Some medications, such as glucocorticoids and immunosuppressants, may suppress the development of vaccine immunity. In such cases, vaccination tactics should be discussed with your doctor.
For vaccines against the new coronavirus infection, the duration of vaccine immunity remains one of the main questions. It is very difficult to predict the duration of protection of a particular vaccine. This is usually determined in practice by recording the frequency of infections in people vaccinated during mass vaccination after different amounts of time, as well as measuring the titer of protective antibodies.
What are antibodies to coronavirus?
Antibodies (also known as immunoglobulins) are special proteins that are produced and/or produced by plasma cells.
What do immunoglobulins do?
Immunoglobulins are formed in response to foreign bacteria or viruses entering the body. They interact with the antigen (specific site of the pest) and neutralize it.
Thus, our immunity guards our health.
What classes of immunoglobulins are there?
There are 5 classes of immunoglobulins
, some of which contain subclasses.
IgA - secreted on the surface of the epithelium and present in saliva, tears, and on the surface of mucous membranes.
IgM - detected upon initial exposure to antigen.
Indicates an acute infectious process in humans.
IgG is the main class of immunoglobulins that protects against viruses, bacteria, and toxins.
IgD is found on the surface of developing B lymphocytes. The function is not installed.
IgE - secreted during an immediate allergic reaction.
How are antibodies related to immunity?
This is one of its main tools in the fight against threats. Antibodies are not independent cells, but protein structures that are created by protective cells (lymphocytes) for a specific target. It happens that it turns out to be completely harmless substances - for example, pollen or chicken egg whites. This is how an allergic reaction occurs. But most often, antibodies fight viruses, bacteria, parasites and other “saboteurs”.
Antibodies can also be produced against the body’s own cells—they are called autoimmune. Each cell of the body has special protein molecules - identification marks that say that it is “our own”. But if the cell has grown old, died or degenerated into a malignant one, an “order” for destruction is also sent against it.
What to choose – qualitative or semi-quantitative analysis?
Why is qualitative and quantitative analysis carried out?
Qualitative analysis allows us to answer 2 questions:
- Were you sick or not?
- How long have you been sick?
A semi-quantitative test can answer these questions and also determine the amount of immunoglobulins in the body.
Why determine the amount of immunoglobulins?
Determining the amount of antibodies allows you to determine whether long-term immunity has been formed. It is what protects the body from re-infection with coronavirus.
Why are antibodies not immediately formed during illness?
To create the right antibody, the immune system first needs to study the offender. To achieve this, different “departments” cooperate in the body. First, interceptor cells (macrophages) absorb and digest foreign particles. Then they are introduced to their structure of “laboratory” cells (B-lymphocytes). They, in turn, form many copies of themselves with different variants. The “memory” of immunity is not based on antibodies alone. Cells also have it. Lymphocytes that produce antibodies remain dormant until they encounter the pest again. At the right moment, they can quickly create new “shells”. True, such preparation also has a downside, which prevents the creation of effective vaccines against some viruses.
When faced with a familiar virus, the body first throws into battle the cells that were trained to attack it. He suspends the development of new antibodies to save energy. But the virus can mutate in such a way that its vulnerabilities are protected, and the immune system does not recognize this. Even worse: the virus can use the antibody attached to it to enter an immune cell and infect it.
Decoding the results of the test for antibodies to coronavirus
How to decipher a qualitative coronavirus antibody test
| Yes/No | Ig G (Eat) | Ig G (No) |
| Ig M (Yes) | 1 option | Option 2 |
| 5-10 weeks have passed since infection. IgM is still present in the blood, but IgG is already being formed | Acute phase of the disease. 1-3 weeks have passed since infection | |
| Ig M (No) | Option 3 | Option 4 |
| Several months have passed since the illness. You may have had the disease asymptomatically | You have not encountered any viruses or no more than 7 days have passed since infection |
Antibodies to coronavirus - table with interpretation of results
In the 2nd and 4th version
(if there are suspicious symptoms), it is recommended to take a PCR test for coronavirus to identify the pest.
The complete absence of immunoglobulins may also mean that:
1) The preparation conditions were not met and the result was distorted
2) The symptoms of influenza or ARVI were similar to the symptoms of coronavirus,
3) The patient suffered a mild form of the disease and did not develop antibodies.
4) The patient suffered a severe form of the disease, and the antibodies quickly disappeared.
How to prepare for analysis
To test for ANA, venous blood is needed.
