01.11.2017
Interesting
Bogacheva Sharofat Bairovna
The brain is a “mystical” organ that can fill us with incredible sensations, show us our own “movie”, dreams, accumulate experience and wisdom that allows us to think. This is an organ that controls and regulates the functioning of the entire organism as a whole and each organ and system separately; providing the balance, protection, and compensatory reactions to disturbances necessary for our body. This small organ, weighing about 1400–1500 g (2% of body weight), has incredible abilities that have not yet been fully studied.
What does the brain need? Working without rest day and night, he is in dire need of oxygen (the brain consumes 20% of all oxygen entering the body) and nutrients, without which he cannot live even for a few minutes. It is a known fact that oxygen reserves are not created in the brain, and there are no substances that can nourish it under anaerobic (in the absence of oxygen) conditions. That is, the nerve cells of the brain constantly need oxygen, glucose and “cleaning” (cleansing of cell waste products).
Excursion into physiology
The uninterrupted supply of substances necessary for the nerve cells of the brain and the cleansing of waste are carried out by the cerebral circulatory system, where arterial blood carries oxygen and nutrition to the brain, and venous blood removes toxins and metabolic products.
The vessels of the brain have a unique, perfect structure that ideally regulates blood flow, ensuring its stability. They are designed in such a way that with an increased flow of blood into large vessels, the strong pulse impulse of the blood coming from the heart is weakened due to numerous bends (siphons) of the vessels along the vascular bed, which contribute to the pressure drop and smoothing of the pulsating blood flow. Due to complex regulatory mechanisms, when total blood pressure increases, the pressure in the brain remains stable for a long time. Regulatory systems allow blood flow to be redistributed from parts of the brain with less load to areas with increased brain activity.
The brain has an autonomous regulatory system, which allows it to be in a healthy functional state and control the processes of continuous adaptation of the body to constantly changing conditions of the external and internal environment. In a state of functional rest, the brain receives 750 ml of blood per minute, which is 15% of cardiac output. In children, blood flow activity is 50–55% higher, and in elderly people it is 20% lower than in adults.
It should be noted that the gray matter of the brain (cell bodies of neurons) is supplied with blood more intensively than the white matter (conducting pathways), which is due to greater cell activity. Thus, during intense mental work, local blood flow in the cerebral cortex can increase 2–3 times compared to the resting state.
The brain has the richest capillary network. Nerve cells are not only intertwined, but also penetrated by capillaries. The vessels of the brain are connected to each other by collaterals (“bridges”). Arterial collateral circulation of the brain, important for maintaining normal blood flow, plays a particularly significant role in compensating for circulatory disorders when one of the cerebral arteries is blocked.
With a high intensity of blood flow in the vessels of the brain, the blood pressure in them is maintained relatively constant. A complex chain of regulatory mechanisms protects the brain from a drop in blood pressure and hypoxia (decreased oxygen). Along the path of blood flow to the brain, there are many sensitive cells (pressoreceptors, chemoreceptors) that can respond to blood pressure and regulate heart rhythm and vascular tone.
The activity of the vasomotor centers of the brain is associated not only with nervous and humoral regulation mechanisms, but also with the autonomic regulation system, which allows, despite significant fluctuations in total blood pressure, to maintain cerebral blood flow at a constant level.
Thus, cerebral circulation is provided with complex regulatory mechanisms that make it possible to maintain a constant supply of the substances it needs.
With excessive blood supply to the brain, excessive hydration (fluid accumulation) may occur, followed by the development of edema and damage to vital centers that are incompatible with life. The cause of excess blood supply can be, for example, an increase in systemic blood pressure to 160–170 mm Hg. Art. and higher.
In the problem of impaired blood supply to the brain, much attention is paid to arteries. But venous circulation is no less important. The veins carry out the removal of waste substances (toxins) with the blood - that is, cleansing the brain. Thanks to these vessels, constant intracranial pressure is maintained.
Violation of the venous outflow leads to stagnation of blood and accumulation of fluid in the brain, causes hydrocephalus with compression of the brain centers, and contributes to the occurrence of phlebitis and thrombophlebitis.
There is one more feature of the cerebral veins that must be taken into account. The wall of a venous vessel in the brain does not have a valve apparatus, unlike, for example, the veins of the extremities (valves help withstand loads by moving blood upward and preventing it from moving in the opposite direction). Therefore, venous blood in the vessels of the brain passes freely in both directions, depending on the pressure that arises. This creates a danger of rapid spread of infection from the sinuses and eye sockets, which is facilitated by the atomic structure of the nose and its paranasal sinuses, located in close proximity to the brain. When coughing, venous pressure increases, reverse venous flow, congestion, and brain hypoxia become possible. There are known cases of loss of consciousness during a coughing attack in the presence of a chronic respiratory tract disease and in young children when they “go into a fit” of coughing during illness and crying and screaming until they cough.
