Experience of using indole-3-carbinol in the treatment of benign mammary dysplasia
Benign mammary dysplasia is the most common disease among the female population. This pathology affects 30–67% of women of reproductive age, and in women with gynecological diseases, dyshormonal dysplasia occurs in 78–95% of cases [1, 2].
Considering the general pathogenetic basis for the development of benign and malignant diseases of the mammary gland, much attention is paid to the treatment of benign dysplasia as a precancerous disease. The likelihood of malignancy largely depends on the degree of proliferation of breast cells. Thus, with a non-proliferative form of the disease, malignancy occurs in 0.87% of cases, with dysplasia with moderate proliferation - in 2.34%, with severe proliferation - in 31.4% [3].
The main factor that enhances the proliferative activity of mammary gland cells is considered to be an increase in the level of estrogen both in the blood and in the mammary gland tissue itself. Estradiol stimulates differentiation, proliferation and development of the mammary gland ductal epithelium and inhibits apoptosis. In addition, the presence of hormonal imbalance, which manifests itself in the form of relative hypoprogesteronemia, enhances the proliferative effect of estrogens on tissue [2, 4].
Estrogens actively bind to receptors on the membranes of the arcuate nucleus, which causes a decrease in dopamine levels, leading to hyperprolactinemia. In addition, direct stimulation of prolactin secretion by estrogens was detected, activating the expression of the gene responsible for prolactin synthesis. An increase in the level of prolactin entails an increase in the number of estrogen and progesterone receptors, which increases the prolactin-binding ability of alveolar cells of the mammary gland and promotes their proliferation [5].
Estrogen, once inside the cell, activates the estrogen receptor, which facilitates its penetration into the nucleus. Once in the nucleus, this complex stimulates the expression of estrogen-dependent genes. These include vascular endothelial growth factor (VEGF), cyclin-dependent kinase (CDK), insulin-like growth factor (IGF) and other proteins that increase the sensitivity of breast cells to proliferation [5, 6].
Vascular endothelial growth factor stimulates tumor angiogenesis and is a survival factor for immature tumor vessels. In breast cancer, VEGF overexpression is observed in 58% of cases [7, 8].
Estrogens circulating in the bloodstream inevitably pass through the liver, where they are metabolized with the participation of cytochrome P450. Three isoforms of cytochrome P450 are predominantly involved in the metabolism of estrogens - CYP 1A2, CYP 1B1, CYP3A4. The first catalyzes the addition of hydroxyl to the 2-carbon position in the estradiol molecule (E1) and forms a 2-hydroxy derivative (2-OHE1), the second isoform - to position 4 and 4-hydroxy derivative (4-OHE1) and the third isoform to position 16 with the formation of 16- alpha-hydroxy derivative (16-alpha-ONE1). It has been shown that estrone and estradiol represent only 10–15% of the total amount of estrogen derivatives, and 85–90% are estrogen metabolites (mainly hydroxy derivatives) [7]. In addition, estrogen metabolites have greater proliferative activity than estrogen itself. 2-hydroxyestrogens are synthesized with the participation of the enzyme CYP1A1 in the liver and other tissues; they are found in the greatest quantities in breast tissue. These metabolites have a weak estrogenic effect (48% of estradiol activity) and precisely because of this they do not have a proliferative effect on cells. 16-hydroxyestrogens - with the participation of cytochrome 3A4, 16-alpha-ONE1 is formed. The mitogenicity of this metabolite is 8 times higher than that of estradiol, since 16-alpha-ONE1 can covalently and irreversibly bind to endoplasmic reticulum loci, along with binding to nuclear estrogen receptors, which provides stimulation over days rather than hours, while the effect is maintained until the binding proteins are degraded. 4-hydroxyestrone (4-OHE), another estrogen metabolite, like 16-alpha-ONE1, has estrogenic activity (79% of the activity of estradiol). The carcinogenic mutagenic effect of 4-hydroxyestrone can be explained by the influence of its toxic quinol metabolites, the induction of the formation of free superoxide radicals and damage to cell DNA. Thus, an increase in the production of these metabolites is considered as evidence of qualitative changes in steroidogenesis and a factor in the development of some malignant neoplasms [17].
The search for drugs for the treatment of benign mammary dysplasia has led to the development of agents containing indole-3-carbinol, which reduce the proliferative activity of estrogen-dependent cells and have antitumor activity.
Characteristics of indole-3-carbinol-containing dietary supplements
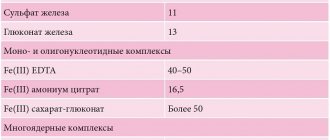
In the treatment of benign mammary dysplasia, we used three biologically active food supplements containing indole-3-carbinol: Stella, Indinol and Estrovel (Table 1).
Stella is available in the form of three-color capsules of 400 mg. The yellow capsule contains 100 mg of indole-3-carbinol, found in cruciferous vegetables. Indole-3-carbinol has the following effects:
1) stimulates the 2-hydroxy estrogen detoxification pathway; 2) modulates estrogen receptors (estrogen receptor alpha antagonist); 3) stimulates apoptosis of cancer cells; 4) inhibits tumor angiogenesis; 5) antioxidant.
The green capsule contains 60 mg of epigallocatechin-3-gallate, found in green tea. Epigallocatechin-3-gallate has the following effects:
1) reduces the production of the aromatase enzyme, which promotes the conversion of androgens into estrogens; 2) selectively reduces the rate of vascular growth in neoplasms, that is, it suppresses the production of vascular endothelial growth factor (VEGF).
The red capsule contains 60 mg of soy isoflavones (genistein and dzadzein), which have the following effects:
1) stimulate 2-hydroxylation of estrogens; 2) competitively bind to estrogen receptors; 3) reduce the secretion of 4-hydroxy estrogens; 4) increase the production of sex-binding globulin.
