Pharmacological properties of the drug Tagista
A synthetic analogue of histamine, has a histamine-like and vasodilating effect. It is a weak H1-histamine receptor agonist and a fairly powerful H3-histamine receptor blocker. It has 3 levels of action: on the cochlear blood flow, on the central vestibular apparatus and on the peripheral vestibular apparatus. The action of betahistine includes: vasodilation in the inner ear, which is realized indirectly through H3- and H1-histamine receptors, inhibitory effects on the vestibular nuclei, which are realized directly through H3-histamine receptors, inhibiting effects on the impulse activity of the ampullary receptors. Through a direct agonistic effect on the H1-histamine receptors of the vessels of the inner ear, located, in particular, in the stria vascularis and precapillary sphincters of the microvasculature of the said area, as well as indirectly through the effect on H3-histamine receptors, it improves microcirculation and capillary permeability, normalizes endolymph pressure in the labyrinth and cochlea increases blood flow in the basilar arteries. It has a pronounced central effect, being an antagonist of H3-histamine receptors in the nuclei of the vestibular nerve, and also normalizes neuronal transmission in polysynaptic neurons of the vestibular nuclei at the level of the brain stem. By indirectly acting on H3-histamine receptors, it increases the content of the neurotransmitter serotonin in the brain stem, which reduces the activity of the vestibular nuclei. Helps eliminate disorders of both the vestibular and cochlear apparatus: reduces the frequency and intensity of dizziness, reduces tinnitus, and helps improve hearing in cases of hearing loss. Stimulates H1-histamine receptors rather than blocks them, therefore does not have a sedative effect and does not cause drowsiness.
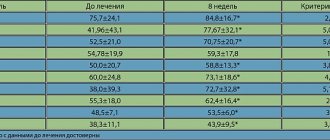
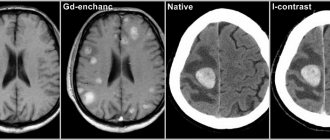
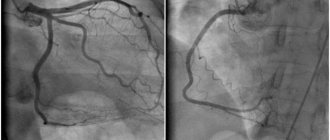
Tagista – control over dizziness today
Dizziness can be defined as a feeling of disorientation of the body in space, accompanied by the illusion of movement of the patient or objects around him. During ontogenesis, a person develops a certain idea of the relationship with surrounding objects (space); The main role here is played by information entering the central nervous system (CNS) from the vestibular apparatus, the organ of vision, and nerve endings that perceive deep and cutaneous sensitivity. When the transmission or perception of this information is disrupted, dizziness occurs [2]. Dizziness can occur in healthy people, for example, with excessive or prolonged irritation of the vestibular apparatus (movement with significant linear or angular acceleration, rocking, etc.), due to intense rhythmic irritation of the receptors of the eyeballs (with prolonged fixation of the gaze on a moving object) or in the absence of in the external space of familiar points that determine spatial orientation (at height). The cause of dizziness is an imbalance of sensory information coming from the main afferent systems that provide spatial orientation - vestibular, visual and proprioceptive (Table 1) [6, 8, 10]. A classification generally accepted in clinical practice involves dividing dizziness into systemic (rotational, vertigo), often caused by the peripheral level of damage to the vestibular analyzer, and non-systemic, predominantly occurring with central vestibular disorders or without involvement of vestibular anatomical formations in the pathological process, for example, with psychovegetative disorders [1, 9]. Peripheral vertigo is characterized by vectoriality of sensory sensations - rotation of either the patient himself in relation to surrounding objects, or the environment in relation to the patient. The feeling of vector movement is accompanied by imbalance, fear, the desire to hold tightly to support, nausea, vomiting, and autonomic disorders. Peripheral vestibular disorders have a sudden onset, varying duration - usually no more than a few days. Intense dizziness, aggravated by turning the head, is often combined with hearing loss and tinnitus. In this case, there are no focal neurological symptoms. Central vestibulopathies have a smooth, gradual onset, a long duration (weeks, months), and imbalances are often moderately expressed. Focal neurological symptoms are recorded. Non-systemic dizziness is characterized by an imbalance of the type of ataxia without an accent on the side, a feeling of “lightheadedness”, heaviness in the head, accompanied by a blurred perception of the surrounding world, unsteadiness of gait, and loss of orientation in space. Improving the quality of diagnosis and the effectiveness of treatment for dizziness is one of the unresolved problems of practical medicine that has important medical and social significance. The relevance of this problem is largely determined by the high prevalence of dizziness. Dizziness is one of the most common