It becomes clear why long-term respiratory problems, accompanied by constant swelling and coughing, can cause cerebrovascular accidents. Because they not only cause brain hypoxia, but also disrupt venous outflow and, being a constant source of infection, contribute to its penetration into the brain.
An ophthalmologist, for example, can observe manifestations of congestion in the brain (dilated, blood-filled vessels of the fundus). But this is also visible to the naked eye: red, puffy eyes after sleep (due to drinking alcohol the night before, overeating at night, lack of sleep) are a symptom of congestion in the brain.
After a brief excursion into physiology, it becomes clear that the reasons for the deterioration of cerebral circulation may be associated with disturbances in the flow of blood to the brain and the outflow of blood from the brain.
Circulatory disorders of the lower extremities
General information
The human blood circulation is a closed vascular pathway that provides a continuous flow of blood, carrying oxygen and nutrition to cells, carrying away carbon dioxide and metabolic products. Blood, saturated with nutrients and oxygen, moves through the arteries from the heart to the organs and tissues. If blood flow in the arteries supplying the lower extremities is impaired due to the progression of atherosclerosis, then their tissues receive insufficient oxygen and nutrients and a disease called “peripheral artery disease” or “leg artery disease” develops.
Symptoms of circulatory disorders:
- feeling of discomfort/pain when walking;
- pain in the areas of the lower extremities (foot, shin, knee).
The risk of developing the disease increases with age. In the age group over 70 years, one in three people suffers peripheral artery In addition, smoking and diabetes increase the risk of developing this disease.
In rare cases, disease of the peripheral arteries of the lower extremities is asymptomatic. A common symptom of the disease is intermittent claudication. It is expressed in discomfort in the lower extremities, which occurs when walking and disappears when it stops. The patient may experience pain and the following symptoms:
- convulsions;
- weakness in the lower extremities;
- intermittent lameness (when going up).
As the disease progresses, intermittent claudication begins to occur over increasingly shorter distances. Ischemia of the lower extremities occurs when the blood supply to the tissues in the extremities is severely impaired. The tissues do not receive enough oxygen and nutrients, so severe pain occurs. Localization of pain from the hip to the fingertips, intensifies with minimal physical activity on the lower extremities. In severe forms of the disease, the following symptoms may occur:
- the appearance of dry skin;
- decrease in temperature;
- pale skin;
- the appearance of trophic ulcers.
If left untreated, soft tissue necrosis and gangrene of the lower extremities develop.
Causes of circulatory disorders in the lower extremities
Diseases that cause circulatory problems in the lower extremities can be different. Among them:
- Obliterating atherosclerosis of the great vessels. It ranks first among other arterial diseases. It disables work and is localized mainly in large vessels.
- Obliterating endarteritis (thromboangiitis). A systemic chronic inflammatory disease that affects the small arteries of the extremities. The average age at which the disease appears is 30-40 years.
- Vascular damage in diabetes mellitus.
- Phlebeurysm.
- Thrombophlebitis.
The cause of thromboangitis has not been established to date. In diabetes mellitus, damage to the arteries of the lower extremities occurs 3-5 times more often than in people free from this endocrine disease. The circumstance suggested the presence of a genetic connection between diabetes and atherosclerotic processes in the arteries. In diabetes mellitus, atherosclerosis occurs in complex forms. About 40-50% of lower limb amputations are performed on patients with diabetes. Factors causing circulatory disorders in the extremities:
- Smoking;
- Diabetes;
- Excess body weight by more than 30%;
- High blood pressure;
- high cholesterol or triglycerides;
- Increased level of homocysthenia.
Prevention of circulatory disorders in the lower extremities
Normal blood circulation is an important factor in the healthy functioning of the body. To maintain blood circulation, take care of yourself, your diet and active lifestyle. Great for stimulating blood circulation:
- bath;
- sauna;
- cold and hot shower;
- massage.
There are drugs to improve blood circulation - antispasmodics, antiplatelet agents (prevent platelet aggregation), anticoagulants (normalize blood microcirculation), angioprotectors (reduce vascular permeability). Phyto or homeopathic medicines are considered safe at the initial stage of disease development. Self-medication is dangerous; it is better to consult a doctor before doing so. It will help you choose the most optimal option for medications for the treatment and prevention of peripheral circulation.
What happens when blood pressure rises?
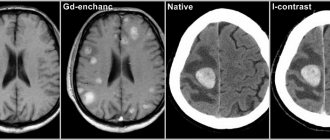
At first, vascular tone is slowly disrupted. Over time, if elevated blood pressure (BP) persists, minor cerebral hemorrhages and strokes may occur.
As a result of a constant increase in blood pressure during hypertension, plasma (part of the blood without formed elements) is released, which ultimately leads to the destruction of the walls of blood vessels.
