23.09.2019 9898 0
Newborns and children under one year old have immature thermoregulation. The body quickly reacts to any temperature changes, clothing inappropriate for the weather, or food intake. Even prolonged crying can cause a rise in temperature! The baby's body temperature may be 0.5-1 degrees higher after sleep and feeding.
Mercury thermometer
The most accurate device, there is practically no deviation from the temperature measurement, and errors are rare and are calculated in fractions of a degree. Another advantage is the possibility of disinfection. This device can measure the temperature in the armpit, mouth and rectum.
A mercury thermometer has two disadvantages - the duration of measurement and fragility. The thermometer will have to be left in the armpit for 10 minutes, in the mouth and anus for 5 minutes, which causes difficulties when measuring temperature in infants. The thermometer is made of glass, and is filled with the substance mercury, which causes poisoning of the body. Therefore, it is important to be careful when using it, especially in children.
Why do you need to measure temperature?
We all know from childhood that normal temperature is 36.6 * C. But in fact, small fluctuations occur during the day, which are in no way related to diseases and pathologies. For example, in the morning the indicator decreases slightly, but in the evening it may well rise.
Most often, we perceive an increase in temperature as an alarming sign. On the one hand, this is correct, because if the indicator goes beyond the norm, it usually indicates some kind of malfunction in the body. But there is a second side to the issue: the body raises its temperature to protect against the introduction of bacteria or viruses, activating the immune system.
In other words, an increase in temperature is a way to combat foreign and dangerous microorganisms, and not at all a reason for panic. But it is necessary to control the temperature level, for a number of reasons:
- Recognition of diseases at an early stage;
- Monitoring the course of the disease;
- Assessing the effectiveness of prescribed procedures and medications;
- Preventing the negative effects of too high a temperature on the body.
Fever is especially dangerous for children under 3 months of age. For them, the maximum permissible value is 38*C; in other cases, measures will have to be taken to reduce the indicator. If the child has previously had febrile seizures, increasing the temperature to this level is unacceptable. The same applies to children with severe pathologies of the nervous system, lungs or heart.
Who is guilty?
Most often, the cause of fever in children is pathogens that have entered the body. Moreover, in most cases that cause diseases of the upper respiratory tract are to blame Fortunately, they are mostly quite harmless and go away in three to seven days.
If the cause is bacteria , then the temperature in children is usually very high - up to 41 degrees. Such a sharp rise in body temperature is usually caused by purulent inflammation of the middle ear (otitis media), meninges (meningitis) and abscesses. In addition, such indicators can also signal acute inflammation of the kidneys or renal pelvis. As a rule, it is in the case of bacterial diseases that pediatricians prescribe antibiotics to their young patients.
There are cases when the temperature rises after vaccinations . In this case, the cause is weakened pathogens of various diseases contained in vaccines.
Sometimes the temperature may rise as a result of children's increased physical activity . If after a walk or outdoor games your child seems too hot to you, give him a rest for half an hour and measure his temperature again. Most likely, she will be normal.
Special cases
There are situations when in some children an increase in temperature leads to seizures. The child may roll his eyes, convulse, clench his teeth, or even lose consciousness. This reaction can be frightening. However, research shows that in most cases, seizures do not affect the mental development of the child and extremely rarely signal epilepsy. However, if a child has had convulsions, especially prolonged ones, it is necessary to seek medical help, and before that try to bring down the temperature (how to do this is described in detail above). If at least once in his life a baby has had a seizure that occurs when the temperature rises, experts recommend not allowing it to rise above 38 degrees.
Sometimes an increase in temperature, even not very significant, up to 37.5 - 37.8 degrees, can lead to nosebleeds. Usually in such cases, doctors prescribe a course of ascorutin (it contains ascorbic acid and vitamin P) and advise reducing the temperature. In any case, you shouldn’t make diagnoses yourself. If your baby has a nosebleed during illness, especially more than once, be sure to tell the doctor about it.