symptoms in patients with chronic disorders of the blood supply to the brain, especially with pathology of the vertebrobasilar system. In this group of patients, dizziness is usually caused by age-related changes in the sensory system, a decrease in the compensatory capabilities of the central mechanisms for maintaining balance, and cerebrovascular insufficiency with a predominant lesion of the vertebrobasilar system. In this case, changes in the vestibular nuclei of the brainstem or vestibulo-cerebellar connections play a major role, but the so-called “peripheral” component, caused by atherosclerotic lesions of the vessels of the inner ear, is also of certain importance [2, 5, 6]. Dizziness may occur with secondary hypotension due to cerebrovascular diseases, Parkinson's disease, diabetes mellitus, alcoholism, and spinal cord tumors. The appearance of dizziness in stable arterial hypertension can be caused by long-term disruption of the regulation of cerebral circulation and microcirculation of the labyrinths, metabolic disorders of the vestibular structures, vascular tone and venous outflow from the cranial cavity, the presence of cerebral atherosclerosis in the patient, and stenotic lesions of the brachiocephalic vessels. The occurrence of dizziness is provoked by negative weather conditions, stressful situations, infectious diseases, and injuries [6]. In the clinic of neurological manifestations of cervical osteochondrosis, a special place is occupied by syndromes accompanied by severe dizziness. This is the so-called vertebrogenic vertebral artery syndrome, or posterior cervical sympathetic syndrome, which is caused by the impact of pathological bone and cartilage structures on the vertebral artery. Most often, the wall of the vessel is affected by uncovertebral growths, which deform the medial wall of the vessel or injure the surrounding sympathetic plexus, causing spasm of the artery and its branches. Manifestations of the syndrome unfold in the areas of vascularization of the branches of the vertebral artery. The clinical picture consists of headaches of occipital localization with frontal distribution, visual disturbances (in the form of subjective sensations of “fog”, “sand in the eyes”) and cochleovestibular disorders. The latter often come to the fore and are manifested by systemic and non-systemic dizziness, sometimes with nausea, vomiting, paraacusis (noise, hum, crackling) and hearing loss on the affected side [1, 3, 4, 7]. Angiogenic vestibular disorders acquire particular significance in the geriatric age group. Age-related static disorders - presbyastasis, characteristic of older age groups, are caused by involutional processes, impaired blood supply to the labyrinth due to ischemia, microcirculatory disorders, changes in the rheological properties of blood, and atherosclerosis. Postural disorders are aggravated by natural aging of the musculoskeletal, nervous systems and vision, diseases of the musculoskeletal system, cardiovascular system, and post-traumatic syndromes [2, 6, 7]. It should also be noted that there is a high incidence of dizziness (more than 20%) as a symptom in patients who have suffered uncomplicated concussions. The histaminergic system plays an important role in the functioning of the vestibular structures. Thus, the transmission of impulses from vestibular receptors and vestibular nuclei is provided primarily by histaminergic neurons. The main source of histaminergic innervation is the posterior hypothalamus, mainly the tuberomammillary nucleus. Neurons of the tuberomammillary nucleus are connected with almost all structures of the diencephalic region and telencephalon, including the basal ganglia and cortex, as well as with the brainstem and, in particular, with the vestibular nuclei complex [1, 9, 11]. Histaminergic innervation is most represented in the medial vestibular nucleus. In peripheral vestibular disorders, there is an increase in spontaneous impulses of neurons of the ipsilateral vestibular nuclei, mainly the medial one. At the same time, there is a decrease in the expression of GABA receptors, which leads to the predominance of stimulating histaminergic influences. In addition, there is an increase in the density of GABA receptors in the contralateral medial vestibular nucleus. The histaminergic system also ensures the transmission of excitation between the vestibular nuclei and the vomiting center. Serotonergic, noradrenergic and dopaminergic innervations have a certain significance in the formation of connections of the vestibular system. Thus, dizziness is a common symptom of many diseases that doctors of various specialties encounter in their practice. One of the most difficult areas in solving the problem of dizziness is the optimization of therapeutic measures, in particular, the use of rational pharmacotherapy. A large number of medications from different therapeutic groups are used to treat dizziness, but only a very small number of them have a