It is recommended to take Stella to normalize estrogen metabolism (restoring the normal ratio of 2-hydroxyestrogen and 16-alpha-hydroxyestrogen and reducing the production of 4-hydroxyestrogens), to improve the functional state of the female reproductive system and reduce the risk of hormone-dependent diseases of the female reproductive system, such as fibroids, mastopathy , endometriosis and as part of complex therapy of the latter. Recommended doses: 1 yellow capsule in the morning, 1 green capsule in the afternoon and 1 red capsule in the evening - for 1 month. If necessary, treatment can be extended to 3–6 months, 1–2 times a year at regular intervals [18].
Indinol is available in 300 mg capsules. Each capsule contains 90 mg of indole-3-carbinol and excipients, including magnesium stearate 3 mg.
Indinol should be taken for prevention and as part of complex treatment of benign diseases of the mammary glands. It is also recommended to take Indinol when benign mammary dysplasia is combined with other diseases of the female reproductive system: endometriosis, uterine fibroids, endometrial hyperplasia, cervical dysplasia, genital condylomatosis.
Estrovel is available in 500 mg tablets. It contains indole-3-carbinol (25 mg per tablet), cohosh racemosa extract (30 mg per tablet), wild yam root extract (50 mg), soy isoflavones (25 mg), vitamins B6, E, folic acid and other auxiliary components in small quantities.
Cosimifuga racemosa and wild yam root have been used since ancient times to treat menopausal disorders in women. Soy isoflavones are phytoestrogens and compensate for the negative effects of estrogen when it is in excess. Therefore, in addition to the therapeutic effect on breast tissue, Estrovel helps to normalize unstable blood pressure, reduces the intensity of headache attacks, and reduces the frequency of hot flashes in women with neurovegetative disorders during menopause. The recommended dose of Estrovel is 1-2 tablets per day for 2 months.
In many Russian cities there are no large mammology centers. Identification, clinical observation and treatment of patients with dishormonal dysplasia of the mammary gland is carried out by local obstetricians-gynecologists. In turn, an analysis of outpatient records of a dispensary group of patients showed that treatment of diseases of the mammary glands is not always carried out adequately to their objective condition, changes in ultrasound and mammography, and the presence of concomitant gynecological pathology. Therefore, research into the use of indole-3-carbinol-containing dietary supplements will help more rational treatment of women with diseases of the mammary glands.
Purpose of the study: to analyze the effectiveness of treatment of women of different age groups with dyshormonal dysplasia of the mammary glands with indole-3-carbinol-containing dietary supplements.
Patients and methods. A total of 192 women registered with a mammologist with a diagnosis of benign dishormonal dysplasia of the mammary glands were treated with indole-3-carbinol-containing dietary supplements (as part of complex therapy). The age of the patients ranged from 17 to 56 years. The duration of observation by a mammologist ranged from 1 to 19 years. All patients underwent ultrasound examination of the mammary glands. Women 40 years and older - ultrasound examination and mammography.
Group 1 included 52 women aged 17 to 35 years. The group accepted Stella for 3 months.
Group 2 consisted of 103 patients aged 17 to 50 years who received Indinol. There were 48 patients of reproductive age, 55 patients of premenopausal and menopausal age.
Group 3 included 37 women aged 50 to 56 years who were treated with Estrovel.
Evaluation of the results of therapy included an analysis of the intensity of pain in the mammary glands, the state of the structure of the breast tissue during examination and palpation, and changes in the breast tissue during an ultrasound examination.
Pain intensity was assessed using a verbal scale ranging from 0 to 4:
- 0 points - no pain;
- 1 point – mild pain;
- 2 points - moderate pain;
- 3 points - severe pain;
- 4 points - unbearable pain.
The condition of the breast tissue was assessed based on examination and palpation in scores from 0 to 6 [11]:
- 0 points – absence of pathological process;
- 1 point - mild diffuse fibroadenomatosis;
- 2 points - moderately severe diffuse fibroadenomatosis;
- 3 points—severe diffuse cystic or fibrous fibroadenomatosis;
- 4 points - pronounced diffuse cystic or fibrous fibroadenomatosis;
- 5 points - localized fibroadenomatosis against a diffuse background;
- 6 points - localized fibroadenomatosis against a background of diffuse fibroadenomatosis.
The results obtained and their discussion
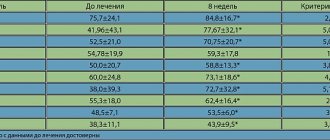
Group 1 included women of reproductive age. All patients complained of severe pain in the mammary glands before menstruation for 7–10 days (78%) or moderate pain not associated with the cycle (22%). During examination, lump-like compactions in the mammary glands were more common - 5 points (63%) and medium-grained compactions - 4 points (37%). In 80% of cases, upon examination, the breast tissue is dense and swollen. During an ultrasound examination, the picture in all women corresponded to a mixed (fibrocystic) form of mastopathy. The maximum size of cysts is 14.5 mm.
Women of the 1st group were prescribed Stella capsules, 1 pc. 3 times a day for 1 month (according to the instructions and voluntary certification, translated into indole-3-carbinol 100 mg). This treatment was carried out as part of complex therapy, which included vitamins and microelements. For severe pain, Mastofit Evalar cream was used topically 2 times a day, 7–10 days a month.
All women tolerated the treatment well. Many noted the modern color design of the tablets, which increased the motivation of patients for consistent treatment. Improvement occurred in 72% of women. Pain in the mammary glands, both premenstrual and not associated with the cycle, decreased to mild, although the pain syndrome was not completely relieved. 26% of patients did not note any significant improvement in their condition. And 1 patient (2%) after treatment complained of increased pain in the mammary glands before menstruation.
Upon examination, an improvement in the condition of the mammary glands was noted in 86% of women. The breast tissue has become softer and more uniform (3–4 points). Lump-like seals persisted in 27% of patients. During control ultrasound, no significant changes were noted: tissue fibrosis remained, the size of the cysts did not decrease. Patients are recommended to continue the course for up to 3–6 months.
