Body temperature is an indicator of the internal environment of the body. Constancy of temperature is one of the main conditions for normal human life.
The body spends energy on digestion, brain activity, heart beats, muscle contraction and other physiological processes. This energy turns into heat, which is released by the body. The physiological mechanism responsible for body temperature is thermoregulation. Heat balance is controlled by a small region in the brain called the hypothalamus. It monitors the body’s energy expenditure: it can increase or decrease heat transfer.
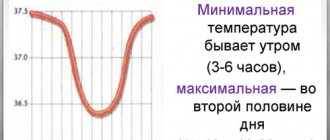
Normal body temperature ranges from 36.5 to 37.5 0C in different parts of the body. During the day, the temperature can fluctuate: at 4–6 am it drops to 35.5–36 0С, in the evening it can rise to 37 0С. This is a daily rhythm, which is caused by different hormonal activity in the evening and morning.
Body temperature is measured in the anus, mouth and armpit. The last option is the most common: when it comes to body temperature, we usually mean measuring the temperature in the armpit. There the average is 36.6 0C.
Stable normal temperature of internal organs and blood maintains the constancy of biochemical reactions, the movement of electrolytes, the viscosity of intracellular fluid and the transport of biological fluids. Temperature also affects the processes of excitation and inhibition in the nervous system, protective reactions of the immune system, the release of hormones and the absorption of nutrients in the digestive tract.
In diseases and pathological conditions, body temperature increases (fever or hyperthermia) or decreases (hypothermia). Based on the dynamics and daily temperature fluctuations, one can suspect the type of infection, the stage of the disease and the degree of its severity.
Reasons for rising temperature
An increase in temperature is an adaptive reaction in response to exposure to pathological factors: bacteria, viruses, parasites, tumors, injuries, poisoning, electric current or endotoxins. An elevated temperature is considered to be an indicator that exceeds 37 0C when measured in the armpit. There are two types of fever - fever and hyperthermia (overheating).
Fever
Fever is a complex process that is activated when the body is exposed to pathogenic factors. Fever involves immune cells and certain hormones.
Fever is characteristic of many infectious diseases and pathological conditions:
- infections: malaria, brucellosis, typhus, tuberculosis, influenza, parainfluenza, measles, rubella, scarlet fever, viral hepatitis, diphtheria, whooping cough, tetanus, polio, cholera, dysentery, salmonellosis, escherichiosis, enterovirus, plague, streptococcus, staphylococcus, cytomegalovirus, parasitic diseases;
- respiratory system: pneumonia, bronchitis, otitis media, sinusitis, laryngitis;
- gastrointestinal tract: appendicitis, gastroenteritis, acute cholecystitis, acute pancreatitis;
- rheumatoid arthritis, reactive and psoriatic arthritis, systemic lupus erythematosus;
- urinary system: pyelonephritis and glomerulonephritis;
- central nervous system: meningitis, encephalitis, meningoencephalitis;
- purulent diseases;
- sepsis;
- malignant tumors;
- recent vaccination.
It is difficult to list all the diseases that cause fever. Almost all of them, which are accompanied by inflammation and cell damage, are manifested by fever. Examples of pathological conditions that can manifest as fever:
- heavy metal intoxication or food poisoning;
- withdrawal syndrome;
- fracture of a limb, dislocation, deep wound, bruise of internal organs;
- electrical injury;
- neuroleptic malignant syndrome;
- teething.
Body temperature can rise even with mental disorders. For example, in febrile schizophrenia, the body temperature exceeds 40 0C.
It is not always possible to determine the cause of fever. For example, there is a pathological condition called fever of unknown origin. It is manifested by one symptom - an increase in body temperature above 380C for more than 3 weeks.
Fever is experienced differently by people. Some people have individual intolerance to high body temperature and experience convulsions. But fever always has common symptoms:
- heart rate increases;
- blood pressure increases;
- sweating increases;
- metabolism accelerates.
Fever is especially difficult for people with cardiovascular, endocrine and neurological diseases. The same applies to older people.
Hyperthermia
Hyperthermia (overheating) is a pathological condition in which the functioning of the thermoregulation center is disrupted and body temperature rises uncontrollably. The endocrine and immune systems do not participate in this process. In this case, anti-inflammatory and antipyretic drugs have no effect. In other words, hyperthermia is a malfunction in the thermoregulation center, and fever is a natural response to a pathogenic factor.
Hyperthermia occurs when compensatory heat exchange mechanisms are strained to the maximum. If you do not create conditions for heat transfer, for example, do not leave the bathhouse or continue to be under the scorching sun, heat stroke occurs.