truly proven vertigolytic effect in research and practice [11, 12]. One of the drugs that has a structural similarity to histamine, an affinity for blocking H3 and stimulating H1 receptors, is the drug Tagista, containing betahistine hydrochloride. Betahistine was first used in 1962 for the treatment of cluster headaches, and in 1965 its positive effect was noted in Meniere's disease. In 1970, betahistine was registered in Europe as a medicinal product. In the last 20 years, a large number of studies have been carried out to evaluate the effectiveness of betahistine, incl. a number of double-blind studies. Currently, Tagista is a clinically proven effective drug for the treatment of Meniere's disease and other vestibular disorders caused by damage to the peripheral part of the vestibular analyzer [5, 8]. Due to the blockade of H3 receptors, betahistine increases the release of neurotransmitters from the nerve endings of the presynaptic membrane, has an inhibitory effect on the vestibular nuclei of the brain stem and improves blood supply to the inner ear. The drug has a local powerful stimulating effect, increasing the release of neurotransmitters (histamine) from the nerve endings of the receptor cells of the inner ear into the synapse. Neurotransmitters act on the precapillary sphincters, causing vasodilation of the vessels of the inner ear, increasing their permeability and thereby normalizing intralabyrinthine pressure, i.e. eliminating hydrops. The effectiveness of betahistine is associated with a decrease in both spontaneous and evoked impulses from vestibular receptors and vestibular nuclei. Thus, in the experiment, the administration of the drug led to a dose-dependent decrease in the frequency of spontaneous impulses from the receptors of the semicircular tubules. In addition, betahistine reduces the intensity and amplitude of firing of neurons of the lateral vestibular nucleus both at rest and during stimulation. Betahistine also stimulates the synthesis of endogenous histamine, as evidenced, in particular, by increased synthesis of messenger RNA encoding histidine decarboxylase, the main enzyme in histamine synthesis. Along with its effect on histamine receptors in the peripheral and central vestibular structures, betahistine has a vasoactive effect. The drug causes dilation of the arterioles and capillaries of the inner ear, which leads to a selective increase in blood flow. In addition, while taking the drug, there is a slight increase in cerebral blood flow in both the vertebrobasilar and carotid areas, which leads to an improvement in cognitive functions in patients with chronic cerebrovascular insufficiency. The administration of betahistine reduces the frequency, severity and duration of attacks of systemic dizziness. Along with the positive effect on vestibular function, there is also an improvement in hearing during treatment, which is apparently due to the vasoactive effect of the drug. In the work of O.V. Veselago (2010) conducted a study of the effectiveness of Tagista in relation to vestibular disorders in patients with chronic cerebral ischemia. Vestibular disorders in patients with discirculatory encephalopathy (DE) were most often represented by short-term, almost daily episodes of systemic dizziness, occurring mainly when turning the head to the side (“the image does not keep up with the eyes”), oscillopsia, visual dizziness (“wavering shadow” symptom), instability when walking (“throws to the sides”), lack of coordination [5]. Against the background of chronic dizziness, extensive attacks of systemic dizziness could also occur, accompanied by nausea and vomiting, falling, and loss of consciousness. Sometimes the attacks were accompanied by auditory symptoms: noise in the ears or head, ear congestion, hearing loss. The main group consisted of 56 patients with DE (30 women and 26 men aged from 42 to 88 years, average age - 68.5 years). Patients in the main group received a standard course of treatment with Tagista lasting 60 days (24 mg 2 times a day) without any change in basic therapy (hypotensive, vascular, neurometabolic). The control group consisted of 30 patients with DE (16 women and 14 men aged from 43 to 84 years, average age - 63.5 years). Patients in the control group received only basic therapy [5]. In addition to general clinical and neurological examinations, all patients underwent CT or MRI studies of the brain, duplex scanning of the main arteries of the head, and a study of acoustic brainstem evoked potentials. Otoneurological examination was carried out twice - at the beginning and end of the course of treatment according to the generally accepted method of N.S. Blagoveshchenskaya. The effectiveness of treatment was assessed based on the analysis of subjective data (patient complaints of dizziness, imbalance, oscillopsia, etc.) and the results of an objective otoneurological examination. After the course of treatment in patients of the main group who received Tagista, a