Treatment of dermatomycosis is carried out through local therapy with antifungal creams, the use of antibiotics and agents to enhance immunity. Disinfection of shoes and clothing is mandatory.
Ringworm is a fungal infection that affects most of the human body. The affected area has a ring-shaped shape, while in the middle of the affected area with flaky and inflamed edges, the skin has a healthy appearance.
Dermatosis can appear on the following areas of the body:
- scalp;
- nails;
- smooth body skin;
- groin area;
- feet;
- facial skin where vegetation is located.
Infection with dermatomycosis
This infectious disease is quite common. If you identify and begin to eliminate the disease in a timely manner, and follow all the doctor’s recommendations, then such effective therapy will give positive results. However, it may also happen that when the disease is advanced, its chronic form develops.
Infection with dermatomycosis occurs through direct contact with a sick person, or through contaminated objects. Such objects may include towels, shoes, and carpets. Some types of fungus live on damp surfaces, such as the floor of a locker room, bathhouse, or shower. The fungus can be contracted from pets suffering from ringworm (ringworm).
The causative agent of the disease is a fungus of the genera Microsporum, Trichophyton, Achorion.
Where is it most often found?
According to various sources, up to 20 percent or more of adults are affected by various forms of dermatomycosis. The reasons leading to the appearance of this disease include a decrease in immunity in combination with difficult environmental conditions - lack of ventilation, airtight shoes, clothing.
Hence the main risk groups:
- aged people;
- HIV patients;
- miners, metallurgists, athletes, military.
Public swimming pools and saunas, as well as gyms, are the main “supplier” of mycotic infections.
Symptoms and treatment depend on the specific species.
Symptoms of ringworm
Dermatosis of the scalp mainly affects children. This is characterized by the formation of small, gradually multiplying papules, flaking of the scalp and hair loss in the affected areas. Also, boil-like, inflamed nodes may appear in the area of papules. This disease is caused by microsporum or trichophyte.
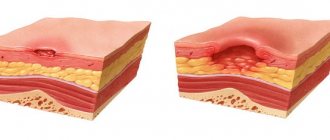
If dermatomycosis affects the smooth skin, papules spread to any area of the skin, flat formations are formed, covered with scales and dry, or wet and covered with crusts. Based on the degree of enlargement of the papules, the centers of the formations are cleared, giving a classic picture in the form of circles. This form of the disease is caused by the fungus trichophyton.
The onset of ringworm of the fingernails and toenails is observed at the tips themselves. In cases of hand nail disease, the disease is detected much less frequently compared to the first case. The disease becomes a consequence of gradual thickening of the nail plate, curvature or change in shade. A substance formed from dead cells accumulates under the plate. Eventually, the nail may completely collapse.
Ringworm of the feet causes fine-plate peeling of the skin and the formation of blisters between the toes. In severe forms, the infection can cause inflammation of the foot, characterized by increased itching and pain when walking.
Dermatomycosis of the groin area is determined by the appearance of reddened spots with clear outlines in the affected area. The designated lesions can spread to the buttocks, external genitalia and inner thighs. This form manifests itself mainly in men who wear tight sports underwear and live in a warm climate area. Tinea groin is caused by different types of fungi, as well as yeast. Relapses of this disease often occur because the fungi remain viable on human skin for a long time.
Treatment of the disease is individual, it depends on the form of manifestation. At the first signs, you need to contact an experienced specialist. After all, based on the form of the disease, skin lesions differ in appearance and duration of existence of the pathogen.
Classification
Dermatomycoses are classified according to location:
- smooth body skin;
- scalp and beard;
- nails;
- groin area;
- stop.
Depending on the pathogen, dermatomycosis is classified into:
- keratomycosis: nodular microsporia, lichen versicolor;
- dermatophytosis: athlete's foot, athlete's foot, trichophytosis, imbricate mycosis, favus, rubrophytosis;
- deep mycoses: aspergillosis, chromomycosis, blastomycosis, sporotrichosis, etc.;
- candidiasis: superficial, visceral and chronic generalized;
- pseudomycosis: actinomycosis, trichomycosis, erythrase, etc.
Diagnosis of ringworm
Very often, skin diseases have similar symptoms, but require different treatment. For this reason, the correct diagnosis can only be made by a specialist by taking a sample of the infected nail or skin for culture (culture) or microscopic examination. Culture can determine the type of fungus, but the process takes some time because the fungus develops slowly.
So, the diagnosis is established on the basis of clinical and epidemiological information, including the results of laboratory examinations. In laboratory examinations, the material used is hair, skin scrapings, scales and crusts from peripheral or infected areas that have not been treated.
During microscopic examination, the pathological material is placed in a Petri dish or on a watch glass and filled with a 10 percent sodium hydroxide solution, after which it is placed in a thermostat for 15-20 minutes or slightly warmed up and split with dissecting needles. The required volume of material is applied to a glass slide in a drop of glycerol (50%), covered with a glass slide and examined under a microscope.
Microscopic examination reveals Trichophyton fungi in the form of straight mycelial hyphae with septa. The spores are oval, round, unicellular, located at the base in chains or clutches.
Microsporum fungi are single-celled round spores located randomly on the surface of the hair or inside it.
Achorion mushrooms, in the form of thin mycelium, consist of rectangular cells with two contours. The spores are multifaceted or round, arranged in groups or chains.
In the differential diagnosis of dermatomycosis, the luminescent method is widely used. If necessary, inoculations are made from the original raw material onto agar.