Causes of hyperthermia:
- thyrotoxicosis – excessive accumulation of thyroid hormones in the blood;
- pheochromocytoma - tumor of the adrenal glands;
- use of muscle relaxants and anesthesia;
- medications: some antidepressants, antipsychotics, drugs against Parkinson's disease, m-anticholinergics.
- long stay in the sun, in a sauna or bath;
- work in a heating microclimate: in a hot workshop or thick clothing.
An increase in body temperature should not always be considered a pathological condition. For example, your temperature may rise during prolonged exercise or while soaking in a hot bath. Body temperature can rise to 37 0C in women during ovulation. This is due to changes in hormonal levels. When menstruation begins, body temperature returns to normal.
Hyperthermia is more difficult for people to deal with than fever. The pathological condition is accompanied by loss of blood electrolytes, convulsions, circulatory disorders, decreased oxygen delivery to the brain, loss of consciousness or psychomotor agitation. In particularly severe cases, hyperthermia leads to death.
How to distinguish hyperthermia from fever
To choose the most effective treatment, you need to know the difference between fever and non-infectious hyperthermia. Main signs of fever:
- body temperature rises when the first symptoms of the disease appear: cough, runny nose, chills;
- increased heart rate and breathing;
- antipyretic drugs are effective;
- symptoms of intoxication are observed: headache, fatigue, increased sensitivity, nausea, loss of appetite.
The main signs of hyperthermia (heat, sunstroke):
- there is a feeling of stuffiness;
- dizziness;
- general weakness;
- strong thirst;
- feeling of squeezing in the heart area;
- aching back pain;
- headache;
- heavy sweating;
- irregular pulse.
Knowing the difference between pathologies means choosing the right treatment tactics and providing first aid as effectively as possible.
Is hyperthermia 39°C dangerous?
Fever itself is not dangerous1,2,3 and is not capable of causing thermal damage to the brain. Moreover, during infections, the internal “thermostat”, even in the absence of treatment, does not allow the thermometer to rise above 41.1°C2.3.
Hyperthermia, as strange as it may sound, is generally beneficial1,2,3.
Thanks to her3:
- the activity of leukocytes, the main fighters against infection, increases;
- the production of interferon, a special immune substance that has an antiviral effect, increases;
- metabolic processes are accelerated, providing damaged tissues with nutrients necessary for recovery processes.
The number “39” on the thermometer indicates a danger for people with concomitant diseases of the heart, lungs and nervous system, as well as individual intolerance to hyperthermia1,2,3. For others it is not scary.
The main “disadvantages” of hyperthermia1:
- tachycardia - an increase in the thermometer by 1°C leads to an increase in heart rate by 10-15 beats per minute, which increases the load on the heart1;
- heart rhythm disturbances (extrasystole);
- fluctuations in blood pressure;
- loss of fluid due to increased sweating and rapid breathing;
- disturbances in intestinal motility and constipation;
- activation of latent herpetic infection1.
In addition, a rapid rise in temperature to 39.5-40 °C within 1-2 hours can lead to the development of hyperthermic syndrome1,4 - a life-threatening condition. It usually occurs in children and is accompanied by pallor, dryness and coldness of the skin and mucous membranes, frequent shallow breathing, weakened cardiac activity, a drop in blood pressure, loss of consciousness and convulsions4. Therefore, if the fever progresses rapidly, immediate action must be taken.
Up to contents
When to lower the temperature
Body temperature should be reduced when it exceeds 38.5 0C in children and adults. However, there are conditions when body temperature needs to be reduced if it has reached 38.0 0C:
- child under 2 months;
- presence of cardiovascular pathology;
- oncological diseases;
- epilepsy;
- hypertonic disease.
If the patient previously experienced convulsions or impaired consciousness at a body temperature of 38.5 0C or higher, medications should be taken at 38.0 0C.
How to reduce a high temperature
7 tips on how to bring down a high fever with a cold or flu:
- the key to everything is sleep and rest;
- drink plenty of fluids - from 2 to 2.5 liters per day;
- choose light or blended food;
- take probiotics;
- don't wrap yourself in clothes.
The following recommendations are general and are not intended for a specific child. Only a doctor can give precise instructions with individual selection of treatment. Self-medication can lead to serious consequences. If a child has a high temperature that rises quickly, call your local pediatrician or an ambulance.
The pathogenetic mechanism of fever is closely related to inflammation. Therefore, anti-inflammatory drugs with an antipyretic (antipyretic) effect are used to lower the temperature. It should be remembered: treatment of fever is the elimination of the symptom, and not the treatment of the disease itself.
