How to treat ringworm in humans at home
Ringworm is a highly contagious (contagious) infectious disease of the skin, hair or nails caused by pathogenic fungi. The infection can be caused by two types of fungi - Trichophyton and Microsporum. The correct designation of the disease is based on the name of the fungus that caused it, so doctors distinguish trichophytosis and microsporia.
Both of these forms of fungal infection (trichophytosis and microsporia) are combined under the general term ringworm. Thus, ringworm is also called trichophytosis, microsporia, dermatophytosis, dermatomycosis or dermatophytosis. Trichophyton fungi are microbes that parasitize only on human skin, while Microsporum infect both humans and animals. Ringworm is most contagious in children 4 to 13 years of age.
In the article we will look at ringworm, the causative agent of the disease, its symptoms, routes of infection, as well as preventive measures in the table.
Causes
The fungus Trichophyton tonsurans was first identified many decades ago. Its name is directly related to its ability to attack hair. Fungi that parasitize humans cause superficial and chronic ringworm. And bestial forms cause infiltrative-suppurative skin lesions.
- Chronic diseases and vitamin deficiency contribute to the appearance of deprivation.
- Infection occurs after contact with a sick person or his hygiene items, when working with hay and soil, after contact with an animal.
- More often, the disease occurs against a background of decreased immunity and violation of personal hygiene rules, long-term care of animals and damage to the outer covering of the body (scratches, abrasions, burns).
We will tell you further about the symptoms and signs of ringworm in children and adults.
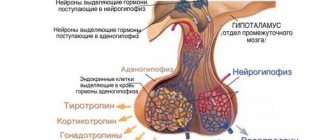
Pathogens
Pathology is caused by parasitic fungi of the genus Microsporum. The pathogen received this name because as a result of its vital activity it forms multiple small spores. Most often found in the middle zone are Microsporum canis and Trichophyton tonsurans.
Microsporum canis is a zoonotic fungus. If it comes into contact with a person, it causes a mild form of the disease and responds well to treatment.
Trichophyton tonsurans is an anthroponotic fungus. Only people become infected; it is severe and becomes chronic.
In soil and pathological material, fungi persist for up to 7 years.
This is interesting - popular questions about trichophytosis
| Question | Answer |
| Is ringworm contagious? | Yes, ringworm is an infectious and highly contagious disease. |
| Does ringworm itch or not? | The disease causes itching, and in some cases it can cause severe anxiety to the patient. |
| Can ringworm go away without treatment? | The possibility of ridding the body of ringworm on its own exists, but it is negligible. Science knows of several cases where the disease resolved without any medical intervention, however, these are isolated phenomena. Most often, the infection, having caused inflammation once, begins to spread further. If the disease developed in childhood and was not treated, it will persist until adulthood. |
| What should I do if I get ringworm during pregnancy? | Do not panic if the infection develops during gestation, since these mycotic organisms are not able to have a pronounced effect on either the child or the woman. If infected, you should consult a doctor and undergo the treatment recommended by him. During pregnancy, oral medications are not prescribed to get rid of the infection; it will be enough to use ointments prescribed by the doctor. |
| Can ringworm reoccur? | The disease can develop again if there has been a new infection, or treatment has not been completed. The body is unable to form immunity against ringworm fungi. |
| Is it possible to wash yourself if you have ringworm? | The disease is not a contraindication to hygiene procedures. When you are sick, it is best to take a shower rather than a bath. |
Which doctor should I contact?
If an adult or child has symptoms of ringworm, you should immediately consult a doctor. This could be a dermatologist or infectious disease specialist.
The doctor, using the diagnostic methods available to him, will confirm or deny the fact of infection and prescribe the appropriate treatment. It is worth remembering that without treatment, ringworm can provoke very unpleasant consequences in the form of baldness or suppuration, and can also be spread to other people.
In addition, there is a possibility that the symptoms of ringworm hide diseases such as atopic dermatitis, psoriasis, lichen planus, alopecia areata, etc.
Read more: Alopecia areata in children and adults
Incubation period of the disease
The incubation period of the fungal infection that causes the appearance of ringworm ranges from several days to 6–8 weeks and depends on the type of pathogen that has entered the body.
Superficial lichen may appear as the first symptoms within 5-7 days after infection. Infiltrative-suppurative lichen does not give any clinical manifestations for several months. The first signs of the disease appear no earlier than 6-8 weeks after the pathogen enters the body.
Pills
Prescribed for severe inflammation of the skin. Taking pills speeds up recovery.