significant disappearance or reduction in the severity of subjective complaints and an improvement in objective indicators were observed in 71.4% of cases. In the control group, the same figure was 36.7%. The effectiveness of Tagista in relation to vestibular disorders in patients of the main and control groups is shown in Table 2. Since in 12 patients of the main group, along with damage to the central parts of the vestibular analyzer, peripheral vestibular syndrome (PVS) was also observed, to exclude the possibility of interpreting the positive effect of Tagista only Due to the effect on the peripheral part of the vestibular analyzer, we conducted a comparative analysis of the effectiveness of using this drug in patients with only central vestibular syndrome (CVS) compared with those with mixed symptoms - CVT and PVS. The results of the study are presented in Table 3. There were no statistically significant differences in the results of the effectiveness of Tagista in CVS and mixed vestibular syndrome. The research results show almost the same effectiveness of Tagista in PVS and CVS, as well as in their combination. Tagista is also effective for relieving attacks of acute dizziness (vertigo). The drug reduces the frequency of attacks, thereby providing a preventive effect. The purpose of another study on the use of Tagista in patients with vestibular vertigo and verified Meniere's syndrome in an outpatient setting was to evaluate the clinical efficacy and tolerability of Tagista in the symptomatic treatment of vestibular vertigo (vertigo) and Meniere's syndrome [8]. The study included 32 patients: 16 women and 16 men aged from 25 to 67 years (average age - 53.4±10.7 years) with vestibular vertigo and Meniere's syndrome, observed in 5 district neurological departments of Moscow. The study included patients with systemic persistent or paroxysmal dizziness of established etiology; with frequent (at least 3 times a week) attacks of any severity and a total duration of more than 1 month. The main causes of dizziness were chronic cerebral ischemia - in 17 (53.1%) people; dyscirculation in the vertebrobasilar system against the background of osteochondrosis of the cervical spine – in 14 (43.75%); 1 (3.15%) patient was diagnosed with Meniere's disease. To assess the effectiveness of therapy, the dynamics of neurological symptoms were studied, and a number of additional techniques were used: vestibular tests (nystagmus - spontaneous, optokinetic, positional); vestibulospinal tests (Romberg test, Unterberger step test, Barany index test); dizziness scale; method of rapid assessment of well-being, activity and mood (SAM) in a modified version by V.A. Doskina; Clinical Global Impression (CGI) scale, which is used to further quantify the possible deterioration or improvement of the patient's mental state during therapy. Scores on this scale vary from 1 to 7 points: 1 – “very significant improvement”, 2 – “significant improvement”, 3 – “minimal improvement”; 4 – “no changes”, 5 – “minimal deterioration”, 6 – “moderate deterioration”, 7 – “significant deterioration”. In addition, a score was used to assess the tolerability and effectiveness of the drug (0–4 points). All patients were prescribed Tagista at a dose of 48 mg/day. (2 tablets of 24 mg 2 times/day). It was part of complex therapy: patients continued to take basic antihypertensive therapy, antiplatelet agents, and were also prescribed therapeutic exercises and stabilization training with biofeedback on a stabiloplatform - 10 procedures using standard methods. The duration of treatment was 4 weeks. The condition of the patients was studied before and after the course of treatment. At the end of the course of treatment, all patients showed a general improvement in well-being and mood, and an increase in daily activity. Patients less pessimistically evaluated their condition and prognosis of the disease, were tuned to further maintenance treatment. There was a distinct positive dynamics regarding the severity of the actual cochleo -investbular disorders: dizziness, hearing impairment, ataxia. Statistically significant changes were observed in the study of vestibulospinal samples: the severity of static ataxia in Romberg’s sample and hit the lamb sample has significantly decreased. In 71.9% of patients before treatment, hearing changes were observed (its decrease, noise, ringing, crackling in the ears, ears congestion). After the therapy of Tagisti, a statistically reliable decrease in the severity of this symptoms was noted. When evaluating the severity of the dizziness, a significant decrease in vertigo intensity was observed. At the end of 4 weeks. Tagisti therapy statistically significantly decreased, the duration of attacks, their severity decreased. Dizziness ceased to bother 27.95% of patients, the rest of his rare attacks were noted. More than half of the patients ceased to complain about the noise in their heads, prefabricated conditions, instability of