Anatomy and physiology
The large intestine is separated from the overlying small intestine by a muscular valve, the so-called. ileocecal sphincter or bauhinian valve. The large intestine is located in the lower part or floor of the abdominal cavity and includes the following sections:
- Caecum (lat. – caecum). It is 3-8 cm long and 4-7 cm wide. This section of the large intestine is equipped with a vermiform appendix, the appendix. The cecum with the appendix is projected onto the right middle and lower part of the anterior abdominal wall.
- Colon (lat. – colon). The longest section of the small intestine. The colon, about 4 cm in diameter, borders the entire lower floor of the abdominal cavity with loops of the small intestine and other organs. Hence the name. In the colon, its initial ascending part is distinguished. 12-20 cm long from the cecum to the right bend, the so-called. hepatic angle. The transverse colon is its middle part, 50 cm long, from the hepatic angle to the splenic angle, the left bend. The descending part, 22-23 cm long, runs from the splenic angle to the sigmoid colon. Due to the fact that the transverse part sags slightly, the configuration of the colon resembles the letter M.
- Sigmoid colon (lat. - colon sigmoideum). The same applies to the colon, and in the form of two loops 54-55 cm long and 4 cm in diameter is located between the descending part and the rectum. It is projected onto the anterior abdominal wall in its lower left part.
- Rectum (lat. - rectum). Located in the pelvic cavity. The length of the rectum is 14 cm. The width in the initial sections is 4 cm, then it expands into the ampulla of the rectum 7.5 cm, and ends with a narrow opening of the anus.
Compared to other parts of the gastrointestinal tract , the large intestine has its own characteristics. Unlike the pink small intestine, the large intestine has a grayish color. On the outside it is covered with a serous connective tissue membrane. Parts of the colon, and in some cases the cecum, are fixed to the walls of the abdominal cavity by the mesentery. This mobile anatomical formation is formed by two layers of peritoneum. Vessels and nerves pass through the mesentery to the intestines.
The middle muscular layer is represented by an inner circular or circular layer and an outer longitudinal layer. Peristaltic (wave-like) contractions of these muscles ensure the movement of the food bolus through the intestinal tube.
But, unlike other parts of the gastrointestinal tract, the outer muscle layer here is continuous only at the junction of the cecum with the appendix , and in the rectum. And for the most part it is represented by three ribbons. These tapes seem to tighten the intestinal tube. As a result, protrusions and haustra are formed on its surface. The haustrae are separated from each other by transverse grooves. These grooves correspond to the semilunar folds of the mucous membrane.
There are no villi on the mucous membrane, like in the small intestine. It contains secretory glands that secrete digestive juice. Colonic juice is secreted at rest, but its amount is small.
Food contents enter the large intestine from the small intestine in small portions at the moment the ileocecal sphincter opens. In response to mechanical irritation, juice secretion increases many times over. It contains: amylase, lipase, and a number of other digestive enzymes. But in general, the content of enzymes in the juice of the large intestine is low, 20 times less than in the juice of the large intestine.
The amount of absorbed food components is also small. Here, those food components that are not absorbed in the small intestine are absorbed in small quantities. The main function of the large intestine is to absorb water from the bolus of food and form feces in a daily amount of 150 g or more.
When eating plant foods, more feces are formed than when eating foods of animal origin. Plant foods contain a large amount of indigestible fibers that absorb intestinal toxins. The final section of the gastrointestinal tract, the rectum, serves as a reservoir for feces. The act of defecation is controlled by muscle valves - the internal and external sphincter.
The functioning of the large intestine is largely influenced by the microflora it contains, represented by bifidobacteria, lactobacilli, and bacteroides.
The main functions of physiological intestinal microflora:
- The final breakdown of undigested food components.
- Inactivation of bile components and digestive juices that enter the large intestine from the overlying sections of the gastrointestinal tract.
- Neutralization of toxic products formed during the digestion of food.
- Synthesis of vitamin K and some B
- Destruction of pathogenic intestinal microflora.
- Participation in other nonspecific immune reactions.
