the underlying bones, muscles and ligaments.
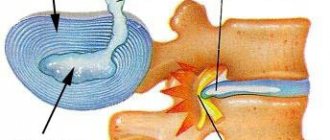
— Are joint diseases and hereditary hemochromatosis C282Y related? How to support joints, what methods and possibilities of prevention?
Natalya Martusevich: Connected. In patients with hemochromatosis, secondary osteoarthritis develops much earlier (earlier wear of articular cartilage and intervertebral discs). This requires correction of the underlying disease, long-term use of symptomatic slow-acting drugs (chondroitin sulfate, glucosamine sulfate or chloride as monotherapy or in combination with each other. Non-drug methods: exercise therapy, spa treatment, physiotherapy, mainly thermal in the absence of contraindications.
I am 49 years old. A year ago, I started having problems with my knee: it hurts to walk, it’s difficult to bend my leg, if you put your palm on it, you feel that the sore knee is hotter than the healthy one. The scan at the clinic did not show any pathology. The therapist prescribed NSAIDs and told me to take them for life. What additional tests would you recommend and where should I go for additional testing?
Natalya Martusevich: To determine the cause of a problem in the knee joint, the following is needed: a general blood test, a biochemical blood test with mandatory determination of the level of C-reactive protein, a general urine test, an examination by a gynecologist, and an ultrasound of the knee joint. If there are no structural changes in the joint, perform an MRI of the knee joint. Examinations can be performed by a therapist in a clinic; MRI is performed if indicated, usually in a hospital setting.
“Knee pain bothers me in spring and autumn”
— All my muscles hurt, I constantly take painkillers, constantly go to doctors, undergo tests and everything else doesn’t help. Tell me what to do, where to go, tell me possible causes or a presumptive diagnosis. Natalia Alexandrovna, born in 1954
Natalya Martusevich : The causes of muscle pain are varied. They can be caused by problems in the muscles, nervous system, or be the result of side effects of drugs, most often statins (drugs to lower cholesterol). To determine the cause, you need to consult a therapist and carry out the following examinations: determine the level of C-reactive protein, creatine phosphokinase, the level of vitamin D, thyroid-stimulating hormone of the pituitary gland, and a general urine test for inflammatory changes. You should also look into the side effects of the medications you are taking. If there are no changes in the tests, the general practitioner will refer you to a neurologist to rule out a neuropathic cause of the pain syndrome.
— Knee pain bothers me in spring and autumn. Should you visit a rheumatologist? If yes, what examinations do you need to come with? Victoria, 35 years old
Natalya Martusevich: Consultation with a rheumatologist is necessary, since some diseases can begin with joint pain without swelling. It is necessary to perform a general blood test, a biochemical study, C-reactive protein levels, a general urinalysis and an examination by a gynecologist. Before examining a gynecologist, you need to undergo an immunological study and determine ASL-O, antibodies to cyclic citrullinated peptide, RF (rheumatoid factor).
Photo: Healthy People portal
Share
How to treat cracking joints
The choice of treatment begins with a diagnosis by a rheumatologist. To do this, you need to undergo an initial examination, functional tests, and possibly x-ray and laboratory tests. If crunching in the joints appears after an injury, it is better to consult a traumatologist.
The first step to treating cracking joints is making a diagnosis.
Treatment for cracking joints is aimed at:
- stopping the inflammatory process in the joint or soft tissues,
- elimination of primary diseases or other causes that caused a problem with the joint (damage to ligaments, cartilage, menisci, labrum, etc.),
- maintaining the elasticity of cartilage,
- prevention of further joint destruction.
Preparations for cracking joints
If the patient is concerned about pain and symptoms of inflammation, non-steroidal anti-inflammatory drugs for cracking joints - such as diclofenac, meloxicam, nimesulide, ibuprofen, naproxen, indomethacin, ketoprofen - become the standard choice. In severe cases, steroids (glucocorticoids) are used - prednisolone, methotrexate and others. The dosage and procedure for using hormonal tablets for cracking joints should be determined by a doctor!
Preparations for cracking joints based on chondroitin and glucosamine (the main structural components of cartilage) are recommended in all cases without exception - as prevention and maintenance therapy of degenerative processes. These include chondroprotectors artracam, artradol, dona, structum (they are available in the form of tablets for cracking joints, which need to be taken for 3-6 months).
If drug treatment for cracking joints is ineffective, the question of partial or complete joint replacement may arise.
