Why do we so carefully study what the thermometer shows us with every cold? What determines the tactics of our further treatment to a greater extent: how we feel or the numbers on the thermometer? And if, due to the characteristics of the body, the temperature during an infectious disease rises slightly, as happens in older people, how can one determine how serious the situation is?
For us, an increase in body temperature is always an alarm signal, because it is quite often one of the symptoms of any disease. We understand that a decrease in temperature after taking antipyretics will not be an indicator of recovery. The correct approach to your health requires first identifying the possible cause of hyperthermia.
Reasons for rising temperature
An increase in body temperature in response to any pathological effect is a nonspecific reaction of the body that is needed to trigger and strengthen defense mechanisms. Under normal conditions, our body maintains a relative constant temperature (temperature homeostasis). The body is protected from overheating by increasing heat transfer processes: intense sweating, expansion of subcutaneous capillaries. The restructuring of thermoregulation processes with reset to a higher temperature level is fundamentally different from the body’s normal reaction to overheating and is called “fever.”
Content:
- Reasons for rising temperature
- Degrees of temperature rise
- What are the dangers of excessive temperature rise?
- Which temperature should be reduced and which should not?
- Increased temperature in newborns
- Temperature for COVID-19
- When to see a doctor
- conclusions
The thermoregulation center is located in the hypothalamus, and sometimes hyperthermia can develop when it is directly damaged (traumatic brain injury, brain tumors), but these are quite rare situations. In the vast majority of cases, the resetting of the thermoregulation center to a higher point is caused by the invasion of the body by bacteria, viruses or other harmful substances. External and internal “stimulants” of the thermoregulation center are called “pyrogens”. External (exogenous) pyrogens are certain substances that enter the body from the environment. Most often they are of an infectious nature: toxins and metabolic products of microorganisms. Internal (endogenous) pyrogens are formed in the body during inflammatory processes, allergic reactions, and the breakdown of tumor tissues. Thus, the range of diseases accompanied by increased body temperature is quite wide [1].
Among the variety of pathologies, it is important to distinguish two main groups: infectious and non-infectious. The combination of the clinical picture of the disease with laboratory parameters allows differentiation between “infectious” and “non-infectious” fever.
An increase in temperature caused by an infectious process occurs in acute and chronic diseases caused by bacteria, viruses and fungi.
Non-infectious causes:
- after blood transfusions (blood transfusions);
- after administration of vaccines, serums;
- if there are foci of aseptic (non-infectious) inflammation in the body (for example, with pancreatitis, gout, thrombophlebitis and other diseases);
- for allergic and autoimmune diseases;
- with the development of malignant tumors (including the hematopoietic system - leukemia), body hyperthermia is included in the concept of the so-called paraneoplastic reaction of the body;
- in the presence of extensive hematomas (hemorrhages) - the increase in temperature in this case is caused by increased destruction of blood cells (hemolysis of red blood cells);
- in the presence of necrotic (dead) tissue (for example, during myocardial infarction);
- if the thermoregulation center in the brain is damaged (for example, after a traumatic brain injury or in the presence of a brain tumor);
- with some endocrine diseases (for example, with hyperthyroidism - a pathology of the thyroid gland, accompanied by its hyperfunction) [2].
Degrees of temperature rise
The degree of increase depends on many factors, including the condition and reactivity of the body and accompanying intoxication.
A slight increase in body temperature in some cases is a normal reaction of the body: during intense physical activity, after eating, during strong emotional stress, in women during the period of ovulation (increase by 0.6-0.8˚C). High ambient temperatures also cause hyperthermia: in hot weather, body temperature is 0.1-0.5˚C higher than in cold weather.
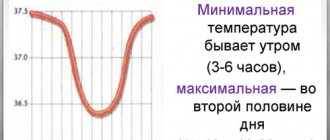
The normal body temperature of an adult fluctuates throughout the day, remaining in the range of 36 – 37˚C (when measured in the armpit). The permissible range of daily fluctuations is usually 0.1-0.6˚C and should not exceed 1˚C. The maximum body temperature is recorded in the evening from 17 to 21 hours, and the minimum in the morning from 3 to 6 hours.