All women of group 2 complained of pain in the mammary glands. Women of reproductive age were bothered by pain before menstruation 10–14 days in advance. The patient's pain intensity was characterized as moderate (40%) and severe (60%). On examination, the structure of the mammary glands is dense-grained, heterogeneous, which corresponded to 3–4 points (56%) and 5 points (44%). On ultrasound, women of reproductive age have fibrous changes and cysts from 0.7 to 1.2 cm. In women of pre- and menopausal age, ultrasound and mammography examinations revealed a fibrocystic or fibrous form of mastopathy with symptoms of fatty involution.
When prescribing Indinol, adjustments were made to the dose and duration of treatment. In the instructions included with the package, the recommended dose is 1 capsule per day for 2-3 weeks. But in the literature devoted to the treatment of breast diseases, the doses used range from 2 to 4 capsules per day with a duration of administration from 1 to 6 months [9, 12–14]. There is evidence of the dependence of the doses used on the patient’s weight. Thus, women up to 60 kg need to take 1 capsule 3 times a day, and women over 60 kg need 2 capsules 2 times a day [14]. But such an increase in the dose and duration of administration requires additional financial costs, which limits the range of patients to whom treatment can be prescribed.
We decided to go with an average dose - 300 mg (1 capsule) 2 times a day (translated into indole-3-carbinol 180 mg). In case of severe pain, Mastofit Evalar cream was additionally prescribed topically to the mammary glands 2 times a day 7–10 days before menstruation.
All patients completed a three-month course of treatment. No allergic reactions or adverse symptoms were observed. In 61% of women of reproductive age, premenstrual pain syndrome significantly decreased to mild pain 3-5 days before menstruation. 52% of women of pre- and menopausal age noted both a decrease or disappearance of pain and a decrease in sensations in the mammary glands such as burning, tingling, and itching.
When examining the mammary glands, a softer and more homogeneous tissue structure (2–3 points) was noted in 83% of women of reproductive age and 64% of women of pre- and menopausal age. The control ultrasound did not reveal any visible positive changes in women of either age group: cysts of the same size, fibrosis in the same volume.
According to the literature, the maximum effect in the treatment of patients is observed by the 6th month. The disappearance of mastalgia and mastodynia is observed in 70.4–90.5% of patients [12–14]. Moreover, 100% effectiveness of treatment was noted in patients with glandular mastopathy [15]. An improvement in the mammographic picture in 33.7% of patients is observed by the 12th month after treatment [16]. Therefore, women in this group were recommended to continue treatment with Indinol.
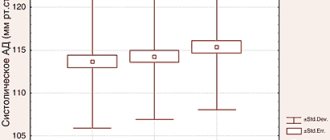
Women of the 3rd group complained of severe (35%) and moderate (65%) pain in the mammary glands and symptoms characteristic of menopausal syndrome: hot flashes, fever, palpitations, sweating. Patients were prescribed Estrovel 1 tablet 2 times a day for 3 months (according to the instructions and voluntary certification, translated into indole-3-carbinol 50 mg). For severe pain in the mammary glands, Mastofit Evalar cream was used topically 2 times a day 7–10 days before menstruation.
Upon examination, the mammary glands had a fine- or medium-grained structure and a dense consistency (2–3 points). Ultrasound reveals fibrous changes in breast tissue against the background of involution. Mammograms showed a similar picture.
The available literature on the use of Estrovel in women during perimenopause shows good tolerability and 100% effectiveness against neurovegetative symptoms [17].
During the treatment of our 37 women, one patient experienced an exacerbation of chronic cholecystopancreatitis. Estrovel had to be cancelled. The remaining 36 women tolerated the treatment well. After three months of therapy, 68% of patients noted an improvement in their health: pain and discomfort in the mammary glands decreased. Severe pain bothered only 8% of patients. Neurovegetative symptoms became less pronounced in 68% of women, and 32% noted the disappearance of hot flashes and fever. Upon examination, the mammary glands became softer and more uniform (1–2 points) in 62% of women (Table 2). But the control ultrasound did not reveal any obvious positive dynamics.
conclusions
- Indole-3-carbinol-containing dietary supplements are highly effective in the complex treatment of patients with benign dishormonal dysplasia of the mammary glands.
- Treatment with indole-3-carbinol-containing dietary supplements is well tolerated by women of reproductive, premenopausal and menopausal age.
- An improvement in the subjective state in the form of a decrease in the intensity and duration of pain in the mammary glands was noted in 61–78% of women of reproductive age and 52–68% of women of pre- and menopausal age. Improvement in objective indicators in the form of improvement in the structure of breast tissue was noted in 83–86% of women of reproductive age and 62–64% of women of pre- and menopausal age.
- To achieve maximum effectiveness from therapy and positive dynamics of the objective condition of the mammary gland according to ultrasound and mammography, it is necessary to continue treatment (as part of complex therapy) with indole-3-carbinol-containing dietary supplements for up to 6 months.
Literature
- Letyagin V.P., Vysotskaya I.V., Kim E.A. Pogodina E.M., Maksimov K.V. Herbal medicine for diffuse fibrocystic disease. M.: ABV-press, 2008. 28 p.
- Mustafin Ch. K., Kuznetsova S. V. Dyshormonal diseases of the mammary gland. Clinical manual / Ed. Pinkhosevich E. G. M., 2009. 126 p.
- Vasilevsky A.V., Kozlovskaya N.A., Ilkevich A.G. et al. Benign and malignant diseases of the breast: A manual for students and doctors. Ed. L. A. Putyrsky, Yu. L. Putyrsky. M.: LLC "Med. information agency", 2008. 336 p.
- Chistyakov S. S., Selchuk V. Yu., Grebennikova O. P. et al. Cancer and benign tumors of the breast: A textbook for the system of postgraduate professional education. Ed. S. S. Chistyakova. M.: Author's Academy, 2009. 120 p.
- Gilyazutdinov I. A., Khaskhanov R. Sh. Benign tumors of the mammary glands: A guide for doctors. Kazan: Medical literature, 2007. 216 p.