Physiotherapy
Physiotherapy is used both in the acute phase of the disease and during remission. It allows you to relieve inflammation, deliver medications to tissues, reduce pain and improve mobility in the joints. Physiotherapeutic methods for treating crunching joints improve blood supply to the muscles and connective tissue around the joint (which means the cartilage receives more nutrients) and restore healthy metabolism. Particularly effective for cracking joints has been demonstrated by:
- kinesiotherapy;
- physiotherapy;
- massage;
- magnetic wave therapy;
- medicinal electrophoresis;
- UHF;
- amplipulse
Other treatments
To treat cracking joints, it is important to include a special diet that helps balance the water-salt balance, nourish cartilage tissue and reduce body weight if you are overweight. The specifics of the diet depend on the causes of the crunch: for diabetes, the consumption of carbohydrates is minimized, for gout - meat.
You should not ignore a rehabilitation doctor - he will help you choose the optimal level and type of physical activity (therapeutic exercises, walking, swimming, cycling, modeling), comfortable orthoses and other ergonomic devices.
Diagnostics
To make an accurate diagnosis, the doctor first interviews the patient to find out some important details:
- were there any other signs that preceded the appearance of crunching in the knees?
- whether the person has a genetic predisposition;
- whether the patient is sick with something else.
When the visual examination and questioning of the patient is completed, the doctor may recommend certain diagnostic procedures:
- magnetic resonance therapy (MRI);
- arthroscopic examination of the knee;
- ultrasound diagnostics;
- radiography
Based on the results obtained after the study, the doctor accurately diagnoses the disease. This will allow you to choose the right treatment in each specific case. How effective the prescribed therapy will be is largely determined by the advanced stage of the disease. You should not ignore the symptoms and wait for them to disappear on their own.
Doctors' advice: how to get rid of crunching in joints?
To prevent and treat crunching in the joints, doctors recommend alternating physical activity with rest, not allowing the joint fluid to stagnate. Also get rid of bad habits - alcohol, smoking and excess coffee consumption accelerate the destruction of joints and reduce the effectiveness of treatment for cracking joints.
Physical activity
Avoid both inactivity and heavy loads on the joint. Any sports exercise should begin with a warm-up, which will “warm up” the muscles and prevent starvation of the cartilage. Aggressive sports, running, and strength training with cracking joints are contraindicated, especially if you have been diagnosed with inflammatory, degenerative changes, or joint hypermobility.
If the crunch in the joints is not associated with the individual anatomical characteristics of the patient, doctors recommend walking more (at least 40-60 minutes or 10 thousand steps a day, or 5-8 km) or cycling, swimming (2-3 times a week ), do Nordic walking or yoga. To track your activity, install a pedometer on your phone. Exercise should be done daily and systematically - do not try to catch up in a few hours 2 times a week. This can worsen the condition of the joint, because synovial fluid does not have time to be produced during intense exercise.
For arthritis and arthrosis, it is better to do not standard exercises, but a set of general strengthening exercises that help maintain the tone of muscles and ligaments.
Labor activity
Increased joint mobility, although not a pathology, can cause varicose veins or injuries due to high load on the joints. Taking this feature into account, it is better not to choose standing work. If you still have to stand, shift your weight from foot to foot more often, equip the place with a low bench on which you can place your foot from time to time. To prevent crunching in the joints, try to dilute the work in the same position with 10-15 minute warm-ups (3-4 during the day) - so-called. industrial gymnastics exercises. These include rotation of the head and torso, clenching and unclenching of fists, circular movements of the feet, hands, knees, and the “mill” exercise with the hands.
If necessary, use elastic bandages and restraints while working.
Weight
Regardless of the causes and treatment of cracking in the joints prescribed by the doctor, the patient needs to lose excess weight - it disrupts the healthy distribution of load between the joints, which is why the intervertebral discs of the lumbar region, hip, knee, and ankle joints begin to suffer. For example, 1 extra kilogram of weight is felt by the knee cartilage as 5.
Treatment for knee pain
In order for knee pain treatment to be effective, an examination is first performed to help determine the cause of the pain. Such an examination may include:
- instrumental studies (radiography, ultrasound, computed tomography, MRI);
- arthroscopy (a diagnostic surgical examination during which an endoscope is inserted into the joint cavity);
- laboratory tests (general and biochemical blood tests, serological tests, joint fluid analysis, etc.).
Treatment of knee pain caused by injury may require realignment of the bones, application of plaster, orthoses, and, if necessary, removal of bone fragments, surgery.
For inflammatory diseases of the knee, complex treatment is carried out, including the use of various groups of medications, physiotherapy, massage, and physical therapy. PRP therapy (injections of platelet-rich plasma from the patient's own blood) may be performed.
