Causes of aortic stenosis
The cause of the development of aortic stenosis may be the following diseases: 1. Rheumatism, 2. Protracted septic endocarditis, 3. Atherosclerosis, 4. Infectious diseases. 5. Congenital pathology In addition to true organic stenosis of the aortic mouth, relative stenosis is distinguished, when the aortic valves are not changed, and the ascending part of the aorta is sharply expanded due to arterial hypertension or as a result of loss of elasticity of the aortic wall (atherosclerosis). Aortic stenosis creates a significant obstacle to the flow of blood from the left ventricle into the systemic circulation only if the area of the aortic opening is reduced by more than 50%. Maintaining even 10-20% of its normal value is compatible with life. The lengthening of the systole (contraction time) of the left ventricle and the increase in pressure in its cavity, as a compensatory reaction to the narrowing of the aortic mouth, causes the development of pronounced hypertrophy (increase in muscle mass) of the left ventricle. With no other defect does such significant hypertrophy of the left ventricular myocardium develop as with stenosis of the aortic mouth. Since the powerful left ventricle takes part in the compensation of aortic stenosis, the defect occurs for a long time without circulatory disorders. A long period of compensation is a feature of this defect.
Classification
Classification of stenosis according to the level of narrowing of the aortic mouth:
- valve;
- subvalvular;
- supravalvular.
The most common is valve stenosis (altered fibrotic valves are soldered together, flattened and deformed).
Narrowing of the outflow tract can be observed at different levels:
- damage to the aortic valve itself;
- subvalvular stenosis;
- congenital deformity of the bicuspid aortic valve;
- supravalvular stenosis;
- muscular or fibrous subaortic stenosis.
According to severity they are distinguished:
- I degree. Moderate stenosis – full compensation. Signs of the disease are revealed only during a physical examination.
- II degree. Severe stenosis - the patient presents nonspecific complaints of fatigue, poor exercise tolerance, and syncope. Latent heart failure is noted, and the diagnosis is verified according to data obtained from ECG and EchoCG;
- III degree. Severe stenosis - the clinical picture is similar to angina , signs of blood flow decompensation are recorded. Relative coronary insufficiency is noted;
- IV degree. Critical stenosis - congestion is recorded in the pulmonary and systemic circulation, orthopnea . There is pronounced decompensation.
Symptoms of aortic stenosis
Aortic stenosis is more common in men, especially older men, as a result, for example, of calcium deposits on the valve leaflets. In young people, the most likely cause is congenital anomalies. Complaints in patients with aortic stenosis are determined by the cause of the defect, the nature and course of the disease that caused the defect, the severity and stage of development of the defect. At the stage of compensation of the defect, patients do not complain. The defect is most often discovered accidentally. In patients with more severe stenosis of the aortic mouth, during physical activity (less often at rest), there may be dizziness, a feeling of lightheadedness, fainting, increased fatigue, and compressive pain in the heart and behind the sternum. The combination of squeezing pain in the heart with dizziness and fainting is especially characteristic. The appearance of attacks of cardiac asthma and shortness of breath at rest indicates a significant decrease in the contractility of the left ventricle. Pallor of the skin is observed. Stagnation occurs in the pulmonary and then systemic circulation, which causes the appearance of acrocyanosis and edema.
Diagnosis of coronary artery stenosis
To determine the extent of damage, the doctor sends the patient for a diagnostic examination:
- blood chemistry;
- blood test for cholesterol and glucose levels;
- load tests (treadmill test, bicycle ergometry);
- stress echocardiography;
- electrocardiography;
- 24-hour Holter monitoring;
- ultrasound examination of the heart and blood vessels;
- coronary angiography;
- computer or magnetic resonance imaging of the chest area.
Treatment of aortic stenosis
— All patients, incl. and with minor aortic stenosis that does not have clinical symptoms are under close medical supervision - Patients with aortic stenosis without severe symptoms are recommended to be examined every 3-6 months - Echocardiography - every 6-12 months - All patients with aortic valve stenosis require prophylaxis endocarditis (antibiotics) before, for example, dental treatment or other invasive procedures (regardless of age, cause or degree of stenosis)
Forecast
Aortic stenosis is characterized by long-term asymptomatic treatment, however, after the first clinical signs of decompensation of the disease appear, in the absence of proper treatment, patients die within several years (in half of the patients, death occurs within the first two years).
After aortic valve replacement, the ten-year survival rate is 60-65%. The average lifespan of an artificial valve is 10-15 years. All patients after invasive interventions are monitored by a cardiologist for life. Before any surgical intervention, such patients are given prophylactic antibiotic therapy to avoid endocarditis.