Rules for preparing for the study:
- We recommend donating blood between 8 and 11 am;
- blood must be donated on an empty stomach, after an 8-12 hour overnight fast;
- on the eve of the study - a light dinner with limited intake of fatty foods;
- on the day of the test, you can drink still water and it is better to avoid coffee and tea;
- 24 hours before the test, exclude alcoholic beverages;
- 1 hour before the test it is better to refrain from smoking;
- 24 hours before the study, exclude the use of medications (in consultation with the attending physician);
- 24 hours before the test, eliminate emotional and physical stress;
- You should not donate blood after radiography, ultrasound, massage, endoscopic and physiotherapeutic procedures;
- It is recommended to rest for 10-20 minutes before donating blood.
Ig G - interpretation of the test for antibodies to coronavirus
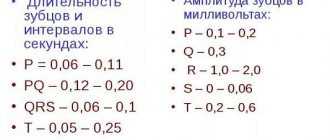
To determine class G immunoglobulins in the blood, a qualitative and quantitative method for determining antibodies is used. Below is a table with a breakdown of the enzyme immunoassay for coronavirus (igG indicator for coronavirus).
Coronavirus antibody index - transcript of captions
| Result | Index | Meaning |
| Negative | Less than 0.8 | The patient either did not encounter the disease or underwent the procedure in the acute phase. |
| Border | 0,8-1,1 | You need to do a repeat test after 14 days. Perhaps the test was done at the onset of the disease or during the recovery process. |
| Positive | More than 1.1 | This level of antibodies to coronavirus in adults is normal. The person had coronavirus infection several months ago, and humoral immunity had time to develop. |
Class G antibodies to coronavirus - interpretation of results
An antibody titer to coronavirus of 1,800 (positive result) is normal. In this case, immunoglobulins of class A and M should be absent in the blood. Their presence indicates the stage of recovery.
Titer? What other title?
As we have already found out, antibodies are proteins that circulate in the blood. In order to provide effective protection, these proteins must be in the blood at a certain concentration - this is called the titer. Express titer as numbers separated by colons, for example 1:50 or 1:100 (read as “one in fifty” or “one in one hundred”).
Since antibodies are complex proteins, it is extremely difficult to determine them by chemical methods. Therefore, immunological reactions are used to determine antibodies. There are a lot of specific methods, but in the most general form the essence of these reactions is very simple. We take a solution of the desired antigen (for example, the same spike protein of the coronavirus) and mix it with the serum in which we are looking for antibodies. If there are antibodies in the serum, they bind to the antigen and their compound precipitates or the solution becomes cloudy. In practice, carrying out such a reaction looks more complicated; special gel media and different detection methods are often used, but this does not change the essence.
The problem is that this approach only answers the question of whether there are antibodies in the serum or not, but does not tell us anything about the amount of antibodies themselves. How, then, can two different serums be compared with each other? The amount of sediment that fell is not an option, the error is too large. But there is another way - you can dilute the test serum until the reaction (precipitate) is still detectable. And the last, strongest dilution, at which we can still observe the reaction of the serum with the antigen solution, is called the titer of this serum. That is, a titer of 1:50 tells us that this serum can be diluted 50 times and it will still react with the antigen. Accordingly, the larger the second digit in the titer designation, the higher the concentration of antibodies in the serum.
The disadvantage of a titer is that it indicates the relative abundance of antibodies. If we have two sera with titers of 1:50 and 1:100, we can confidently say that the second serum contains 2 times more antibodies than the first. But we do not know what exactly the concentration of antibodies is in each of these sera. In practice, this often happens and is not necessary: it is enough for us to know with what titer of antibodies a person is still protected from infection, and with what titer he is no longer protected. This can be easily determined by measuring antibody titers in vaccinated people who still become infected.
Laboratory test results usually report antibody concentrations in international units (IU) or relative units (RU). The results obtained in IU can be compared with each other - the value will not depend on the laboratory, test system and analysis conditions (there are no such conditions for coronavirus yet). The results, expressed in OE, can be compared with each other only for tests of the same brand, while the laboratory itself and the time of analysis do not play a role, that is, it is possible to track the dynamics of changes in the level of antibodies in one person.
BAU/ml - new interpretation of the test for antibodies to coronavirus
The World Health Organization has approved a new international standard for the determination of immunoglobulins for coronavirus, with the unit of measurement BAU (translated as “binding antibody coefficient”).
Interpretation of quantitative analysis for antibodies to coronavirus
Laboratory diagnostics
the level of immunity protection against coronavirus is carried out by studying immunoglobulins to the S-protein of the virus. To facilitate the interpretation of the study results, it was proposed to use a universal measurement system.
Conversion table for antibody test results from different manufacturers in BAU/ml
| Manufacturer | Conversion factor to BAU/ml |
| Abbott ARCHITECT | 0,142 |
| Roche | 1 |
That is, antibodies destroy viruses and bacteria?
