- General characteristics Definition of hypoxia
- Development of hypoxia
- Exogenous hypoxia
Hypoxia is a pathological condition in which oxygen deficiency occurs in the body due to its reduced supply from the outside and/or due to dysfunctional utilization in cells.
hypoxia
“Hypoxia” – hypo and oxigenium (lack of oxygen), translation from ancient Greek. Most people understand hypoxia as oxygen starvation (lack of oxygen) , because... in this case, tissues and organs experience dysfunction from oxygen deficiency.
General characteristics of hypoxia
Definition of hypoxia
Hypoxia is a typical and dangerous pathological process that occurs in the body during a wide range of diseases and acute conditions, and provokes them. For example, hypoxia can be caused by various factors, and also accompany a wide range of diseases, and may even be the main link in the appearance of pathological changes or diseases.
Based on this:
hypoxia is a typical general pathological process and does not relate to either a diagnosis or a syndrome.
The effect of hypoxia at the cellular level is divided into two types - adaptive reactions and decompensation .
During the occurrence of hypoxia, the body launches adaptive protective reactions that maintain for a short time the almost normal functioning of organs and tissues. With prolonged exposure to hypoxia, the body's reserves run out and adaptive defense reactions are switched off - decompensation occurs.
Decompensation is characterized by the occurrence of irreversible disorders in organs and tissues - from organ failure to death.
Development of hypoxia
Compensatory reactions during hypoxia are expressed by oxygen deficiency at the cellular level, and their task is to restore the amount of oxygen in tissues. The complex of compensatory reactions to eliminate the influence of hypoxia includes the organs of the cardiovascular and respiratory systems, and changes in biochemical processes in tissues and organ structures that suffer most from oxygen deficiency are triggered. Until the supply of compensatory reactions is completely exhausted, organs and tissues will not suffer from a lack of oxygen. However, if, when compensatory mechanisms are depleted, the supply of oxygen is not normalized, then irreversible decompensation will begin in the tissues with damage to cells and dysfunction of the entire organ.
In acute and chronic hypoxia, the nature of compensatory reactions is different. Thus, during acute hypoxia, compensatory reactions consist of increased breathing and blood circulation, that is, blood pressure rises, tachycardia occurs (heart rate more than 70 beats per minute), breathing becomes deep and frequent, the heart pumps a larger volume of blood per minute than normal . In addition, in response to acute hypoxia, all “reserves” of red blood cells, which are necessary to carry oxygen to the cells, are released into the systemic circulation from the bone marrow and spleen.
hypoxia
All these reactions are aimed at normalizing the amount of oxygen delivered to the cells by increasing the volume of blood passing through the vessels per unit of time and increasing the amount of oxygen transferred. With very severe acute hypoxia, in addition to the development of these reactions, centralization of blood circulation also occurs, which consists of redirecting all available blood to vital organs (heart and brain) and a sharp decrease in blood supply to the muscles and organs of the abdominal cavity. The body directs all the oxygen to the brain and heart - organs critical for survival, and, as it were, “deprives” those structures that are currently not needed for survival (liver, stomach, muscles, etc.).
If acute hypoxia is eliminated without depleting the body's reserves, then the person will survive, and all his organs and systems will function completely normally after some time. If hypoxia continues longer than the period of effectiveness of compensatory reactions, then irreversible changes will occur in organs and tissues.
Compensatory reactions during chronic hypoxia develop against the background of severe long-term diseases or conditions. First, to compensate for oxygen deficiency, the number of red blood cells in the blood increases, which allows the volume of oxygen carried by the same volume of blood per unit time to increase. Also, in red blood cells, the activity of an enzyme increases, facilitating the transfer of oxygen from hemoglobin directly to the cells of organs and tissues. New alveoli are formed in the lungs, breathing deepens, the volume of the chest increases, additional vessels are formed in the lung tissue, which improves the supply of oxygen to the blood from the surrounding atmosphere. The heart, which has to pump more blood per minute, hypertrophies and increases in size. Changes also occur in tissues - the number of mitochondria (organelles that use oxygen to ensure cellular respiration) increases in cells, and many new capillaries are formed in tissues. It is precisely because of the activation of microcirculation and a large number of capillaries during hypoxia that a person develops a pinkish coloration of the skin, which is mistaken for a “healthy” blush.
Adaptive reactions during acute hypoxia are reflexive, and therefore, when oxygen starvation is eliminated, they cease their effect, and the organs completely return to the mode of functioning in which they existed before the development of the episode of hypoxia. In chronic hypoxia, adaptive reactions are not reflexive; they develop due to the restructuring of the functioning mode of organs and systems, and therefore their action cannot be quickly stopped after oxygen starvation is eliminated.
With chronic hypoxia, the body can change its functioning mode in such a way that it completely adapts to conditions of oxygen deficiency and does not suffer from it at all. For example, this is how the body of residents of megacities adapts.
In acute hypoxia, complete adaptation to oxygen deficiency cannot occur, since the body simply does not have time to rearrange its functioning modes, and all its compensatory reactions are designed only to temporarily maintain the functioning of organs until adequate oxygen delivery is restored.
That is why a person can have a state of chronic hypoxia for many years without interfering with his normal life and work, while acute hypoxia in a short period of time can lead to death or irreversible damage to the brain or heart.
Compensatory reactions during hypoxia always lead to changes in the functioning of the most important organs and systems. These manifestations of compensatory reactions can be conditionally considered symptoms of hypoxia.