There are methods to physically lower body temperature, especially in children. These include: cold heating pads, cold enemas and wiping with cold water. However, it should be remembered that such methods do not have an evidence base. These methods are unsafe and are therefore excluded from protocols for the symptomatic treatment of fever.
The World Health Organization recommends two medications to treat fever: ibuprofen and paracetamol. WHO offers these drugs as the most studied, safe and effective. They rarely have side effects and have the least effect on the liver, so ibuprofen and paracetamol are indicated for children and adults.
How to reduce the temperature of an adult (one of the drugs):
- paracetamol – 650–1000 mg every 6 hours;
- ibuprofen – 400–600 mg every 6 hours.
In this case, the maximum daily dose should not exceed 4 g to avoid toxic manifestations. Take the tablets with plenty of warm water, do not dissolve or chew, or dissolve in water. It is best to take the tablets during or after meals. When taking paracetamol and ibuprofen, you should temporarily avoid other medications against influenza or other infections if they contain acetaminophen, aspirin, naproxen, or any other drug from the group of non-steroidal anti-inflammatory drugs.
How to bring down a child’s temperature (one of the drugs):
- paracetamol – a single dose of 10 mg/kg body weight;
- ibuprofen - a single dose of 5-10 mg/kg body weight (for children over 3 months).
The next dose of one of the medications is after 4–5 hours. Taking the drug is considered effective if after 30 minutes the body temperature has dropped by 0.5–1 0C when measured in the armpit. Remember, you should not self-medicate. To accurately assess your child's condition and give him the right medications, you need to consult a doctor.
In children, fever can be malignant - this is called “pale” fever. It is accompanied by centralization of blood circulation, impaired microcirculation, deterioration of the child’s well-being, severe chills, cold feet and hands, and pale skin. In the case of pale fever, paracetamol or ibuprofen is administered intravenously at a dose of 15 mg/kg body weight.
If there is no paracetamol or ibuprofen at home, you need to use “backup” therapy - a 50% analgin solution intramuscularly at a rate of 0.1 ml per 1 year of the child’s life. However, after administration of the medicine, side effects may occur: allergic reactions and changes in blood tests. However, before you administer analgin, call a doctor. He will assess the child’s condition and tell you exactly whether the medicine needs to be administered.
Due to excessive sweating, fever is accompanied by dehydration. Therefore, during a fever, you should drink a lot of mineral water, tea, fruit drinks, decoctions and juices. In addition, a large amount of fluid promotes detoxification - waste products of viruses or bacteria are eliminated from the body faster. With a fever, appetite decreases. However, you still need to eat. In this state, easily digestible carbohydrates are best: baked goods, sweet drinks, jam or cakes.
If overheating occurs due to sun or heatstroke, the patient must be taken away from the heat source and direct sunlight. The patient should be placed on a bed or sofa in a cool and ventilated room. Next, remove outer clothing and ensure adequate heat transfer. Spray a large amount of room temperature water on your face. Now that the person is safe, call an ambulance. Meanwhile, fan your body with a newspaper or towel, or turn on a fan.
Folk remedies
Traditional methods of treatment also cope well with elevated temperatures. There are at least ten effective recipes that you can prepare yourself at home.
Strawberry
It is not only useful, but also a pleasant remedy for fever. In order to bring down the temperature of 39 in an adult, it is advisable to take 50 grams of berries immediately after a meal or eat two tablespoons of jam.
Chamomile infusion
Dry crushed pharmaceutical chamomile is used as raw material. A teaspoon of raw material should be poured with a glass of boiling water.
Leave to infuse for 30 minutes, then judge and strain. Take the resulting product 6-7 tablespoons every half hour.
Remedy made from pureed viburnum
Rub the viburnum berries with sugar and leave to steep in the jar for several days. Take a tablespoon of the resulting raw material and pour it with a glass of hot water.
The product should infuse for 15 minutes, after which it must be strained. Use as tea.
Puree currant remedy
It is prepared in the same way as the previous product. With the only exception that you need to insist on it for 20-25 minutes. Take as tea.
Raspberries
Raspberries, namely raspberry jam, are perhaps the most famous remedy for fever. This is the most affordable method of treatment. It is enough to take 2-3 tablespoons with tea and wrap yourself in a warm blanket to sweat. This will solve the temperature problem.
Vinegar
Regular vinegar can be a great way to beat heat. In a 1:2 combination, a weak solution is mixed with water (to avoid chemical burns, take 1 part vinegar and 2 parts water). Then the resulting product is rubbed onto the patient’s body. This is an effective recipe.