Features of body temperature
The normal temperature for humans is 36.6 degrees. But this indicator is relative, since it directly depends on age, weather conditions, physical activity and time of day.
In older people, a normal temperature is considered to be below 36.6, since they move less and their metabolic processes in the body are slower. In children, the temperature level approaches 37 degrees, which is also a natural phenomenon, since at an early age the child is more mobile.
During the day, body temperature may deviate slightly from 36.6 degrees. The lowest body temperature in a healthy person can be recorded between 5 and 8 a.m., and the highest in the evening, from 4 to 6 p.m.
A radical deviation in body temperature, both up and down, is critical for human health. An alarming symptom is if it drops to 35 degrees or rises to 38. This indicates the development of the disease. Therefore, it is important to be able to take measurements correctly and with minimal errors, which will allow you to control the situation and provide timely treatment.
If there is a slight deviation from the norm, it is enough to measure the temperature 2–4 times a day, and in the case of an acute form of the disease - every hour.
An indicator below 32 degrees and above 42 is fatal.
Hyperthermia
It happens that the temperature rises not due to illness, but due to external influences. Then we are talking about overheating of the body or hyperthermia. This can happen not only in summer, but also during the cold season. Therefore, if your baby complains of a headache, weakness and dizziness, if he starts vomiting or even loses consciousness, think about whether he could have overheated somewhere and suffered a heatstroke. In this case, cold compresses on the forehead, back of the head, chest and calves are helpful. And, of course, you need to see a doctor.
How to bring down the temperature
As mentioned above, it is not worth bringing down a fever that is not very high, especially if the child tolerates it normally. However, when such a need still exists, try the following methods:
- The temperature is very high, and there is no way to wait for the antipyretic to take effect? Undress the child immediately, remove everything from him, even the diaper. This will quickly lower the temperature by about a degree.
- Rubbing the body also helps. Use warm or cool water for them. This will not only not harm the child, but will significantly alleviate his condition. At the end of the procedure, be sure to dry the baby with a dry soft towel or flannel diaper. This method can be used several times a day.
- Antipyretic compresses are also quite effective. Usually two types are used: calf and chest. In both cases, towels are dipped in warm water (water at room temperature is also suitable for calves) and placed on the child’s legs or chest.
- A diaphoretic wrap reduces the temperature well. Before wrapping the baby, you need to give hot tea with linden. After this, a sheet soaked in warm water and wrung out is placed on a large blanket. This, and then the blanket, is wrapped completely around the child, excluding the head. Carefully monitor the patient's well-being. If he experiences any discomfort, unwrap him immediately. If the baby feels normal, then wrapping can last from 30 to 60 minutes from the start of sweating. Keep in mind that this method is only suitable for strong children over two years old, provided that there are no problems with the cardiovascular system.
- Medicinal antipyretics have proven themselves to be quite effective. However, when deciding to give them to your child, keep in mind that the composition of antipyretic suppositories sometimes includes components that have a hypnotic effect. Therefore, it is better to use such candles only in the evening or before bedtime.
Calf compress:
- Soak towels in water at room temperature.
- Squeeze.
- Wrap around each leg. The fabric should cover the leg from the ankle to the popliteal cavity. Attention! The wrap should not be very tight.
- Wrap with dry woolen scarves or shawls.
- Calf compresses need to be changed every 5 to 15 minutes.
- As a result, the temperature should drop by 1 - 2 degrees.
- If you have a chill, you can’t make compresses! Before the procedure, be sure to make sure that your baby’s feet and hands are warm.
Compress on the chest:
- Soak a towel in warm water.
- Squeeze.
- Wrap the baby's chest.
- Cover the top with a flannel diaper or woolen scarf so that they completely cover the wet towel.
- After 20–30 minutes, the compress must be removed.
- Dry the child with a dry towel.
- You can do this compress several times a day.
- You can’t leave the compress on overnight or let it dry on your body!
Temperature measurement in the ear
A rather exotic method, but in the ear you can catch the earliest temperature changes in the body.