Drug therapy
— There is no specific drug treatment. Drug treatment is aimed at stabilizing hemodynamics - Prevention of infective endocarditis is indicated. Indications for surgery: - pressure gradient between the left ventricle and the aorta is more than 50 mm Hg. Art., or the area of the aortic opening is less than 0.7 cm2 (normally its area in adults is 2.5-3.5 cm2) - angina pectoris, fainting, signs of heart failure. Surgical treatment: — Radical treatment — aortic valve transplantation. — Balloon valvuloplasty of the aortic valve is indicated for elderly, debilitated patients who may not undergo valve replacement surgery
Publications in the media
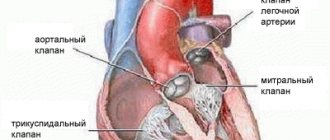
Aortic valve stenosis is a heart defect in the form of narrowing of the aortic opening due to pathology of the aortic valve and perivalvular structures.
Frequency • Isolated aortic valve stenosis - 1.5–2% of acquired valve defects; Aortic valve stenosis in combination with other defects - 23% • Congenital aortic stenosis - 3–5.5% of all congenital heart defects; in combination with other congenital disorders - 13% • The predominant gender is male.
Genetic aspects. Elastin gene defects (130160) in Williams syndrome (see Miscellaneous syndromes) and Eisenberg syndrome (*185500, supravalvular stenosis of the aorta, pulmonary arteries, peripheral arteries).
Etiology • Congenital anomalies, including cusp number anomalies and congenital isolated aortic valve calcification syndrome (61.3%) • Rheumatism (12.6%) • Atherosclerosis (24.2%) • Adult idiopathic calcification (1.9%).
Pathophysiology • Increased afterload ® increased left ventricular (LV) wall tension ® concentric LV hypertrophy ® decreased muscle fiber tension [according to Laplace's law: wall tension = (pressure´ radius)/(2 ´ wall thickness)] • This mechanism maintains systolic function, despite an increase in systolic pressure in the left ventricle • Further myogenic dilatation leads to decompensation and rapid progression of circulatory failure • A sharp decrease in cardiac output leads to insufficient blood supply to the brain, which is manifested by transient or permanent ischemia • If aortic valve insufficiency is associated with aortic valve stenosis, to the increased afterload, an increase in preload is added, which leads to an even greater increase in LV wall tension and a decrease in effective ejection • As a result of the discrepancy between perfusion pressure in the coronary bed and, accordingly, the volume of coronary blood flow to the needs of the hypertrophied myocardium, relative coronary insufficiency develops • With aortic atherosclerosis, the frequency of concomitant IHD, which makes diagnosis difficult • All of these factors lead to a high risk of sudden death • Late manifestations of the defect - hypertension in the pulmonary circulation.
Classification . Depending on the severity (determined by the systolic pressure gradient [SPG] between the LV and the aorta and the area of the valve orifice), four degrees of stenosis are distinguished: degree I - moderate stenosis, GSD <50 mm Hg, valve orifice area >1 cm2 ( norm 2.5–3.5 cm2); II degree - severe stenosis, GSD 50–80 mm Hg, valve opening area 1–0.7 cm2; III degree - severe stenosis, GSD >80 mm Hg; IV degree - critical stenosis, GSD above 80 mm Hg, valve opening area 0.7–0.5 cm2.
Clinical picture and diagnosis
• Complaints: pain in the heart (angina), fainting and shortness of breath are classic symptoms of aortic stenosis.
• Peripheral symptoms are caused by small output syndrome •• Pallor of the skin •• Tachycardia •• Low slow pulse •• “Heart hump” (with the development of the defect in childhood).
• Valvular symptoms •• Systolic trembling in the sternum, in the jugular and supraclavicular fossae •• Weakening of the aortic component of the II tone with severe calcification and decreased mobility of the valves •• With preserved mobility of the valves - increased II tone or click •• With relative mobility of the valves following I tone is used to listen to the systolic ejection sound, which occurs when the movement of the valves stops •• A rough, loud, high-frequency fusiform ejection noise, very well carried to the shoulders, shoulder blades, back of the head and, especially, to the great vessels (the volume of the noise is sometimes so high that it is even carried out on the chair on which the patient is sitting) •• The duration of the noise reflects the severity of the obstruction to a greater extent than its intensity •• Sirotinin-Kukoverov symptom - increased noise when raising the arms up •• With severe calcification of the valves, high-frequency components of the noise can be carried out in the axillary region or to the apex of the heart in the form of a soft mid-systolic murmur, simulating the murmur of mitral regurgitation - Galawarden's symptom.
• Left ventricular symptoms are caused by hypertrophy, dilatation and insufficiency of the pumping and contractile functions of the LV •• Long-lasting, but not diffuse apical impulse, shifted to the left, and a palpable IV tone are almost always present •• An increase in the area of relative dullness of the heart to the left •• Auscultatory signs of congestion in the lungs - diffuse moist rales of various sizes, best heard in the basal regions.