- Orungal. Stops the development of dermatophyte and kills it. The course of taking the drug is 15 days, 100 mg per day.
- Griseofulvin. Stops the development of the parasite. Directions for use: 8 times a day with a spoonful of sunflower oil. Use until laboratory results are negative.
- Lamisil. Destroys dermatophyte. Use for 2.5 months, 1 tablet 2 times a day.
All of these drugs are effective, but you should not choose your own medicine. The specialist decides how best to treat ringworm for a particular patient.
Symptoms
What does ringworm look like in the initial stage, how to recognize it in time and prevent hair loss? Unfortunately, a person may not notice the first signs of the disease immediately. Any area of the scalp begins to lose its vegetation. The hairs gradually thin out, fall out and break, changing their length to 1 - 2 mm. Peeling of the skin adds to the problem. As the disease progresses, the lesion acquires clear outlines.
Symptoms of ringworm (see photo) are more noticeable on the chest, back, lower and upper extremities. A person may notice such deviations as:
- burning and itching spots;
- redness and swelling of the skin;
- framing the hearth with a solid roller;
- blistering of the lesion with subsequent leakage of contents and the formation of crusts.
If nails are affected by trichophytosis, the plates become brittle and dull. Their structure thickens and coarsens. Subsequently, the nails crumble and change color. Dents on the plates, grooves and a dirty gray color are a characteristic sign of lichen.
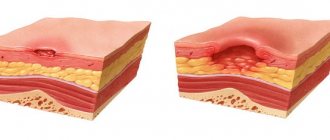
In addition to ringworm patches on the head, problem areas can also appear on the body. The disease manifests itself as a rash, the elements of which are similar to round red spots. Since the fungus feeds on keratin taken from the upper epidermal layers, the skin elements gradually acquire the contours of a ring. Having “eaten” the keratin in one area, parasitic microorganisms move on. This is why plaques grow in diameter and change the boundaries of their edges.
The accumulation of dermatophytes leads to the formation of a bright border. Its bubbly and scaly appearance indicates increased fungal activity in this area. Sometimes the parasites return to the center of the ring and again use it as a source of nutrition. But this is only possible when keratin reserves are restored. The so-called “ring within a ring” is a clear sign of increased dermatophyte activity.
Chronic ringworm
It can be localized on the scalp, fingernails or smooth skin. On the head, lesions are localized, for the most part, at the temples and the back of the head. The lesion is a small (no more than 0.5 cm) smooth scar, similar to an atrophic one, which peels off a little, but has no signs of an inflammatory reaction. At the site of this lesion, the hair breaks off at the very root, forming a spot called a blackhead.
Chronic ringworm on smooth skin is most often localized on the buttocks, thighs, knee and elbow joints, or palms. In this case, the lesion looks like a bluish or pinkish spot of a fairly large size with a vague outline. The surface of the spot is moderately peeling.
Typically, lesions are characterized only by mild itching; there are no other subjective symptoms. Nails affected by lichen become dull, cloudy, gray in color, the outer edge becomes jagged and is easily painted. The nail can suddenly become very thick or, on the contrary, thin.
Diagnostics
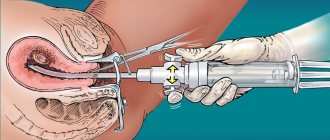
The diagnosis is based on a visual examination of the patient, as well as collecting a medical history and questioning about possible sources of infection. If in doubt, the doctor will scrape the affected area.
The collected materials are examined under a microscope or placed in a nutrient medium for three days, during which rapid growth of fungal colonies is observed. When filaments of mycelium and spores of a fungal pathogen are detected, its identification is made.
Treatment of ringworm in humans
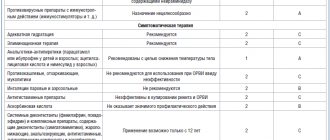
When treating ringworm in humans, the basis of therapy is the fight against the fungus that causes dermatomycosis. Therapy at home combines local treatment with ointments for lichen - antifungal creams, sprays, shampoos with oral antifungal drugs.
The treatment regimen is prescribed by a dermatologist, the main aspects are as follows:
- Ringworm of smooth skin responds better to treatment with Terbinafine and tolnaftate.
- To treat lichen in the morning, a 5% iodine solution is usually used. In the evening, as a rule, sulfur-salicylic or sulfur-tar ointment is prescribed; treatment with pure salicylic acid 3% is also possible.