Treatment of ringworm
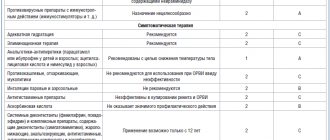
As a rule, ringworm is treated with topical products. The duration of local treatment can be two weeks after symptoms disappear. During treatment, moist, open bandages should be used.
Treatment tactics are selected for each patient individually, based on the type of pathogen, the course of the disease, and the general condition of the body.
In this case, local therapy with antifungal creams, ointments, alcohol tinctures, aerosols and course use of tablets, including antibiotics, are used. At the same time, means are used to enhance immunity and tissue regeneration (immunomodulators, vitamins). Patients also learn methods of disinfecting shoes and clothing, and hygiene skills.
Basically, creams should be applied to the affected areas of the skin 2 times a day, the course of therapy should last about 7-10 days after the last symptoms have disappeared. If therapy was completed prematurely, a relapse may occur.
When treating such a disease, you need to take into account the fact that medicinal creams do not have an immediate effect. The therapeutic effect of their use appears after a few days. Therefore, together with antifungal creams, it is advisable to use hormonal (corticosteroid) agents to relieve pain and itching.
For long-lasting forms of the disease, long-term courses of treatment are recommended. For several months, the patient takes oral medications (for example, griseofulvin) along with local therapy. General or local antibiotics may also be added to treatment.
Treatment of fungal diseases in our clinic is carried out by a dermatologist. At the same time, a comprehensive examination is carried out at an innovative level, which allows us to identify the subtlest disorders of the body and accurately determine the diagnosis with the achievement of complete recovery.
Causes
Speaking about the etiology of the disease, it is important to take into account that the causative agents are a variety of fungi: microsporum, trichophyton, epidermophyton (the latter group includes varieties of this type of fungus, all of them are united under the common name “dermatophytes”). It is always extremely difficult to identify pathogens in body tissues, since a specialist must first isolate a pure culture for research.
Another difficulty is that the causative agents of dermatomycosis are very common, so infection occurs easily, and in some cases such manifestations may have something in common with epidemic symptoms. Most often, dermatomycosis is characteristic of countries with a tropical climate, that is, humid and hot, since fungi usually multiply actively at a temperature of 25-30 degrees Celsius. The summer season and alkaline environment are ideal for them. At the same time, experts say that children are much more likely than adults to become infected.
As a rule, the pathogen appears on the skin after a person has been in contact with the lesion for some time. Doctors distinguish three main types of pathogens:
- bestiality;
- geophilic;
- anthropophilic.
The source of infection in the first case is animals, or rather, parasites living in their bodies. This includes parasites that use domestic dogs, cats or cattle as hosts.
In the second case, we are talking about pathogens living in the ground and soil. A person can work or simply come into contact with the ground without using protective equipment, and as a result become infected.
The third case is parasites that live in the body of a person who is a carrier of the disease. The very fact of infection occurs through contact.
The development of dermatomycosis is expressed in the fact that conidia and hyphal fragments of pathogens enter the hair, upper layers of the skin, and nails (that is, those tissues that contain keratin). The degree of infection in dermatophytes is quite low, so tissue damage does not appear in healthy people. However, pathogens have a characteristic feature: they can subject keratin to complete destruction and destruction.
Pathogens located in the hair shaft can be divided into two types based on their growth. First: endothrix begin to grow from the skin into the hair and follicles, but they do not go beyond the boundaries of the hair shaft itself. Second: ectothrix grow directly into the hair directly from the hair follicle.
Much in the occurrence and development of the disease depends on the characteristics of the person’s body. Some types of dermatomycosis may be characteristic exclusively of an adult, while others - only of a child. In many ways, the disease is caused not only by age, but also by the secretion of the sebaceous glands, the composition of sweat and many other characteristic features.
Primary infection with dermatomycosis is a consequence of sensitization, after which it is time for a relapse to develop. Immunodeficiency largely determines the level of risk of dermatomycosis. In addition, various metabolic disorders, poor nutrition, problems with the hormonal system, and vitamin deficiency can also become a favorable background for infection. It is also important to remember that the fungus penetrates damaged skin faster, so people with ulcers, wounds and scratches on the skin are at particular risk.
Conidia, hyphae, and spores penetrate hair, nails and skin. Since the nutrient medium for the fungus is, first of all, keratin, the epidermis after infection begins to deteriorate at a rapid pace. In this case, healthy areas of the skin are also affected.
Prevention of ringworm
The best preventative measure is to keep the skin dry and clean. You must also adhere to the following simple rules:
- there is no need to immediately change into house shoes, allowing your feet to “breathe”;
- change your underwear and socks every day;
- dry your feet in the sports locker room or pool shower;
- no need to walk barefoot on beaches and public places;
- in hot weather, you should not wear tight clothes;
- You shouldn’t wear someone else’s or old shoes, you shouldn’t use other people’s things and give your things;
- Carefully inspect your pets' fur for the presence of lichen.
Risk factors
Some diseases may predispose to the development of mycoses:
- AIDS
- diabetes mellitus and endocrine diseases
- diseases of the gastrointestinal tract and urinary system
Treatment with certain drugs can also provoke the disease: we are talking about long-term use of corticosteroids, immunosuppressants and antibiotics.
Very often, mycoses occur in athletes, military personnel, and heavy industry workers. After all, people from these areas often use shared showers and locker rooms, wear overalls and heavy closed shoes.⁶