An elevated body temperature from 37 to 38˚C is called subfebrile (from the Latin sub under, below + febris fever). Moderately elevated from 38 to 39˚C is called febrile. High temperatures from 39 to 41˚C are called pyretic (from the Greek pyretos heat). Excessively high body temperature above 41˚C is called hyperpyretic [1].
Formulations with ibuprofen and paracetamol
The good effectiveness of anti-inflammatory drugs allows them to be combined to quickly relieve symptoms of the disease. Tablets that contain both paracetamol and ibuprofen work faster and stronger, but at the same time can cause side effects from both components. The main area of application is the treatment of severe pain. The action lasts about 6 hours.
- Ibuklin
contains 400 mg ibuprofen and 325 mg paracetamol. One tablet can be taken three times a day. Children over 12 years of age are prescribed a maximum of 2 tablets per day. - Nurofen intensive
- tablets with a predominant content of safer paracetamol. The dosage of ibuprofen per unit is 200 mg, paracetamol is 500 mg. Adults can take this Nurofen no more than once every 6 hours, up to three tablets per day, one at a time. If necessary, the dose is increased to the maximum: 2 tablets at a time, 6 in 24 hours.
Combined medications should not be taken for a long time; they are used for quick relief in a serious condition. They are given to older people with caution. Take the combination either before meals, or 2-3 hours after finishing the meal. The course of temperature reduction should not exceed three days.
What are the dangers of excessive temperature rise?
In addition to the detrimental effect on pathogenic microorganisms and stimulation of the immune response, high temperature has a number of negative effects.
Hyperthermia changes metabolism and causes loss of water and salts. When the body overheats, the sweating process increases significantly. Loss of fluid is accompanied by thickening of the blood, increasing the risk of blood clots.
High temperatures pose a great danger to people with cardiovascular disease. When it increases by 1˚C, the pulse increases by 8-10 beats per minute. The heart works at a high frequency, under unfavorable conditions of blood thickening and metabolic disorders. Sometimes, during hyperthermia in patients with cardiac pathology, rhythm disturbances are recorded, which is due to activation of the sympathetic-adrenal system and electrolyte imbalance.
In patients with fever, frequent shallow breathing is observed: the frequency of respiratory movements increases, but the depth of inspiration decreases. Not enough oxygen reaches the organs and tissues, and hypoxia develops.
High temperature accelerates redox processes, which means that the cells' need for oxygen sharply increases: with an increase in temperature by 0.6˚C, the level of basal metabolism increases by approximately 10%. Due to the lack of oxygen, a large number of “acidic” metabolites are formed in the cells, which disrupt the function of tissues and organs. Such a failure of metabolic processes, leading to “acidification” of the body, is called “acidosis.” This is why fever can be accompanied by intoxication. This is most often observed in children, but if the inflammatory process continues for a long time, intoxication also occurs in adults.
When the activity of metabolic processes increases, carbohydrate reserves are used first; after their reserves are exhausted, fats and proteins are used. As a result of increased protein breakdown, their loss is possible up to 300–400 grams per day. Therefore, during fever, it is necessary to give children easily digestible carbohydrates (for example, juices).
With hyperthermia, the function of the gastrointestinal tract is inhibited: appetite decreases, enzyme secretion decreases, motility and absorption processes are impaired. As a result, the development of malabsorption syndrome and constipation is possible. This has a particularly adverse effect on elderly patients.
Patients with high body temperature are at risk of dangerous conditions of the central nervous system, due to increased permeability of the blood-brain barrier and insufficient oxygen supply to the brain. Hyperthermia may be accompanied by agitation. The most dangerous complication occurring in children with an immature thermoregulation system is febrile seizures [3][4][5].
Which temperature should be reduced and which should not?