- A dermatologist can write out a prescription for the production of Vidal's milk in the prescription department of a pharmacy - alcohol, camphor, salicylic acid, sulfur lotion, boric acid, glycerin. Or Lassar pastes - petroleum jelly, starch, salicylic acid, zinc oxide.
- For local treatment, the doctor may recommend various ointments, creams, shampoos containing Clotrimazole, Ketoconazole, Mycoseptin, Terbinafine, Mycoconazole. (Local antifungal agents - creams, sprays, gels).
For systemic treatment of dermatomycosis, Griseofulvin is used; it is a natural antimycotic that has a narrow spectrum of action, namely, it is active against dermatomycete fungi, Trichophyton, Microsporum, Epydermophyton, Achorionum.
- Treatment must be accompanied by oral administration of griseofulvin. It should be taken for 15-25 days, and a bacterioscopic scraping should be taken once a week to detect fungus. As soon as the fungus is not detected, the intake of griseofulvin is continued every other day, at the same dose that the doctor calculated, for another 14 days, so that there is no relapse of the disease.
- If the feet are affected by the fungus, it is recommended that they be treated with Ketoconazole or Clotrimazole orally, and selenium sulfide applied externally.
For the treatment of chronic ringworm, in addition to antifungal agents, both local and oral (Griseofulvin), vitamin therapy, immunomodulators, and drugs that strengthen blood vessels and improve microcirculation are also indicated.
Gels
Gel medications contain a high concentration of the drug. They are quickly absorbed without leaving marks on the skin and clothes:
- Exifin 1%. Apply 2 times a day for 3-4 weeks.
- Mycogel-KMP. It has a destructive effect on the integrity of the cell wall of the dermatophyte and accompanying microorganisms. Used in the same way as Exifin.
Before applying medications, the skin is cleaned of scales, crusts and other dirt.
Hygiene measures when in contact with a sick person
If you or your child have touched a sick animal or interacted with a sick person, then you need to take immediate action.
- The sooner you wash away particles containing fungus from your skin, the less likely you are to become infected.
- Wash your hands several times with antifungal soap. The simplest remedy, which is available in almost every store, is cinnamon laundry soap, or better yet, soap with birch tar.
- Wash your entire body with this soap. Suddenly, particles of the patient’s skin got under his clothes. Do not use a hard washcloth. It leaves micro-scratches on the skin, into which fungus easily penetrates.
- To wash your hair, you must use an antifungal shampoo. For example, Nizoral. You can also use it as a shower gel.
- A modern remedy with a powerful antifungal effect is Citeal. Dilute it in a small container five times. You will end up with a foaming liquid that can be used to wash your hands and entire body.
- Lavender oil, tea tree oil and turpentine have an antifungal effect. They can be used to treat small areas of skin.
Also, five days after contact, it is advisable to consult a dermatologist. He examines the body with a Wood's lamp. If you do become infected, the disease can be detected in the early stages. This will help you quickly treat her at home and avoid going to the hospital.
Contributing Factors
People with low immunity are at particular risk, those who already have a skin disease of non-contagious etiology, if there are wounds or scratches. Frequent stress, depression, and working with soil without gloves increase the risk of contracting an infection.
Microsporia or cat lichen is usually seasonal. Outbreaks occur in August - September. Children become infected through contact with kittens infected with microspores, but outwardly completely healthy.
Adults rarely become infected with this fungus. This is due to the fact that on the skin of an adult there is a conditionally pathogenic fungus that suppresses microspores. Also in adults, undecylenic acid is produced in the sebaceous glands, which suppresses fungus.
An adult can get microsporia in several cases:
- during pregnancy;
- scalp wounds;
- if you wear an infected hat for a long time;
- in hot, humid climates;
- long illness and taking antibiotics.
Trichophytosis is not seasonal; people suffer from it all year round.
Prevention measures
Prevention includes maintaining good personal hygiene and isolating sick animals or people.
At the place where the patient is identified, thorough disinfection is carried out, bed linen and accessories, soft toys, and carpets are subjected to heat treatment. A sick child is not allowed into the children's group until the ringworm is completely cured. Patients are prohibited from visiting swimming pools, saunas, and baths. Kindergarten teachers, nannies, utility workers, and bathhouse attendants are suspended from their duties.
Is ringworm dangerous for humans? The most serious consequences are persistent alopecia areata due to scarring of the skin tissue. The disease should be treated as soon as it begins to manifest itself in order to prevent infection of the immediate environment and reduce the risk of developing a severe allergic reaction.