Knee surgery
If we are talking about a torn meniscus or ACL, then surgery is impossible. Today, few people resort to open surgery; the most effective and safe method of treatment is arthroscopy of the knee joint. It allows minimal damage to surrounding tissues, and also makes it possible to accurately diagnose the problem and immediately carry out treatment. Using a trocar, two or three holes are made in the knee (as necessary), surgical instruments are inserted through one, and the intra-articular cavity is washed. A long tube with a camera at the end - an arthroscope - is inserted into the other hole. The image is displayed in high resolution on the screen, thanks to which the doctor can observe in real time all the manipulations being performed. This allows the operation to be performed with the highest quality and without complications.
One of the added bonuses of arthroscopy is rapid recovery. In most cases, rehabilitation can begin on the third day. There is no need to spend a lot of time in the hospital, and within a few weeks the patient will have access to the usual movements and return to sports. Another plus is the absence of large scars. Since arthroscopic intervention is minimally invasive, only small marks remain on the side of the knee.
Read more about knee arthroscopy
Rehabilitation after knee surgery
After surgery, it is extremely important to carry out rehabilitation, which includes physical therapy and exercises. In particular, the following are used:
- Unstable boss platforms to stabilize the lower body;
- Lunges and exercises on a fitball;
- Eccentric squats, speed-strength movements;
- Rehabilitation using the Neurac system using Redcord equipment;
- Kinesiotherapy at TechnoGym multi-stations, etc.
Knee dislocations
Accounting for about two percent of all injuries, professional athletes, as well as those who lead a sedentary lifestyle, are at risk. Dislocations occur as a result of a blow or sudden movement.
It is customary to distinguish between primary and secondary injuries. After the primary, it is extremely important to properly carry out treatment and recovery. It is old, untreated injuries that ultimately lead to secondary trauma, as well as the development of other pathologies.
Causes of gonarthrosis
Healthy articular cartilage in the knee serves a buffering and protective function, acting as a shock absorber during movement and impact. Its presence ensures that the bones of the thigh and lower leg do not directly rub against each other.
It is normal for cartilage to break down due to wear and tear due to the natural aging process. However, under certain circumstances, this wear and tear on the cartilage can become excessive. Increased wear and tear on the cartilage, for example, can be caused by excessive stress on the knees caused by heavy physical work, participation in sports, or being overweight. Improper performance of sports exercises can also have an effect, leading to inadequate (not provided for by the design of the joint) mechanical loads. A separate reason is incorrect positioning of the legs (for example, caused by anatomical pathology), when the knees knock against each other when walking. Gonarthrosis can also develop as a result of joint injuries or bone fractures.
What do experts advise?
We recommend the following as preventive measures for cracking joints.
- Avoid stagnation of joint fluid . It is important to alternate physical activity and rest, and avoid heavy loads.
- It is advisable to give up nicotine, alcohol and coffee - they help speed up the destructive process.
- A low-carbohydrate diet will provide some benefits . Eliminate sweets and starchy foods from your diet.
- 2-2.5 liters of water per day .
- Don't choose a standing job . But if you have to stand all day, shift your weight from one leg to the other more often (you can use a low stool). When working in any position, take regular breaks and stretch your joints.
- Watch your weight . Every extra kilogram on your body feels like 5 kg on your knee.
If you experience an unhealthy crunch in your joints, contact the KIT multidisciplinary medical center. We will diagnose and give the necessary recommendations!
Treatment methods for gonarthrosis
Damage to cartilage is irreversible. This means that gonarthrosis, unfortunately, cannot be cured, so treatment is aimed primarily at relieving pain and slowing the progression of the disease.
Conservative treatment
Conservative treatment may include medications, physical therapy, a weight loss program, habit changes to reduce stress on the knees, and the use of orthotics. Anti-inflammatory and painkillers are used to prevent inflammation and reduce pain. The use of elastic orthopedic bandages can reduce pressure on the joint, and special exercises and physical therapy methods can improve its mobility and strengthen the muscles.
Surgery
Surgical intervention becomes necessary if conservative treatment does not give the desired result. There are procedures to create secondary cartilage tissue in the knee. This can reduce discomfort and, in some cases, eliminate pain altogether. However, the load-bearing capacity of the new cartilage is not as great as the old one. In difficult cases, knee replacement is recommended.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Conservative treatment of injuries
If we are talking about a minor injury, they resort to conservative treatment methods. First of all, this:
- Therapeutic gymnastics , performing various types of exercises under the guidance of a specialist for the allotted time (as a rule, this is a whole course of exercise therapy - there is no effect from one lesson);
- Physiotherapeutic measures - magnetic therapy, ultrasound, kinesio taping, exercises on special simulators;
- Taking medications.
The doctor will determine which medications will be prescribed and which physiotherapeutic procedures will be used – he will prescribe treatment depending on the severity of the injury and the characteristics of the individual patient’s body.