Along with microflora, immune protection is provided by accumulations of lymphoid tissue located in the mucous membrane, lymphatic follicles.
Classification of types of digestion
According to the origin of digestive enzymes, they are divided into three types:
- own;
- symbiont;
- autolytic.
According to the localization of the polymer splitting process:
- intracellular digestion;
- extracellular digestion: distant (cavitary);
- contact (wall, membrane).
Symbiont digestion
Symbiont digestion is the hydrolysis of nutrients due to enzymes synthesized by the symbionts of the macroorganism - bacteria and protozoa of the digestive tract. Symbiont digestion occurs in humans in the large intestine.
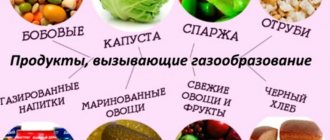
Fiber in food in humans, due to the lack of the corresponding enzyme in the secretions of the glands, is not hydrolyzed (this has a certain physiological meaning - the preservation of dietary fiber, which plays an important role in intestinal digestion), therefore its digestion by the enzymes of symbionts in the large intestine is an important process.
Enzyme products from NSP:
1. Digestive enzymes
- Digestive enzymes replenish the deficiency of digestive enzymes.
- Improves the breakdown and absorption of nutrients.
- Digestive enzymes also normalize the functioning of the digestive organs.
2. Protease Plus
- Used as a systemic enzyme preparation.
- Improves the breakdown and absorption of proteins.
- Reduces blood viscosity, improves blood circulation.
- Has anti-inflammatory and anti-edema effects.
3. Ag-X
- Reduces inflammatory processes in the digestive system, reduces pain.
- Strengthens the secretion of digestive enzymes and bile, improves the digestion of food in the gastrointestinal tract.
- Increases the body's protective properties.
Diseases and symptoms
Diseases of the large intestine:
- Chronic non-infectious inflammatory processes of the cecum, colon and sigmoid colon - typhlitis, colitis, sigmoiditis.
- nonspecific ulcerative colitis;
- appendicitis;
- acute intestinal infections;
- helminthiases;
- diseases of the rectum - proctitis, paraproctitis, hemorrhoids, anal fissures;
- cancer of various parts of the large intestine;
- colonic benign tumors, polyps;
- colonic obstruction caused by paralysis of smooth muscles, blockage of the intestinal lumen by a tumor, and other reasons.
Typical symptoms of chronic diseases:
- widespread aching abdominal pain;
- bloating, flatulence ;
- diarrhea, constipation , their alternation;
- pain, feeling of incomplete bowel movement after bowel movement;
- admixture of mucus, blood in the stool;
- dark “cherry” or tarry stools are a sign of intestinal bleeding.
Intestinal obstruction and other acute diseases are characterized by the patient’s severe general condition. Peritonitis (inflammation of the peritoneum) with sharp pain and tension in the muscles of the abdominal wall is possible. Intoxication is accompanied by nausea and vomiting. With intestinal obstruction, vomiting may take on a fecal character.
Chronic diseases of the large intestine, as a rule, occur against the background of dysbiosis with emaciation, anemia, vitamin deficiencies, and decreased immunity.
Pain syndrome with damage to the large intestine
Many different diseases can cause pain in the large intestine. A number of factors lead to the development of such violations:
- sedentary lifestyle;
- eating disorders, including frequent overeating or following a strict diet;
- abuse of spicy, fatty, smoked foods;
- disruption of the digestive system in patients due to advanced age;
- chronic constipation;
- hypotension accompanied by impaired peristalsis;
- constant use of pharmacological drugs.
These factors can cause disturbances in the functioning of both the entire digestive tract and the large intestine separately. At the same time, it is usually quite difficult to establish the cause of the pain syndrome, and almost impossible on your own. In general, dysfunctions of the digestive system can be divided into two main groups:
- inflammatory in nature: colitis, diverticulitis, Crohn's disease, etc.;
- non-inflammatory disorders: atonic constipation, tumor processes, endometriosis, etc.