- Vysotskaya I.V. Modern possibilities for the treatment of fibrocystic disease // Tumors of the female reproductive system. 2009. No. 1–2. pp. 44–46.
- Vozny E.K., Belonogov A.V., Satirov E.F., Yurgina O.V. Breast cancer (modern approaches). Clinical mammology. Thematic collection. 1st edition. M.: LLC Firma Strom", 2005. 181–189.
- Speirs V., Atkin SL Production of VGEF and expression of the VEGF receptors Ade-1 and KDR in primary cultures of epithlial and stromal cells derived from breast tumors // Br J Cancer. 1999. No. 80 (5–6). 898–903.
- Kiselev I.V., Lyashenko A.A. Indinol is a regulator of proliferative processes in the organs of the reproductive system. M.: ZAO MiraxPharma, 2008. 48 p.
- Sidorenko L. N. Mammary gland. How to protect yourself from cancer. A book for every woman. SPb: Folio-Press. 1998. 704 p.
- Rakhimzhanova R.I., Suleimenova E.V., Mayer K.M., Solomonova A.M. Experience of using indinol in the treatment of various forms of mastopathy in Kazakhstan. Organizational, medical and technical aspects of clinical mammology. Mater. 5 All-Russian scientific-practical conf. with international participation. M., 2007. 130–132.
- Rozhkova N.I., Meskikh E.V. Evaluation of the effectiveness of the drug indinol in the treatment of various forms of mastopathy. Organizational, medical and technical aspects of clinical mammology. Mater. 5 All-Russian scientific-practical conf. with international participation. M., 2007. 149–152.
- Rozhkova N. I., Burdina L. M., Smetnik V. P. et al. Complex allopathic and homeopathic treatment of mastopathy // Bulletin of the Russian Association of Radiologists. 2009. No. 1. 148–152.
- Zulkarnaeva E. T., Khakimova R. Kh., Lapan E. I., Blagodetev I. L. Indinol-3-carbinol in the treatment of benign breast diseases // Tumors of the female reproductive system. 2008. No. 3. P. 50–54.
- Kulagina N.V. Therapy of fibrocystic disease of the mammary glands in patients with uterine fibroids // Tumors of the female reproductive system. 2010. No. 1. P. 40–43.
- Kulchavenya E.V., Brizhatyuk E.V., Breusov A.A. The effectiveness of the dietary supplement estrovel in the complex therapy of women with chronic cystitis during perimenopause // Obstetrics and Gynecology. 2009. No. 3. P. 69–71.
- Bradlow HL, Telang NT, Sepkowic DW et al. // J Endocrinol. 1996; 150: 259–265.
- Information letter from ROAG. M., 2009.
E. A. Sukhareva*, Candidate of Medical Sciences L. A. Ponomareva**, Doctor of Medical Sciences, Professor S. V. Kozlov**, Doctor of Medical Sciences, Professor
*MUZ City Clinic No. 1, Syzran ** State Budgetary Educational Institution of Higher Professional Education SSMU named after. V. I. Razumovsky Ministry of Health and Social Development of Russia, Samara
Contact information for authors for correspondence
In recent years, there has been increasing interest throughout the world in the health and quality of life of women, as the steady trend towards an increase in the number of diseases of the female reproductive system, including the breast, continues [10]. Thus, in the population, non-cancerous diseases of the mammary glands occur in 30-70% of women, and when they are simultaneously combined with gynecological diseases, the number of cases increases to 76-97.8% [10].
In Russia, more than 34,000 new cases of breast cancer are detected annually, and a significant decrease in the age of those affected is noted. In 25% of women under 30 years of age and in 60% after 40 years of age, dyshormonal diseases of the mammary glands (mastopathy) are diagnosed [6]. Despite the fact that mastopathy is not an obligate precancer, breast cancer occurs 3-5 times more often against the background of diffuse dishormonal benign diseases of the mammary glands and 30-40 times more often in nodular forms of mastopathy with phenomena of proliferation of their epithelium [6]. In general, obstetrician-gynecologists do not deal with breast cancer, but women often turn to them with problems that are not directly related to the content of the specialty, including problems related to the mammary glands. Therefore, obstetricians-gynecologists can significantly improve the quality of work to preserve the health of women with extragenital pathology and with some forms of cancer, in particular with breast cancer. Undoubtedly, the priorities for gynecologists are the diagnosis and treatment of benign diseases of the mammary glands. Identification of diffuse and focal pathology of the mammary glands and correct interpretation of the examination results make it possible to promptly refer women to a comprehensive examination and navigate the correct choice of treatment method.
More than 100 years have passed since the morphological picture of mastopathy was described, but there are still more questions related to this disease than answers. If the possibility of malignancy in pronounced proliferative forms of fibrocystic disease in 30% of cases is obvious, then the issues of etiology and pathogenesis of the disease remain largely unclear. If it is recognized that an important role in the pathogenesis is assigned to absolute or relative hyperestrogenism and progesterone deficiency, then the motives for the development of severe forms of the disease in women with a regular two-phase cycle and a full luteal phase are unclear [9]. The interdependence of diseases of the mammary glands and internal genital organs and their impact on reproductive health in general has been established. At the same time, clinical and epidemiological data indicate a pathogenetic connection between fibroadenosis of the mammary glands and dyshormonal changes in the body, gynecological diseases, defective development of generative and sexual dysfunction [9].
Despite the numerous studies available, currently the etiology of mastopathy remains unclear. The variety of forms of dysplastic processes and benign breast tumors, which have different histo- and morphogenesis, indicates the polyetiology of their occurrence. Also, no specific risk factor for the development of this disease has been identified, since mastopathy is a multifactorial disease associated with both genetic and environmental factors.