Increasing temperature is an evolutionary mechanism of protection against pathogenic microorganisms. When exposed to viruses, bacteria and their toxins, immune system cells (leukocytes) produce special substances that trigger an inflammatory response. The temperature reaction is accompanied by a number of characteristic changes in metabolism and physiological functions aimed at strengthening cellular and humoral immunity. In conditions of high temperature, antibodies and defense cells are more actively produced, and the proliferation of viruses and bacteria is inhibited. Many pathogens become sensitive to antibacterial drugs only at elevated temperatures. Its unreasonable decrease suppresses the severity of the immune response. However, very high temperatures pose a danger to the body. Hyperthermia above 40˚C can lead to the development of cerebral edema and dysfunction of vital organs.
The threshold temperature at which it is necessary to make a decision on taking antipyretic drugs is considered to be 38˚C and above. But each person experiences hyperthermia differently. Therefore, you should focus on your well-being and the presence of concomitant diseases. This is especially important in relation to children.
A rise in body temperature above 38˚C is dangerous for children in the first 6 months of life, as well as for children from 6 months. up to 3 years of age who are at risk for developing febrile seizures. In accordance with the recommendations, antipyretic therapy is prescribed for children in the first 3 months of life at a temperature above 38.0˚C, for children older than 3 months (previously healthy) - above 39.0˚C.
In adult patients with severe diseases of the respiratory, cardiovascular and central nervous systems, the course of which may worsen with fever, a decrease in temperature above 38.0˚C is indicated.
For young people without concomitant pathologies, taking antipyretic drugs is indicated at 39.0˚C and above.
The question of choosing a drug is decided in each case individually [6][7].
Tablets with several components
Any complex composition enhances the benefits of the active ingredients, while increasing the likelihood of side effects. Such drugs are more expensive than simple tablets with one active substance, but they help get rid of fever and pain faster. To combat cold symptoms, they are the best.
- Theraflu extratab
- tablets with paracetamol, chlorphenamine maleate and phenylephrine hydrochloride. Reduce runny nose, make breathing easier during colds, relieve irritation of the pharynx and larynx. Take the medicine once every 4-6 hours, you can treat for no longer than 5 days. - Rinza
has a similar composition, but additionally contains caffeine, which reduces drowsiness. Take a tablet 3-4 times a day. - Citramon p
- combines acetylsalicylic acid, paracetamol and caffeine. You can take it every 4 hours. Popular and often recommended by doctors.
Cold tablets replace powder symptomatic remedies, but they begin to act more slowly. Theraflu and Rinza are contraindicated for pregnant and lactating women; The first drug can be given to a child from 12 years of age, the second - only from 15. Citramon contains lower dosages of active ingredients. Pregnant women should not take it in the first and third trimester, and the product is suitable for children from 15 years of age.
Increased temperature in newborns
Separately, it should be said about the increase in temperature in newborns and children in the first year of life.
Immediately after birth, the child’s body is completely ready for independent thermoregulation. Newborns have sufficiently developed sweating and the ability to perform vasomotor reactions. However, an imbalance between heat production and heat loss develops more often in infants than in later life. In the first year of life, due to insufficiently expressed subcutaneous fatty tissue and a relative increase in the specific surface area of the body, the process of heat transfer always predominates. An additional increase in heat generation occurs in newborns due to increased oxidative processes in brown adipose tissue (non-contractile thermogenesis). They do not have contractile thermogenesis (the ability to increase heat production due to involuntary muscle contraction). Within 24 hours after birth, children exhibit the ability to develop fever, but at first it is less pronounced than at an older age. Therefore, infectious diseases in infants may not be accompanied by a significant increase in body temperature, but if this occurs, it indicates the severity of the disease [8].
Ways to reduce fever
The most popular tablets for fever are drugs based on paracetamol or ibuprofen. The first substance causes fewer adverse reactions, is often included in complex preparations and is considered the first choice for fever in children. Both anti-inflammatory drugs are available in several dosage forms, can be included in children's syrups, and are sometimes found together in preparations and enhance each other's effects.