Not really. The purpose of antibodies is to neutralize the “intruder” so that it cannot reproduce, or to mark it for destruction. For example, they stick to viral particles, preventing them from entering the cell. Since the virus is unable to reproduce outside cells, it dies. Antibodies can also clump bacteria together into clumps, which are then devoured by phagocytes, or activate a system of immune proteins that will break through the bacterial membrane and kill it.
An antibody works like a molecular master key: it is born already tailored to a certain structural feature of a foreign body. For example, this could be a site (spike) on the surface of a viral particle through which it binds to a cell. The antibody blocks the spike and the virus cannot infect the cell. Related viruses may have similar structural elements, and then antibodies to one member of the family will be effective against another. For example, some people who have had SARS in the past (caused by the SARS-CoV-1 virus) already have effective antibodies against its relative, SARS-CoV-2, which causes COVID-19 infection.
What else is prescribed with this study?
Humoral immunity (immunoglobulins IgA, IgM, IgG, IgE, circulating immunocomplexes, complement components C3, C4)
17.51. Ven. blood 8 days
2,740 ₽ Add to cart
Immune status (screening) (Phagocytic activity of leukocytes, cellular immunity, total immunoglobulin IgE, immunoglobulins IgA, IgM, IgG)
27.960. Ven. blood 3 days
5 880 ₽ Add to cart
Total immunoglobulin IgE
17.2. Ven. blood 1 day
400 ₽ Add to cart
Cellular immunity (T-lymphocytes, T-helpers, T-cytotoxic cells, Immunoregulatory index, B-lymphocytes, NK-T cells, NK cells, Leukocyte formula)
17.50. Ven. blood 3 days
4,170 ₽ Add to cart
Serum paraprotein typing using immunofixation
50.28.2181 Ven. blood 14 days
4,000 ₽ Add to cart
What is the "positivity rate"?
Semi-quantitative tests are used in most cases to determine antibody levels after vaccination. They do not show the exact amount of antibodies formed. But with their help, you can assess the intensity of the immune response - by the brightness of the sample, if the test is carried out using the enzyme-linked immunosorbent assay (ELISA).
Tests from different manufacturers have different scales. In most cases, state laboratories use Vector-best test systems, and their cut-off level is 1. That is, if the indicator is lower, there are no antibodies. From 1 to 1.1 is the so-called gray zone. If the result is higher than 1.1, it means that we have a strong positive reaction of the immune system.
The “positivity rate” shows how many times the level of antibodies in the sample exceeds the threshold level for their recognition. So, for example, the indicator of 15, which the president recently spoke about, is a good result. The majority of those vaccinated with Sputnik V or CoviVac have approximately the same or even higher rate of positive immune response.
At the same time, I would like to note once again that other test manufacturers may have a different scale and, accordingly, different indicators. At the same time, when you receive the test result in the laboratory, you can always see the reference values on the form and compare the result with them.
What does the appearance of antinuclear antibodies in the body indicate?
The presence of antinuclear antibodies indicates the development of autoimmune pathologies in the body:
- rheumatoid arthritis;
- systemic scleroderma;
- periarteritis nodosa;
- systemic lupus erythematosus;
- dermatomyositis, polymyositis;
- Sjögren's syndrome;
- myasthenia gravis;
- mixed connective tissue disease.
A less pronounced increase in antinuclear antibodies is typical for:
- other diseases of an autoimmune nature: type 1 diabetes mellitus, Bazedow's disease, Hashimoto's thyroiditis;
- infections: tuberculosis, bacterial endocarditis, tuberculosis, viral hepatitis;
- lung and liver tumors;
- pulmonary fibrosis, hepatic cirrhosis;
- taking ACE inhibitors, some anticonvulsants, antituberculosis drugs, lithium, cholesterol-lowering drugs.
Antibodies IgA, IgG, IgM. Importance in the diagnosis of infections
Antibodies are proteins that the immune system produces in response to infection. In laboratory diagnostics, it is antibodies that serve as markers of infection. The general rule for preparing for an antibody test is to draw blood from a vein on an empty stomach (at least 4 hours must pass after eating). In a modern laboratory, blood serum is examined on an automatic analyzer using appropriate reagents. Sometimes a serological test for antibodies is the only way to diagnose infectious diseases.
Tests for infections can be qualitative (they answer whether there is an infection in the blood) or quantitative (they show the level of antibodies in the blood). The level of antibodies for each infection is different (for some there should be none at all).
Different classes of antibodies
Enzyme immunoassay determines infectious antibodies belonging to various Ig classes (G, A, M). Antibodies to the virus, in the presence of infection, are detected at a very early stage, which ensures effective diagnosis and control of the disease. The most common methods for diagnosing infections are tests for IgM class antibodies (acute phase of infection) and IgG class antibodies (sustained immunity to infection). These antibodies are detected for most infections.