The lack of a clear opinion on the etiology and pathogenesis of dishormonal diseases of the mammary glands also determines the lack of a clear algorithm for the treatment of fibrocystic mastopathy. Each case requires an individual approach. The main links in the pathogenesis of benign breast diseases are hormonal imbalances, activation of cell proliferation signaling pathways associated with the expression of growth factors and neoangiogenesis, as well as suppression of apoptosis. In this regard, the search for treatment methods that affect the mechanisms of development of the pathological process remains relevant.
The modern approach to the treatment of diffuse forms of mastopathy involves the use of hormonal and non-hormonal methods. Most often, hormonal therapy is aimed at reducing the excessive stimulating effect of estrogens on breast tissue, and less often at correcting dysprolactinemia or hypothyroidism. Among the hormonal methods of treatment, it is known to prescribe antiestrogenic drugs (tamoxifen, toremifene), combined oral contraceptives, gestagens (progestogel-gel, utrozhestan), androgens (danazol), luteinizing hormone releasing factor analogues (zoladex, buserelin), prolactin secretion inhibitors (bromocriptine, dostinex). However, despite the clinical effect of hormonal therapy, its long-term use is limited due to the risk of developing known side effects. An exception is the use of combined oral contraceptives, the undoubted role and effectiveness of which in the treatment of dishormonal pathology of the mammary glands has been proven [7, 12, 13, 18]. But, along with this, the results of numerous studies do not give a clear answer about the harm or benefit of these drugs, bearing in mind the risk of developing benign and malignant breast diseases. And this contributes to some fear both on the part of patients and on the part of doctors of general use of oral contraceptives for the treatment of breast diseases. When analyzing the risk-benefit factor for the patient, the choice will not be in the direction of hormonal therapy.
Among the non-hormonal methods of treating diffuse dishormonal diseases of the mammary glands, the following are distinguished: diet correction, vitamin therapy, the use of non-steroidal anti-inflammatory drugs that improve blood circulation, the prescription of diuretics, sedatives and complex natural products.
The use of non-hormonal methods for the treatment of dishormonal diseases of the mammary glands is widely discussed and very controversial. If it is impossible to carry out more effective treatment in the presence of symptoms of mastopathy, the use of herbal remedies is appropriate and justified. Chairman of the Board Prof. Michael Popp said about natural products: “We combine the best of what man is now capable of with the best of what nature has to offer us.” Herbal medicines are widely used in Russian clinical practice. Prof. dedicated her speech to their role in the treatment of breast diseases. N.I. Rozhkova, head of the Federal Breast Center, President of the Russian Association of Mammologists: “The priority areas today are screening, early diagnosis and prevention. And here the correct choice of drugs for the treatment of mastopathy and premenstrual syndrome is very important in order to prevent the development of more severe diseases. Herbal medicines are ideal for these purposes. The center’s specialists came to this conclusion based on their own research.”
Over the past 10 years, at the Department of Obstetrics and Gynecology of the Yaroslavl State Medical Academy, studies have been conducted to study the effect of hormonal drugs (combined oral contraceptives, hormone replacement therapy, progesterone) and the combined homeopathic drug mastodynon on the condition of the mammary glands in various diagnosed forms of mastopathy [7, 11-13, 18]. In recent years, indinol, a drug produced by the ILMIX GROUP, has attracted attention. The interest is primarily due to the mechanism of action of the drug described in the literature. The main pharmacological effects of indinol include the following:
- normalization of the metabolism of the female sex hormone - estradiol;
— inhibition of the synthesis of 16-hydroxyestrone, which has pronounced carcinogenic properties;
- reduction in the number of estrogen receptors in target tissues.
The effect of the drug is due to the content of highly purified indole-3-carbinol, which normalizes the metabolism of estrogen in the body and prevents the development of estrogen-dependent diseases through the following mechanisms:
— normalization of estrogen metabolism by inducing the activity of cytochrome CYP1A1, responsible for the predominant formation of 2-hydroxyestrone;
— inhibition of pathological cell proliferation by blocking intracellular signaling pathways coming from growth factors (EGF, IGF) and cytokines (tumor necrosis factor-alpha, interleukin-1);
— induction of apoptosis in tumor and tumor-like cells through the Bax-Bcl system.
All of the above suggests that indinol can be used as a pathogenetic agent in the treatment of mastopathy.
The purpose of this study is to identify changes in the mammary glands in diagnosed various forms of mastopathy that occur during the use of indinol.
Material and methods
The study involved 178 female volunteers from 19 to 50 years old with diagnosed various forms of mastopathy, who were prescribed indinol as a therapeutic drug, 2 capsules 2 times a day for 3 months. The women examined were grouped into four age groups. The groups were formed taking into account data on the morphofunctional periods of age-related restructuring of the mammary gland: group 1 (up to 34 years) - mastopathy with a predominance of the glandular component; 2nd (35-40 years) - gradual loss of glandular structures; 3rd (41-44 years) - thickening of the columnar epithelium of the ducts, thickening of the basement membrane and fibrous restructuring of the connective tissue; 4th (45-50 years) - dilatation, and sometimes cystic expansion of the milk ducts, compressed by fibrous tissue. After 51 years of age, slow obliteration of the milk ducts, as well as small vessels and the formation of adipose tissue are observed [2, 14]. The distribution of the number of observations of various forms of mastopathy in different age groups is presented in Table. 1.
The following diagnostic methods were used.
— Clinical and anamnestic, including medical history, examination and palpation of the mammary glands. When collecting anamnesis, special attention was paid to information about pain symptoms and engorgement of the mammary glands. Pain and engorgement were proposed to be assessed on a 5-point conditional scale, in which the maximum pain and engorgement were assessed as five points, less pronounced - 4, 3, 2 points, 1 point, and the absence of pain and engorgement - 0 points.
— Ultrasound examination of the mammary glands was carried out from the 5th to the 9th day of the menstrual cycle on a Combison 530 ultrasound machine using a 7.5 MHz electronic linear sensor according to standard methods.
— X-ray mammography was carried out from the 5th to the 9th day of the menstrual cycle on the X-ray machine Mammodiagnost UC. We used ACFA Mammorei HDR film and Kodak min-R cassette.