Features : You cannot measure the temperature in the ear with ordinary thermometers. A special infrared ear thermometer is required. If there is an inflammatory process in the auricle, the device will give an inflated result.
Extremely low. At what body temperature can a person die? More details
The normal temperature in the auricle is 35.5-37.5 degrees.
What to feed a child with fever
As a rule, a child with fever does not want to eat. And this is good: experts believe that the body “is not distracted by trifles” in order to devote all its strength to fighting the pathogens of the disease. Therefore, do not stuff your child. If he gets better, he will eat. But if he is still hungry, offer him curdled milk or yogurt, grated apples, bananas, cottage cheese dishes, and light soups. Don't forget to drink plenty of fluids. Chamomile or linden tea, still mineral water, and fruit drinks will be beneficial. It is better if they are warm, but not hot.
Photo - Lori's photo bank
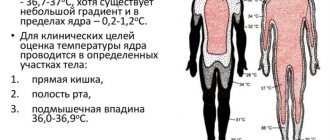
What does “normal” temperature mean? Although a “normal” temperature reading is generally considered to be 36.6˚C, measurement readings can range from 35.2˚C to 36.8˚C and still be considered “normal.” Variations in temperature can be explained by activities such as exercise, physical activity and food and drink consumption. Your temperature is lower in the morning than in the afternoon. Other variations may be related to the method of temperature measurement: axillary (underarm measurement), oral (in the mouth), and rectal (rectal measurement). If the armpit temperature corresponds to the characteristics described above, then the oral temperature is usually 0.5˚C higher. Rectal temperature will be 1.0˚C higher.
Methods for measuring body temperature:
- Axillary measurement: Wipe the armpit with a dry towel and place the tip there. When measuring temperature, keep your hand pressed tightly to your body (the armpit should be closed). The normal armpit temperature range is 35.2-36.8˚C.
- Oral measurement: Place the tip under the tongue as close to the bottom of the tongue (in the sublingual fold) as possible. Keep your mouth closed while taking your temperature. The range of normal oral temperature is 35.7-37.3˚C.
Please note: Drinking hot or cold drinks, smoking, exercise or other activities may raise or lower your temperature. Therefore, it is important to relax for about 5 minutes with your mouth closed before taking the measurement.
- Rectal measurement: Lubricate the tip with water-soluble hygienic lubricant; do not use petroleum jelly. Insert the tip of the thermometer into the rectum about 1 cm. The normal rectal temperature range is 36.2-37.7˚C.
The measurement usually takes 1-3 minutes, but may take longer or significantly less time depending on the method used and the type of thermometer.
NOTE: For hygiene reasons, you should not use the same thermometer for a rectal measurement that you used for an axillary or oral measurement. Avoid drinking hot or cold drinks, exercising, smoking, or taking a bath or shower immediately before taking a measurement. General precautions
- Children should only use the thermometer under adult supervision.
- Do not walk, run or talk while taking your temperature.
- Clean the thermometer before and after each use.
- Store the device in its protective case when not in use.
- Do not chew the tip of the thermometer.
- Do not store the device in a place where it may be exposed to direct sunlight.
- rays, in a dusty or damp place. Avoid sudden temperature changes.
- Be careful not to drop the thermometer or subject it to strong impacts.
- Do not attempt to disassemble the electronic thermometer except to replace the battery.
thermometer
Share this article with your friends
Non-contact measurement methods
You can obtain the necessary data without direct contact with the patient. This became possible with the help of infrared thermometers, which appeared not so long ago. Their principle is based on determining the amount of heat from the person being diagnosed with further conversion of the information into an electrical signal. Infrared thermometers give an error level of 0.1–0.2 degrees.
Non-contact methods of temperature measurement allow you to obtain the necessary data in 1–3 seconds. To do this, it is enough to bring the device to the forehead of even a sleeping person. This procedure reduces the likelihood of transmission of infection through the device, since there is no direct physical contact. Therefore, this method is ideal for public institutions: hospitals, medical facilities. offices, schools, kindergartens.