Diseases of the large intestine can significantly impair the patient's quality of life. To prevent the development of complications, it is necessary to promptly pay attention to the appearance of alarming signs of pathology.
Ulcerative colitis
Ulcerative colitis is an inflammatory lesion of the tissues of the large intestine. The disease has a chronic course and is characterized by fairly frequent relapses. To date, it has not been possible to accurately determine the cause of the development of the pathology, but it is classified as a disorder of autoimmune origin.
Colitis is most often detected in people of two age groups: patients 25-45 years old and patients over 55-60 years old.
There are three categories of disease progression:
- acute colitis;
- chronic with periodic exacerbations;
- chronic continuous, in which remission is not observed for 6 months or more.
The clinical picture of ulcerative colitis is generally synonymous with other diseases of the large intestine and is manifested by the following symptoms:
- Intense, long-lasting abdominal pain. Their localization largely depends on which part of the colon was affected by the pathological process.
- Diarrhea or constipation. In this case, bloody inclusions may be observed in the feces.
- Signs of intoxication of the body: nausea, cephalalgia, dizziness, drowsiness and lethargy.
Lack of therapy for colitis can lead to perforation of the intestinal wall and, as a consequence, massive intestinal bleeding. This condition is life-threatening for the patient.
Colitis therapy should be carried out comprehensively, taking into account the severity and form of the disease. In case of radical damage to the intestine, the patient is indicated for hospitalization. Therapy for ulcerative colitis:
| Drug name | Image | pharmachologic effect |
| Mesalazine | Anti-inflammatory and antimicrobial agent | |
| 5-ASK | Anti-inflammatory and cytoprotective effects | |
| Prednisolone | Anti-inflammatory, immunosuppressive effect | |
| Cyclosporine | Immunosuppressant |
Crohn's disease
Crohn's disease is a chronic inflammatory bowel disease, which is characterized by the formation of ulcerations on the intestinal mucosa, in place of which granulomas subsequently grow, adhesions and strictures form, which narrows the intestinal lumen and impairs its patency.
Researchers have identified several factors that are important in the mechanism of chronic intestinal inflammation, but the trigger point in the pathological process is not known. Contributing factors include:
- Failure in the body's immune system. In the mechanism of maintaining inflammation, the autoimmune component plays an important role, that is, the pathological reaction of the immune system to the body’s own tissues, as well as to those intestinal microorganisms that are not pathogenic and are necessary for the absorption of food;
- Hereditary predisposition. It is known that people with Crohn's disease often have relatives suffering from chronic inflammatory bowel diseases, such as ulcerative colitis;
- The damaging effects of external factors: unhealthy diet, bad habits, unhealthy lifestyle, infection.
Drug treatment of Crohn's disease during an exacerbation consists of the use of antidiarrheals, anti-inflammatory drugs (hormonal therapy with corticosteroids), antibacterial drugs and drugs that suppress excessive activity of the immune system (immunosuppressants).
Therapy for Crohn's disease
| Drug name | Image | pharmachologic effect |
| Sulfasalazine | Anti-inflammatory, antibacterial effect | |
| Budenofalk | Decongestant, antihistamine effect – corticosteroid | |
| Azathioprine | Immunosuppressive drug | |
| Imodium | Antidiarrheal agent | |
| Acetaminophen | Analgesic effect |
Diverticular disease
Diverticular disease of the colon, a disease characterized by the formation of multiple thinned protrusions of the mucous membrane on the intestinal walls beyond the intestinal wall, most often affects patients in older age groups. According to statistics, the occurrence of colon diverticulosis in the age group under 40 years old occurs in less than 5%. At older ages, the disease occurs more often, and in patients over 85 years of age, this disease is registered in 65% of cases.
Factors that, according to experts, influence the development of diverticular disease include:
- genetic predisposition
- lack of physical activity
- obesity
- smoking
- decrease in beneficial gut bacteria
- increase in pathogenic bacteria in the intestines
- taking certain medications, including steroidal and nonsteroidal anti-inflammatory drugs such as ibuprofen
The older a person is, the higher the risk of developing diverticular disease. The 40-year mark is considered a milestone. In general, by the time they reach their 80th birthday, most people have this disease.