— To visualize breast tissue, electrical impedance mammography was used using a multifrequency 256-electrode electrical impedance mammograph (MEM), developed by the Institute of Radio Engineering and Electronics of the Russian Academy of Sciences, at frequencies of 10 and 50 kHz [3-5, 15-17]. The software was provided by Senior Researcher IRE RAS, Ph.D. physics and mathematics Sciences V.N. Kornienko and the head of the electromagnetic tomography group of the IRE RAS, Ph.D. physics and mathematics Sciences, senior researcher A.V. Korzhenevsky.
In order to implement the electrical impedance mammography method, a measuring system and an image reconstruction algorithm have been developed that allow, using a set of 256 electrodes located in the form of a two-dimensional matrix on a flat surface, to visualize the static distributions of electrical conductivity of the medium adjacent to the surface with the electrodes. Current flowing through breast tissue creates a volumetric distribution of electrical potential. The potential decreases along the current line as it moves away from the current-injecting electrode. The voltage drop per unit length is proportional to the magnitude of the current I and the resistance of the medium ΔR in accordance with Ohm's law. By measuring the voltage drop ΔV and knowing the current value, you can calculate the resistance value. During the examination, the matrix was pressed against the mammary gland in the direction of the ribs, and two output electrodes, one of which was used as a common electrode of the current source, and the second as a reference electrode for a potential difference meter, were docked together and located on the patient’s wrist (Fig. 1 ).
Figure 1. Technique for performing electrical impedance mammography.
The potential difference meter was connected by a multiplexer to the first electrode of the matrix, and then the current source was sequentially connected to each of the remaining electrodes of the matrix and measurements were made (at a frequency of 50 kHz, the current was 0.5 mA, at a frequency of 10 kHz - 0.13 mA). After this, the cycle was repeated for another recording electrode. The complete data set used to obtain the image consisted of 65,280 measurements. The material was processed using a personal computer connected to the device via a standard USB port. The result of the reconstruction was electrical impedance images of seven cross sections of the medium under study, parallel to the plane with the electrodes, taken with a step of 0.7 cm in depth.
— A puncture biopsy was performed with a special puncture needle according to standard methods after the results of ultrasound and X-ray examinations.
— If there was discharge from the nipples, a cytological examination of the discharge was performed.
— Statistical processing of the results obtained was carried out using the methods of variation statistics using sampling testing for compliance with the laws of normal probability distribution of a sign in the compared groups and equality of general variances. In the presence of a normal distribution, the significance of differences was assessed using Student's t-test. The probability of p=0.05 was used as a confidence level. Statistical processing was carried out on a Pentium-4 personal computer using data analysis systems Microsoft Excel and Statistica for Windows. Version 6.0. The mean (M) and standard deviation (SD) were calculated [1, 8].
To confirm the diagnosis, verify various forms of mastopathy and exclude breast cancer, all 178 women underwent examination of the mammary glands using clinical history, ultrasound and electrical impedance methods before prescribing the drug. X-ray mammography was performed in 135 women 35 years of age and older. A puncture biopsy was performed in 47 women of different age groups in the presence of cysts larger than 10 mm in diameter. A cytological study was carried out on 41 women of different age groups with nipple discharge. No atypical cells were detected in any observation.
3 months after starting to take indinol, all women underwent examination of the mammary glands using clinical history, ultrasound, and electrical impedance methods. Two patients underwent puncture biopsy of cysts with a diameter greater than 10 mm. Cytological examination of nipple discharge was performed in 23 women of different age groups. Similar to the first study, no atypical cells were found. X-ray mammography was not used as a method for comparing results due to the short time period for repeated examination.
The data presented in modern literature about changes in the mammary glands during the use of any drugs are based on an assessment of patient complaints regarding pain symptoms, ultrasound data, x-ray mammography, cytological examination of discharge from the nipples or punctate in the presence of focal symptoms. The value of each of the listed diagnostic methods is undoubted and has been proven many times, but for dynamic monitoring of the condition of the mammary glands, the method of electrical impedance mammography has an advantage. This is due to the real possibility of detecting minimal changes in the mammary glands using this method and its ability to provide not only a visual, but also a quantitative objective assessment of the condition of the mammary glands. Therefore, in our study, all generally accepted methods were of secondary importance, and the main place in detecting changes in the mammary glands while taking indinol was occupied by the method of electrical impedance mammography.
Results and discussion
Data on the comparative assessment of pain symptoms and engorgement of the mammary glands in women with different types of mastopathy on a 5-point scale before taking indinol and 3 months after starting its use are presented in Fig. 2, 3, 4, 5.
Figure 2. Comparative assessment of pain symptoms and engorgement of the mammary glands before taking indinol and 3 months after starting it in women with glandular type of mastopathy.
Figure 3. Comparative assessment of pain symptoms and engorgement of the mammary glands before taking indinol and 3 months after starting it in women with cystic type of mastopathy.
Figure 4. Comparative assessment of pain symptoms and engorgement of the mammary glands before taking indinol and 3 months after starting it in women with fibrous type of mastopathy.
Figure 5. Comparative assessment of pain and engorgement of the mammary glands before taking indinol and 3 months after starting it in women with mixed type of mastopathy.
As the figures show, before taking indinol, the pain symptom and engorgement of the mammary glands were most pronounced in women with the glandular form of mastopathy (5 points - in 12.2%, 4 points - in 36.6%) and with a mixed type of mastopathy (5 points - 5%, 4 points - 35%). Painful sensations of moderate severity were more common in women with fibrous form of mastopathy (3 points - in 20%, 2 points - in 51.2%), cystic form of mastopathy (3 points - in 34.4%, 2 points - in 40, 6%) and mixed type (3 points - in 35%, 2 points - in 6.7%). Lack of pain and engorgement were uncommon in mastopathy and averaged from 0 to 8%.