How does this happen? A specific protein (hyaline-like substance, similar in structure to cartilage) is deposited on the walls of blood vessels, which leads to the development of hyalinosis. The vessels become like glass tubes, lose their elasticity and ability to hold blood pressure. In addition, the permeability of the vascular wall increases, and blood can freely pass through it, soaking the nerve fibers (diapedetic bleeding). The result of such transformations can be the formation of microaneurysms and rupture of the vessel with hemorrhage and blood entering the white medulla. The resulting swelling and hematomas lead to further hemorrhages (hemorrhagic stroke).
Atherosclerosis that accompanies hypertension, or exists without it (which is rare), contributes to cerebral ischemia - insufficient supply of nutrients and oxygen to the tissues (except for atherosclerotic plaques that narrow the lumen of the arteries, the blood itself can be thick and viscous).
Acute circulatory disorders are strokes (hemorrhagic and ischemic). But it all starts with transient cerebrovascular accidents against the background of hypertension and atherosclerosis, as well as obesity, diabetes mellitus, and respiratory diseases that often accompany them.
Symptoms of cerebrovascular accident
When a lesion forms in the brain with impaired blood supply, the patient may experience numbness in half of the body (on the side opposite to the lesion) and part of the face around the lips; short-term paresis of the limbs or other parts of the body and face is possible. Speech is impaired and an epileptic seizure may occur.
If there is a circulatory disorder, depending on the location of the lesion, the legs and arms may become weak, the head may become dizzy, the patient may have difficulty swallowing and pronouncing sounds, photopsia (appearance of luminous spots, sparks, etc. in the eyes) or diplopia (doubling of visible objects) may occur. . The person loses orientation and has memory lapses.
Signs of impaired cerebral circulation due to hypertension are manifested in the following: the head and eyeballs begin to hurt very much, the person experiences drowsiness, he experiences stuffiness in the ears (like on an airplane during takeoff or landing) and attacks of nausea. The face turns red and sweating increases.
Unlike strokes, all these symptoms, which are called “transient attacks,” disappear within 24 hours.
Chronic cerebrovascular accident (CVA), unlike acute forms, develops gradually. There are three stages of the disease:
- At the first stage, the symptoms are vague. They are more like chronic fatigue syndrome. A person quickly gets tired, becomes hot-tempered and absent-minded, and forgets some minor points. His sleep is disturbed, his mood often changes, his head hurts and he feels dizzy.
- At the second stage, chronic cerebrovascular accident is accompanied by significant memory deterioration, and minor motor dysfunctions develop, causing unsteadiness in gait. There is a constant noise in my head. A person perceives information poorly, having difficulty concentrating his attention on it. Becomes irritable and unconfident, loses intelligence, reacts inadequately to criticism, and often becomes depressed. He gradually degrades as a person and adapts poorly socially. He constantly feels dizzy and has a headache. He always wants to sleep. Performance is significantly reduced.
- In the third stage, all symptoms intensify. Personality degradation turns into dementia, memory suffers. Having left home alone, such a person will never find his way back. Motor functions are impaired, which manifests itself in hand tremors and stiffness of movements. Speech impairment and uncoordinated movements are noticeable.
Working out the back of the neck
As we have already found out, the problem arises due to compression of blood vessels, which is a consequence of the incorrect position of the vertebrae. Gymnastics will help solve and even more so prevent such a situation. For urgent help, you can gently influence the vessels. Let's take a closer look at how to do all this.
Gymnastics for the neck
Gymnastics should be performed regularly. Spend just 3-5 minutes a day and you will almost 100% protect yourself from headaches. A bonus is the prevention of high blood pressure – both intracranial and arterial.
There are many sets of exercises for the neck; you can see in detail, with step-by-step instructions and explanations, in Dr. Shishonin’s publications on cervical osteochondrosis. You've probably already read these articles and watched the videos, so let's briefly remind you. Tilts and rotations of the head, movements of the neck should not be performed abruptly, but carefully, so that there are pleasant sensations similar to those you experience when stretching after sleep.
Triggering a reflex response
The back of the neck can be treated with a piece of ice. The temperature effect causes a reflex reaction of the vessels: they react by restoring their shape. Dr. Shishonin spoke in detail about these techniques in specialized articles on cervical osteochondrosis.
Here we just remind you that you need to work with ice carefully. Don’t be afraid, you physically won’t be able to harm yourself, but don’t overdo it, otherwise the effect will be worse than from a delicate influence.
Consequences of cerebrovascular accidents
Disability is a sad result of acute and in many cases chronic cerebrovascular accident.
Acute cerebrovascular accident has serious consequences. In most cases, a person who has suffered a stroke becomes completely helpless. He cannot eat, perform hygiene procedures, dress, etc. on his own. Such people have a completely impaired ability to think. They lose track of time and have absolutely no orientation in space.
Some people retain the ability to move. But many people, after a cerebrovascular accident, remain bedridden forever. Many of them maintain a clear mind, understand what is happening around them, but are speechless and cannot express their desires and feelings in words.