You can alleviate the patient’s condition with tablets containing acetylsalicylic acid, as well as cold preparations: for example, Rinza or Theraflu. In some situations it is better to resort to candles. In case of extreme heat or beginning convulsions, a special remedy comes into play: a lytic mixture of three components. Any medicine for fever should not be taken for too long: it will not affect the underlying cause of the disease, but may cause side effects.
Temperature for COVID-19
The initial manifestations of coronavirus infection are similar to the course of many acute respiratory viral infections. Weakness, headache and muscle pain may come first, followed by catarrhal manifestations: nasal congestion, slight sore throat. Then, as with many acute respiratory viral infections, the temperature rises from 37˚C to 39˚C. This reaction of the body is recorded in most patients with COVID-19. The duration and level of temperature rise during infection with SARS-CoV-2 depends on many factors: the immune response, the amount of the pathogen that has entered the body, and developing complications. Some survive the infection without significant elevation.
The temperature reaction with COVID-19 is a natural response of the body that mobilizes the immune system upon contact with the virus. Therefore, taking antipyretic drugs at temperatures below 38.5˚C is not recommended, except in situations where the patient does not tolerate an increase in temperature.
As a rule, the elevated temperature lasts 1-3 days, sometimes up to 5-6 days. If it is above 37.5˚C for five days in a row, this is a reason to seek medical help, as a more severe course of the disease is possible with the development of complications.
If a young person without concomitant chronic pathology has a high fever, a doctor can be called to his home to assess his condition and prescribe appropriate therapy.
If a temperature above 37.5˚C persists for several days in people over 65 years of age or with serious concomitant diseases, you should definitely call an ambulance for transportation to a hospital.
One of the serious consequences of the new coronavirus infection is hyperinflammatory reactions. This is an excessive immune reaction that is provoked by the SARS-CoV-2 virus.
An indirect sign of the development of a hyperinflammatory reaction may be a return rise in temperature. Febrile fever above 38 degrees after the temperature has normalized is also a reason to call a doctor at home.
A sharp increase in temperature over 38˚C with a significant deterioration in health and the addition of shortness of breath is an indication for calling an ambulance and urgent hospitalization.
A feature of the course of COVID-19 is the prolonged persistence of low-grade fever (not higher than 37 degrees). Subfibrillation can persist for up to a month during the recovery process. In this case, in the absence of other symptoms and satisfactory health, complications are unlikely [9][10][11].
Lytic mixture
Lytic mixture is an effective way to reduce fever in severe cases. It is taken both in tablets and in injections - usually with the help of a doctor. The mixture must include one of the following medications:
- antipyretic: paracetamol, analgin, ibuprofen, nimesulide acetylsalicylic acid;
- antispasmodic to prevent vasospasm: No-spa, Drotaverine, nicotinic acid;
- antihistamine for allergies: Diphenhydramine, Diazolin, Suprastin, Tavegil.
Most often they combine Analgin, No-shpa and Diphenhydramine; the first drug is often replaced with Aspirin. To avoid an overdose, to prepare a lytic mixture, choose medications without the active substances that the patient has already taken. If it is not possible to prepare a mixture for injection, to obtain the effect, it is enough to swallow one tablet of each of the three selected components. You can’t drink lithika for no reason: it should be used only for convulsions, cold extremities due to high temperature or prolonged heat above 39 °C.
When to see a doctor
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Young people without concomitant pathologies should seek medical help if hyperthermia exceeds 39˚C. Patients belonging to risk groups (elderly, with chronic diseases, small children, pregnant women) should call a doctor at home even with a low-grade fever of 37.9˚C and a moderate fever of 38.0-39.0˚C, for a timely appointment therapy.
An ambulance team must be called if severe intoxication develops, signs of respiratory, cardiac, renal or multiple organ failure.
Emergency medical care is required for patients with fever with any signs of damage to the central nervous system (confusion, agitation or retardation, convulsions).
If a fever above 38.5˚C is not relieved by antipyretic drugs in recommended age-specific dosages within 48 hours, it is also worth calling an ambulance so that doctors can provide emergency care and resolve the issue of hospitalization [12].