Therapy for diverticular disease
| Drug name | Image | pharmachologic effect |
| Cefoxitin | Antibacterial action | |
| Portalac syrup | Prebiotic with laxative effect | |
| Domperidone | Stimulation of gastrointestinal motility | |
| No-shpa | Antispasmodic effect | |
| Tylenol | Analgesic effect |
If there is no effect from conservative therapy, the patient needs surgical intervention.
Malignant neoplasms
Neoplasms of the large intestine can be both malignant and benign. At the same time, the first group of tumors is characterized by slow growth and does not cause a significant deterioration in the patient’s quality of life.
Carcinomas develop more aggressively, which leads to the appearance of a characteristic clinical picture of cancer:
- attacks of vomiting, admixture of feces in the vomit;
- loss of appetite leading to cachexia;
- lethargy, drowsiness, weakness;
- low-grade fever;
- stool disorders;
- melena - black stool mixed with blood;
- cutting and tearing pain in the area of tumor formation.
The thick gastrointestinal tract is an important part of the digestive system. Pain in this part of the gastrointestinal tract may indicate the development of serious pathologies and require urgent consultation with a specialist.
Diagnostics
Diagnosis of the large intestine begins with a digital examination of the anus. Next, laboratory and instrumental studies begin. , endoscopy of the large intestine is diagnostically valuable - sigmoidoscopy and colonoscopy . During sigmoidoscopy, the doctor examines the rectum and sigmoid colon, and during colonoscopy, the entire large intestine.
Irrigoscopy is an X-ray diagnosis of the large intestine after filling through the anus with a contrasting barium suspension. Plain radiography of the abdominal organs without the use of contrast is informative in case of intestinal obstruction. The so-called Kloiber cups, horizontal fluid levels in the intestinal lumen. This is a symptom specific to intestinal obstruction.
Of the laboratory tests, the main place is occupied by the diagnosis of stool. Depending on the tasks assigned, feces are taken for:
- general analysis (coprogram);
- occult blood;
- worm eggs;
- bacterial culture on nutrient media.
A supporting role is played by a general and biochemical blood test, immunodiagnostics and blood culture on nutrient media.
The role of bacteria in the digestive process
Everything that enters the human body is processed, broken down and absorbed, bringing benefit or harm, but always leaves behind some waste or undigested particles. The functions of “cleaning” and “removing” in the body are performed by bacteria of the large intestine, which are part of the healthy microflora.
Our digestion largely depends on these bacteria. According to scientists, there are about five hundred different types of bacteria in the human gastrointestinal tract. Only 30-40 varieties of them are the main “workers”.
The relationship between the host organism and bacteria constitutes a harmonious symbiotic system, i.e. they are mutually beneficial. The body gives bacterial cells food and a “place in the sun,” and in return they perform the extremely important work of processing food, removing residues, strengthening the immune system, protecting against dangerous viruses, etc.
What is diverticular disease (diverticulosis) of the colon?
Diverticula (Latin diverticulum - literally “branch”, “road to the side”) are understood as sac-like protrusions of all layers of the wall of the colon or only the mucous membrane and submucosal layer through a defect in the muscle layer.
Figure 1. Section of the colon. Diverticulum
Colon diverticulosis is a condition in which there is at least one diverticulum in the colon.
Figure 2. Diverticulosis of the left colon
Diverticular disease is a disease characterized by clinical manifestations of the inflammatory process and its possible complications - abscesses, perforation of diverticula, fistula formation, peritonitis, and bleeding.
Introduction
Over the past 20 years, the number of patients with diverticular disease has increased significantly, which is primarily due to changes in the nature of nutrition, a decrease in fiber and dietary fiber in the diet and, as a consequence, the development of constipation. For patients suffering from diverticular disease, as well as their relatives, it is important to understand all stages of development, methods of diagnosis and treatment of this disease. To fully understand the pathological process, it is necessary to begin studying the issue from the basics - the anatomical features of the organ.