Dried fruits
A decoction of their dried fruits allows you to quickly cope with hyperthermia. To prepare the decoction, you need to take a handful of raw materials, pour half a liter of boiling water over it, and leave for 30 minutes. Take a glass 3 times a day.
Linden blossom
To bring down the temperature, linden blossom tea is suitable. Take a handful of linden flowers. Pour half a liter of boiling water over them. Strain. Add a tablespoon of honey. Leave for 30 minutes, then take a glass three times a day.
Cranberry
It works due to the content of a large amount of salicylic acid. To prepare, take a tablespoon of berries and pour a glass of boiling water over them. Leave for 30 minutes, then strain. Take 3 tablespoons 3 times a day. Can be consumed in larger quantities as tea.
Pearl barley decoction
To prepare, take 100 grams of pearl barley, fill it with water (a liter) and boil for 20 minutes. You can add honey. Take half a glass of the decoction three times a day.
All of these recipes are safe. However, if after taking folk remedies the temperature does not subside, you should definitely call an ambulance.
Fever without symptoms: what to do
Sometimes there may be no symptoms of fever: no cough, headaches, runny nose, fatigue or chills. Fever without symptoms can occur in two cases: fever without a source of infection and fever of unknown origin.
Fever without a source of infection affects children under 3 years of age who do not have catarrhal symptoms (runny nose, cough, sputum) and other signs that indicate the cause of the pathology and its location. Fever without a focus of infection occurs with viral and bacterial diseases, most often with pneumococcal infection, Haemophilus influenzae, typhoid and salmonella. In this case, you need to show the child to a pediatrician or call an ambulance, as it is necessary to quickly establish the cause and begin treatment.
Fever of unknown origin is a syndrome in which fever (38.5 0C and above) does not go away on its own and lasts longer than 3 weeks. However, the cause could not be determined after using routine diagnostic methods. Probable causes: infections (most often tuberculosis), autoimmune diseases, malignant neoplasms, medications, alcoholic cirrhosis, Crohn's disease. If you have a fever of unknown origin, you need to see a doctor and be hospitalized so that doctors can monitor the patient constantly.
Diagnosis of the primary source of pathology
It is not the temperature that needs to be diagnosed, but the initial factor that caused hyperthermia.
Diagnostics begins with choosing a specialized specialist. In this case, an initial consultation with a therapist is recommended.
He will help you decide on examination tactics and give you the necessary directions.
There are a great many specialists who help get rid of fever:
- Nephrologist (for kidney pathologies).
- Neurologist.
- Neurosurgeon (in tandem with a neurologist treats pathologies of the central nervous system that cause a rise in body temperature).
- Infectious disease specialist.
- ENT.
- Rheumatologist.
- Oncologist, etc.
It is extremely difficult to independently understand the huge number of specialists.
Diagnostics includes both a number of instrumental and a number of laboratory studies:
- Ultrasound (thyroid gland, abdominal cavity, genitourinary system).
- Psychiatric research using special tests.
- X-ray (lungs, other organs).
- Visual assessment of organs (for ENT pathologies, etc.).
- Contrast radiography of the genitourinary system.
- Fluorography.
- MRI/CT examinations. Allows you to obtain detailed images of the organs and structures being examined. These methods play a huge role in identifying organic brain lesions.
Laboratory methods are no less informative:
- Complete blood count: gives a picture of inflammation (leukocytosis, high erythrocyte sedimentation rate).
- Biochemistry of blood.
- Bacterial cultures.
In combination, these methods are sufficient to make an accurate diagnosis and prescribe the correct treatment.
Temperature does not go down - when to call an ambulance
After using paracetamol or ibuprofen, body temperature should decrease at a rate of 0.5–1 0 C per hour. However, sometimes the fever remains at the same level, while the patient’s well-being worsens. In what cases should you call an ambulance or go to the hospital yourself if:
- taking medications according to the regimens described above did not produce any effect;
- for “white” fever, analgin had no effect;
- fever is combined with concomitant pathologies: epilepsy, intracranial hypertension, hydrocephalus, congenital heart defects;
- against the background of fever, the patient refuses to drink and eat, has difficulty breathing and cannot sleep;
- fever is accompanied by severe abdominal pain and incessant vomiting.
If the temperature rises, even despite taking medications, most likely this is a pathological variant of fever - hyperthermic syndrome, in which antipyretic drugs are not effective. This is also one of the reasons to call an ambulance and be hospitalized.
5
1
6
Article rating:
5 out of 5 based on 9 ratings
Author: Atamanenko Alena Valerievna
General practitioner, endocrinologist, physiotherapist. Second category. Work experience more than 9 years.