the gait, nausea. At the time of inclusion in the study, 15 patients suffered from noise (ringing) in the ears. After therapy, only 8 people bothered the noise in the ears, while only 2 patients were strong, the rest of the rest was moderately pronounced. The noise in the head disappeared in 8 patients. Initially, they complained about nausea and vomiting of 6 patients. Tagist's treatment eliminated these concomitant symptoms in all patients by the time the study is completed. By the time the study was completed, the therapeutic effect of varying degrees of severity was observed in 96.88% of patients, including “Very good” therapeutic effect - in 40.6%, “good” - in 50%and “satisfactory” - in 6.28%. In 1 (3.12%) patient, the speaker was not traced. There were no severe side effects and cases of deterioration in the somatic and mental state of patients. In 9.4% of cases (3 patients) in the first days of taking the drug, nausea, discomfort in the epigastric region, and abdominal pain were observed. These complaints did not require additional treatment or cancellation of the drug, they independently stopped for 1st week. During the intake of Tagista, there was no drowsiness and sedative effect, as well as the effect on systemic hemodynamics. The study showed that when using Tagista, the frequency of dizziness attacks was significantly reduced, and a preventive effect was provided. Statistically significant improvement was observed at the end of the 4th week. therapy in the form of a reduction in the frequency of seizures and their severity. The drug also weakens the severity of noise in the head, nausea, vomiting. It is important to note that after the course of treatment, a reliable increase in the stability index was observed (especially in the Romberg pose). The effect of therapy on the severity of ataxia can be both a consequence of an improvement in the state of the vestibular system, and the result of the direct effect of the drug on the system of regulation of postural tone and maintaining balance. Statistically significant positive dynamics in Tagist therapy was accompanied by a minimum number of side effects. Many drugs used for dizziness cause sedentation and depression of the central nervous system. This slows down the compensation process, which is so necessary for the patient's rehabilitation. Tagist, who does not cause oppression of the central nervous system, does not interfere with the compensation process. Moreover, the Tagist accelerates vestibular compensation and allows you to start the process of vestibular rehabilitation as early as possible, which is an integral component of the treatment of patients suffering from dizziness. The drug really has the effect of acceleration to vestibular adaptation, which is vital for the speedy rehabilitation of patients with acute peripheral vestibular disaster. Thus, the Tagist in complex therapy is an effective tool for the treatment of dizziness of various etiologies, which allows us to recommend the use of the drug in everyday neurological practice.
Literature 1. Babiyak V.I., Bazarov V.G., Lantsov A.A. On the problems of vestibular pathology // News of otorhinolaryngology and logopathology. 2000. No. 2 (22). pp. 67–73. 2. Blagoveshchenskaya N.S. Otoneurological symptoms and syndromes. M.: Medicine, 1990. 190 p. 3. Brandt T., Dieterich M., Strupp M. Dizziness (translated from English). Translation editor M.V. Zamergrad. M.: Praktika, 2009. pp. 18–23, 80–120, 140–142. 4. Bradu R.A. et al. Control of symptoms of acute vertigo with betahistine // Breast Cancer 2008. Pain syndrome. pp. 45-50. 5. Veselago O. V. Experience of using Tagista in the treatment of vestibular disorders in chronic cerebrovascular insufficiency // Russian Medical Journal. 2010. No. 26. P. 1546-1548. 6. Zamergrad M.V., Parfenov V.A., Melnikov O.A. Treatment of vestibular vertigo // Journal of Neurology and Psychiatry named after S.S. Korsakov. 2008. v. 108, no. 11. pp. 86–92. 7. Morozova S.V., Ovchinnikov Yu.M., Shtykova N.A. Features of diagnosing vestibular disorders in older people // Bulletin of Otorhinolaryngology. Materials of the Russian Conference of Otorhinolaryngologists. November 18–19, 2003, pp. 173–174. 8. Kostenko E.V., Petrova L.V., Torganova E.A. et al. Experience in the treatment of vestibular vertigo and Meniere's syndrome in an outpatient setting. Treatment of nervous and mental diseases. 9. Tabeeva G.R., Vein A.M. Dizziness in psychovegetative syndromes // Consiliummedicum. 2001. T. 04, No. 15, supplement. 10. Ammar KA, Ane P., Benevant et al. Ishemia of the inner ear. Clinical presentation. The role of an alpha-blocker // Cah.ORL. 1989. Vol. 24. P. 791–798. 11. Eggers SD Migraine-related vertigo: diagnosis and treatment // Curr Pain Headache Rep. 2007. Vol. 11. P. 217–226. 12. Toupet M. Formes cliniques ettraitements des vertiges positionnels paroxys tiques benins. In "Vertiges 97", ouvrage collectif du grouped'etudes des vertiges, Masson, Paris, 1998, pp. 149–172.