After using indinol for 3 months, the number of women with lower scores for pain symptoms and engorgement of the mammary glands in all types of mastopathy increased. The most significant reduction in pain was observed in the fibrous form of mastopathy (1 point - 53.3%, 0 points - 35.6%) and in its glandular form (1 point - 46.3%, 0 points - 36.6%). To a lesser extent - with the cystic form of mastopathy (1 point - 40.6%, 0 points - 12.5%) and with the mixed type (1 point - 26.7%, 0 points - 13.3%).
When analyzing the data obtained, a decrease in pain and engorgement of the mammary glands when taking indinol or their complete disappearance is clearly visible, which, undoubtedly, cannot but improve the quality of life of a woman.
The assessment of pain and engorgement of the mammary glands cannot be devoid of an element of subjectivity, bias and, in addition, depends on the threshold of pain sensitivity, which varies among different patients. Therefore, it is more important to assess the effectiveness of the drug by assessing the objective symptoms of mastopathy. When conducting an ultrasound examination of the mammary glands, the thickness of the parenchyma, the average diameter of the maximally dilated ducts and the diameter of mammary gland cysts less than 10 mm were taken into account. Cysts larger than 10 mm were punctured and were not included in the comparative assessment. Other ultrasound signs of mastopathy - the degree of tissue echo density and the severity of fibrosis, in our opinion, are subjective and cannot be accurately assessed during dynamic observation. The results of dynamic monitoring of the condition of the mammary glands when taking indinol are presented in table. 2.
When conducting a comparative analysis of ultrasound signs of mastopathy before taking indinol and 3 months after its start, a tendency to a decrease in the diameter of the ducts was revealed, especially in glandular and mixed forms of mastopathy, as well as a tendency to a decrease in the diameter of mammary gland cysts. But the difference in all cases was statistically insignificant (p>0.05). However, positive dynamics in relation to ultrasound symptoms of mastopathy during dynamic observation cannot but indicate the beneficial effect of indinol, especially in glandular and mixed forms of mastopathy.
When examining the mammary glands using electrical impedance mammography and conducting a comparative analysis during dynamic observation, we used previously developed and presented in the scientific literature data on electrical conductivity in normal conditions and in various types of mastopathy [13]. Electrical conductivity is expressed in conventional units (arbitrary units).
According to the studies, during dynamic observation 3 months after the start of taking indinol, no visual changes were detected on electrical impedance mammograms. In all cases, before taking the drug and 3 months after its start, the following was observed: clear, undeformed contours of the mammary gland; no displacement of internal structures; violation of the architectonics of images due to changes in the ratio of breast tissue and, as a consequence of this, a discrepancy between the type of electrical impedance image (juvenile, reproductive, premenopausal, postmenopausal) and age; an increase in hyperimpedance areas due to fibrotic changes in adipose tissue, fibrosis of the walls of the ducts and Cooper’s ligaments; an increase in zones of average electrical conductivity due to hyperplasia of glandular tissue with adenoses; the appearance on mammograms of hypoimpedance inclusions with clear contours, corresponding to mammary gland cysts or pronounced pocket-like dilatation of the ducts. Given the absence of visual changes during dynamic observation, as well as to eliminate the subjectivity of the assessment, this study focused on the quantitative analysis of electrical impedance images.
Analysis of the results of a quantitative assessment of electrical impedance images in women taking indinol was carried out before starting the drug and 3 months after the start of treatment from the 2nd scanning level, since the patterns of changes in electrical conductivity at all levels are the same [13]. The results are presented in table. 3.
When analyzing the results obtained, a clear statistically significant increase in the electrical conductivity of the mammary glands was revealed when scanning at a frequency of 50 kHz after 3 months of using indinol in women of all age groups with mastopathy with a predominance of the glandular component and with a predominance of the fibrous component (p<0.01, p<0 .05). In mastopathy with a predominance of the cystic component and the mixed form, a statistically significant increase in electrical conductivity parameters when scanning at a frequency of 50 kHz was observed only in age groups under 40 years (p<0.01, p<0.05). After 40 years, despite the trend towards an increase in electrical conductivity in these groups, the difference was statistically insignificant (p>0.05). When scanning at a frequency of 10 kHz, which allows us to detect swelling of the breast tissue, there was no statistically significant deviation of electrical conductivity parameters from the initial values in any age group for all types of mastopathy (p>0.05).
The results obtained made it possible to establish that the mammary glands of women of different age groups and with different forms of mastopathy react to taking indinol in different ways.
It is known that at different stages of the involutive process the ratio of glandular tissue, connective tissue and fatty components in the structure of the mammary gland changes, the thickness of the columnar epithelium, the lumen of the ducts and the state of the receptor apparatus change. With mastopathy, these processes do not correspond to age-related changes, but rather precede them and are more pronounced. All this, apparently, causes a different response of the mammary glands to treatment with indinol at different age periods and with different forms of mastopathy.
With the most preserved glandular tissue, the therapeutic effect of the use of indinol is more pronounced and significant, as evidenced by the increasing electrical conductivity values in all women under 40 years of age with all types of mastopathy. And an increase in electrical conductivity in all cases at a scanning frequency of 50 kHz indicates inhibition and a decrease in proliferative processes, which are always accompanied by a decrease in electrical conductivity. This undoubtedly proves that when treated with indinol, pathological cell proliferation is inhibited and, due to this, the symptoms of mastopathy are reduced.
In women aged 41 years and older, when thickening of the columnar epithelium of the ducts, thickening of the basement membrane, fibrous restructuring of the connective tissue and dilatation of the milk ducts compressed by fibrous tissue are observed, and the amount of glandular tissue decreases, the effect of indinol is not so pronounced. This is confirmed by the absence of a statistically significant increase in electrical conductivity at a scanning frequency of 50 kHz.