• Symptoms of the underlying disease: rheumatism, atherosclerosis, congenital heart disease.
Special studies
• ECG: signs of hypertrophy and overload of the left sections, primarily the LV; signs of myocardial ischemia.
• Sphygmography: a prolonged low pulse waveform with a difficult-to-define dicrotic notch and jagged apex—a symptom of a “cockscomb.”
• X-ray of the chest organs •• Cardiomegaly (cardiothoracic index exceeds 50%) due to expansion of the LV arch •• Signs of pulmonary congestion •• Expansion of the aortic arch due to its poststenotic dilatation •• Calcification of the leaflets and fibrous ring of the aortic valve.
• EchoCG •• Expansion of the cavity and hypertrophy of the LV myocardium •• Violation of local and global systolic, as well as diastolic functions of the LV •• Poststenotic expansion of the ascending aorta •• Damage to the cusps and apparatus of the aortic valve (defects, vegetations, abnormalities in the number of cusps, increased echogenicity and acoustic shadow with calcification, decrease in the amplitude of movement of the valves) •• In Doppler mode, high-speed flow is recorded through the narrowed opening of the aortic valve and the peak systolic and average pressure gradients between the LV and the aorta are determined •• The area of the aortic valve opening is measured in Doppler and B-modes (as a basis For diagnosis, the worst indicator is taken).
• Catheterization of the left and right ventricles and aorta: direct pressure measurement; see also Aortic valve insufficiency.
• Left ventriculography, ascending aortography •• The presence and degree of stenosis is determined by the diameter of the jet of contrast agent expelled from the LV •• The presence of zones of hypo- and akinesia of the LV indicates myocardial ischemia •• Combined valvular lesions are also diagnosed.
• Coronary angiography: see Aortic valve insufficiency.
TREATMENT
• Drug therapy •• The possibilities of conservative treatment are limited, since it has little effect on the functional class and mortality •• Regardless of the severity of aortic stenosis, infective endocarditis is prevented (see Infectious endocarditis) •• LV systolic dysfunction with congestive heart failure - cardiac glycosides, diuretics , treatment of atrial fibrillation, dual-chamber pacemaker, vasodilators - in small doses and under monitor control (can increase GDM) •• For refractory heart failure - IV inotropes •• Intra-aortic balloon counterpulsation is used as a backup method of hemodynamic stabilization in preparation for surgery •• Termination of pregnancy is indicated.
• Surgical treatment •• Indications ••• Aortic valve stenosis grade III–IV, accompanied by clinical symptoms ••• Asymptomatic aortic stenosis with LV dysfunction ••• There is no consensus on whether surgical treatment is indicated for severe asymptomatic aortic stenosis with normal function LV •• Contraindications: see Aortic valve insufficiency •• Methods of surgical treatment ••• Balloon valvuloplasty - radical treatment for a congenital unicuspid or bicuspid aortic valve, preparation for replacement in case of cardiogenic shock, patient refusal or impossibility of replacement in the near future (for example, with pregnancy, in elderly and debilitated patients) ••• Aortic valve replacement with a mechanical artificial heart valve under conditions of artificial circulation ••• Biological prostheses are not used.
Specific postoperative complications • Restenosis • Angina pectoris • Hemolytic anemia • Secondary infective endocarditis of the prosthesis • Thromboembolism • Aneurysms of the ascending aorta when using disc prostheses with a small opening angle.
Course and prognosis • In the natural course, the 5-year survival rate does not exceed 25%, and the 10-year survival rate does not exceed 10% • The average life expectancy after the onset of angina attacks is 3.5 years, after the onset of syncope episodes - 2 years, after the onset of LV failure - 1.5 years, after the onset of generalized heart failure - 7 months • Sudden death is recorded in 15–20% of patients with clinical manifestations • With GDM above 50 mm Hg. 17% of patients survived 3 years • With surgical treatment, hospital mortality is 3–8%, 9-year survival exceeds 85% with initially preserved function and 10–25% with LV dysfunction • In general, the prognosis after aortic valve replacement with its stenosis is better, than with insufficiency • After valvuloplasty for isolated calcification and rheumatism, despite a decrease in GDM and the area of the aortic valve orifice, in most cases severe aortic valve stenosis persists, postoperative mortality reaches 6%, mortality within a year is 25%, restenosis rate is 60% within 6 months.
Synonym. Aortic stenosis, aortic stenosis.
Abbreviations • GSD - systolic pressure gradient • LV - left ventricle.
ICD-10 • I06 Rheumatic diseases of the aortic valve • I35 Non-rheumatic lesions of the aortic valve