A detailed diagnosis of the type and amount of antibodies for a diagnosed disease can be done by taking an analysis for each specific infection and type of antibodies. Primary infection is detected when a diagnostically significant level of IgM antibodies is detected in a blood sample or a significant increase in the number of IgA or IgG antibodies in paired sera taken at an interval of 1-4 weeks.
Reinfection, or repeated infection, is detected by a rapid rise in the level of IgA or IgG antibodies. IgA antibodies have higher concentrations in older patients and are more accurate in diagnosing ongoing infection in adults.
Previous infection in the blood is defined as elevated IgG antibodies without an increase in their concentration in paired samples taken at an interval of 2 weeks. In this case, there are no antibodies of the IgM and IgA classes.
IgA antibodies
They appear in the serum 10-14 days after the onset of the disease, and at first they can even be detected in seminal and vaginal fluids. The level of IgA antibodies usually decreases by 2-4 months after infection if treatment is successful. With repeated infection, the level of IgA antibodies increases again. If the level of IgA antibodies does not fall after treatment, then this is a clear sign of a chronic form of infection.
IgG antibodies
The main role of IgG antibodies is the long-term protection of the body from most bacteria and viruses - although their production occurs more slowly, the response to an antigenic stimulus remains more stable than that of IgM class antibodies.
Levels of IgG antibodies rise more slowly (15-20 days after illness onset) than IgM antibodies, but remain elevated longer, so may indicate a long-standing infection in the absence of IgM antibodies. IgG antibodies may remain at low levels for many years, but upon repeated exposure to the same antigen, IgG antibody levels rise rapidly.
For a complete diagnostic picture, it is necessary to determine IgA and IgG antibodies simultaneously. If the IgA result is unclear, confirmation is carried out by determining IgM. In case of a positive result and for an accurate diagnosis, a second test, done 8-14 days after the first, should be checked in parallel to determine the increase in the concentration of IgG antibodies. The results of the analysis must be interpreted in conjunction with information obtained in other diagnostic procedures.
IgM antibodies
Their concentration increases soon after the disease. IgM antibodies are detected within 5 days after its onset and reach a peak between 1-4 weeks, then decrease to diagnostically insignificant levels within several months, even without treatment. However, for a complete diagnosis it is not enough to determine only IgM class antibodies. Their absence does not mean the absence of the disease. There is no acute form of the disease, but it may be chronic.
IgM antibodies are of great importance in the diagnosis of hepatitis A and childhood infections (rubella, whooping cough, chickenpox), easily transmitted by airborne droplets, since it is important to identify the disease as early as possible and isolate the sick person.
Antibody analysis in the diagnosis of TORCH infections
The abbreviation TORCH appeared in the 70s of the last century, and consists of capital letters of the Latin names of a group of infections, the distinctive feature of which is that, while relatively safe for children and adults, TORCH infections during pregnancy pose an extreme danger. Often, infection of a woman with TORCH complex infections during pregnancy (the presence of only IgM antibodies in the blood) is an indication for termination.
Epilogue
Sometimes, having discovered IgG antibodies in the test results, for example, toxoplasmosis or herpes, patients panic, not realizing that IgM antibodies, which indicate the presence of a current infection, may be completely absent. In this case, the analysis indicates a previous infection to which the body has developed immunity.
In any case, it is better to entrust the interpretation of the test results to a doctor, and, if necessary, decide on treatment tactics with him. And you can trust us to conduct the research!
Go to the catalog section DIAGNOSTICS OF INFECTIOUS DISEASES
.
WHY IS IT FASTER, MORE CONVENIENT AND MORE PROFITABLE TO TAKE ANALYSIS TO ANALYZ-MARKET?
- The check amount won't shock you.
A permanent discount of up to 50% from average market prices applies to all our analyses, because... you interact with the laboratory directly, avoiding intermediaries.
- You don't have to be on time or wait in line.
Placing and paying for an order takes place online in 2 minutes, and taking tests can be done on any day and time period convenient for you.
- The journey to the nearest medical center will take no more than 20 minutes.
We make sure that they are located near your home or office.
- You don't have to wait long for results or go back and forth to get them.
They will appear in your personal account automatically when ready.
Meaning of the analysis results
The test for antinuclear antibodies is carried out in the form of:
- chemiluminescence immunoassay, its purpose is screening (selection for further examination);
- immunoblotting with separation of antibody types - needed to clarify the diagnosis.
In a screening test, a positive result indicates that the patient has some kind of connective tissue disease. This test is performed upon the patient’s initial visit. If the result is negative, it is impossible to completely exclude the autoimmune process.
Immunoblotting shows which types of antibodies predominate and their combinations. This blood test is more complex and expensive, but it helps to more accurately determine the cause of the increase in ANA in the blood.