Naturally, there is a significant increase in electrical conductivity indicators at a scanning frequency of 50 kHz in women of all age groups with a fibrotic form of mastopathy, in which, while taking indinol, the phenomena of proliferation and fibrosis are reduced and, accordingly, the pharmacological effect of the drug is more pronounced.
conclusions
1. Indinol is a safe remedy for the treatment of mastopathy of all forms in women of any age group, since not a single side effect or negative dynamics in the course of mastopathy was identified while taking the drug.
2. The most pronounced effect when using indinol was achieved in mastopathy with a predominance of glandular and fibrous components in any age period, as well as in mastopathy with a predominance of the cystic component and its mixed type - in women under 40 years of age.
3. Along with the symptomatic effect (reduction and cessation of pain and engorgement of the mammary glands), the pathogenetic effect of the drug is also observed (reduction in the proliferation of mammary gland tissue, as evidenced by an increase in electrical conductivity indicators during dynamic observation).
4. If it is impossible to treat mastopathy with hormonal drugs, it is recommended to use indinol, which can significantly reduce the severity of the clinical symptoms of mastopathy and improve the quality of life.
5. The electrical impedance mammography method makes it possible to identify minimal deviations in the structure of the mammary glands, which is inaccessible to other diagnostic methods and therefore can serve as a reliable method for monitoring the treatment during dynamic observation.
Biologically active food supplement “Indinol” (capsules 300 mg) No. 60
Product description
Dietary supplement Not a medicine.
Dosage form
Capsules.
Purpose
For women.
Compound
1 capsule contains 90 mg indole-3-carbinol.
pharmachologic effect
Indinol is a biologically active food supplement that is a universal hyperplastic corrector of pathological processes in the organs and tissues of the female reproductive system (breast, endometrium, myometrium, cervix, ovaries). Normalizes the balance of estrogen in the body and suppresses their negative stimulating effect, and also blocks other (hormone-independent) mechanisms that activate pathological cellular growth in the tissues of the mammary gland and uterus. It has the ability to cause selective death of transformed cells with abnormally high proliferative activity.
Indications
Indinol is recommended as a dietary supplement to food - an additional source of indole-3-carbinol. It is recommended to use: for the prevention of fibrocystic mastopathy and as part of its complex treatment, as well as for the correction of the functional states of the mammary glands caused by this pathology; in combination with the dietary supplement Epigallat in the complex therapeutic treatment of endometriosis, adenomyosis, uterine fibroids and endometrial hyperplasia without atypia, as well as for the prevention of relapse of these diseases after surgical treatment; in the complex treatment of genital diseases in women associated with the human papillomavirus: cervical dysplasia (cervical intraepithelial neoplasia), anogenital condylomatosis.
Contraindications
Individual intolerance to the components of the drug. Not recommended for people taking medications that reduce gastric acidity, as well as for pregnant and lactating women. Consult your healthcare practitioner before use.
How to take, course of administration and dosage
For fibrocystic mastopathy, Indinol is recommended to be taken orally, 1 capsule per day with meals for 2-3 weeks. As part of combination therapy (endometrial hyperplasia without atypia, endometriosis, adenomyosis, uterine fibroids), Indinol is recommended to be taken orally in combination with the dietary supplement Epigallat (1 capsule + 1 capsule) with meals for 2-3 weeks. Longer use is possible on the recommendation of a doctor. For genital diseases associated with the human papillomavirus, take 1 capsule orally once a day in combination with immunomodulator drugs used as standard treatment for these diseases. In this case, both sexual partners must undergo treatment.
Storage conditions
Store in a dry place at room temperature.
Best before date
2 years.
Conditions for dispensing from pharmacies
Over the counter.
Buy Indinol caps. 300 mg No. 60 in the pharmacy
Price for Indinol caps. 300 mg No. 60
Instructions for use for Indinol caps. 300 mg No. 60
Indinol Forto
Indinol Forto (indolecarbinol) is a selective estrogen receptor modulator. Indicated for specific conditions of the mammary glands, which manifest as discomfort and are characterized by pain of varying severity. Prevents hyperplasia of mammary gland tissue. It is an estrogen antagonist. Suppresses excessive proliferation of mammary gland tissue, because causes loss of viability of cells with pathologically high proliferative activity. Potentiates the reaction of the addition of a hydroxyl radical to the estrogen molecule in the 2nd position. The resulting metabolic product blocks the activation of estrogen receptors. As a result, the expression of estrogen-dependent genes is suppressed, which leads to a decrease in stimulation of cells and tissues by estrogen. The use of the drug as part of a full medication course allows you to reduce the intensity and/or completely relieve pain in the mammary gland. Using this medicine does not cause weight gain. The drug has virtually no toxicity. A single dose of Indinol Forto is 200 mg, the frequency of administration is twice a day. The duration of the course of pharmacotherapy is six months. The drug has a favorable safety profile and is well tolerated by women. Possible side effects: lengthening or shortening of the menstrual cycle, epigastric pain, weight loss. In clinical studies, the incidence of side effects in the experimental group was only 6% higher than in the control group (placebo group).
All observed side effects were mild and went away on their own or with minor therapeutic intervention. Indinol Forto is contraindicated in case of individual intolerance to the drug, during pregnancy and breastfeeding. The drug is not used in pediatric practice. Indinol Forto does not affect the ability to drive a car and work with potentially dangerous mechanisms that require increased attention and concentration. Signs of drug overdose: vomiting, diarrhea. Treatment is symptomatic. The active component of the drug indolecarbinol affects the activity of the CYP2C19 and CYP3A4 isoenzymes, which are responsible for the metabolism of foreign organic compounds and drugs, so care must be taken when combining Indinol Forto with drugs in the metabolism of which these isoenzymes are involved: indirect anticoagulants (dicoumarin, warfarin, syncumar ), glucocorticosteroids (beclamethasone, budesonide, hydrocortisone, dexamethasone), tableted antidiabetic drugs (metformin, glibenclamide), antiarrhythmic drugs (amiodarone, sotalol), antiepileptic drugs (carbamazepine, valproic acid), digitalis preparations (digoxin).