Why is it developing?
Doctors identify several main reasons for the development of hypoxemia, as well as a number of provoking conditions. Among the causes of lack of oxygen in the blood are:
- Atypical blood shunting - this situation can occur against the background of heart defects, when venous blood begins to flow into the aorta - in this case, hemoglobin loses its ability to attach oxygen.
- Problems with insufficient ventilation in the lungs - this happens when the frequency of exhalations and inhalations slows down, as a result of which, naturally, the supply of oxygen to the body decreases. Here they usually talk about a whole list of problems, including chest injuries, obstruction in the bronchi, inflammatory processes, such as pneumonia, collapse of part of the lung, etc.
- Anemia - when the level of hemoglobin decreases, the level of oxygen transported to the tissues begins to decrease.
- Diffusion disorders - due to increased physical activity, blood circulation begins to accelerate, as a result of which the amount of time required for hemoglobin to contact with oxygen decreases.
Also, a lack of oxygen in the blood can develop against the background of such a bad habit as smoking, with lung diseases, overweight and obesity, with changes in atmospheric pressure and with a decrease in the concentration of oxygen in the air.
How to measure blood oxygen levels at home? More details
Types of hypoxia
Hypoxia, depending on the mechanism of development, is divided into:
- Exogenous hypoxia (hypoxic hypoxia) is caused by environmental factors.
- Endogenous hypoxia is caused by various diseases or disorders that a person has:
- Respiratory (respiratory, pulmonary) hypoxia.
- Circulatory (cardiovascular) hypoxia: Ischemic; Stagnant.
- Hemic (blood) hypoxia: Anemic; Caused by inactivation of hemoglobin.
- Tissue (histotoxic) hypoxia. Substrate hypoxia.
- Overload hypoxia. Mixed hypoxia.
Depending on the speed of development and course:
- Lightning fast (instant) – develops within a few seconds (no longer than 2 – 3 minutes);
- Acute – develops within several tens of minutes or hours (no longer than 2 hours);
- Subacute – develops within several hours (no longer than 3-5 hours);
- Chronic – develops and lasts for weeks, months or years.
Depending on the prevalence of oxygen starvation , hypoxia is divided into general and local .
Exogenous hypoxia
Exogenous hypoxia (hypoxic) is caused by a decrease in the amount of oxygen in the inhaled air. Accordingly, blood leaves the lungs that is not sufficiently saturated with oxygen and a small amount of gas is brought to the cells of various organs/tissues. Exogenous hypoxia is manifested by cyanosis (blueness of the skin and mucous membranes), dizziness and fainting.
exogenous hypoxia normobaric
Depending on atmospheric pressure, exogenous hypoxia is divided into hypobaric and normobaric.
Hypobaric hypoxia is caused by low oxygen content in rarefied air with low atmospheric pressure. Such hypoxia develops in mountainous areas and at high altitudes.
Normobaric hypoxia develops when there is a low oxygen content in air with normal atmospheric pressure. Normobaric exogenous hypoxia can develop when being in mines, wells, on submarines, in diving suits, in cramped rooms with large crowds of people, with general air pollution or smog in cities, as well as during surgery if anesthesia-respiratory equipment malfunctions.
Respiratory (respiratory, pulmonary) hypoxia
respiratory hypoxia
Respiratory (respiratory, pulmonary) hypoxia develops in diseases of the respiratory system (bronchitis, pulmonary hypertension, any lung pathologies, etc.), when the penetration of oxygen from the air into the blood is difficult. Against the background of respiratory hypoxia, complications may develop, such as respiratory failure, cerebral edema and gas acidosis.
Circulatory (cardiovascular) hypoxia
circulatory hypoxia
Circulatory (cardiovascular) hypoxia develops against the background of various circulatory disorders (for example, decreased vascular tone, decreased total blood volume after blood loss or dehydration, increased blood viscosity, increased coagulability, centralization of blood circulation, venous stagnation, etc.). If a circulatory disorder affects the entire network of blood vessels, then systemic . If blood circulation is disrupted only in the area of an organ or tissue, then hypoxia is local .
During circulatory hypoxia, a normal amount of oxygen enters the blood through the lungs, but due to circulatory disorders, it is delivered to organs and tissues with a delay, as a result of which oxygen starvation occurs in the latter.
According to the mechanism of development, circulatory hypoxia is ischemic and stagnant. The ischemic form of hypoxia develops with a decrease in the volume of blood passing through organs or tissues per unit of time. This form of hypoxia can occur with left ventricular heart failure, heart attack, cardiosclerosis, shock, collapse, vasoconstriction of some organs and other situations.
The stagnant form of hypoxia develops when the speed of blood movement through the veins decreases - with thrombophlebitis of the legs, right ventricular heart failure, increased intrathoracic pressure and other situations when blood stagnation occurs in the venous bed. In the stagnant form of hypoxia, venous blood does not return to the lungs in time to remove carbon dioxide and saturate with oxygen. As a result, there is a delay in the delivery of the next portion of oxygen to organs and tissues.
Hemic (blood) hypoxia
Hemic (blood) hypoxia develops when quality characteristics are impaired or the amount of hemoglobin in the blood decreases. Hemic hypoxia is divided into two forms - anemic and caused by changes in hemoglobin quality .
hemic hypoxia
Anemic hemic hypoxia is caused by a decrease in the amount of hemoglobin in the blood, that is, anemia of any origin or hydremia (dilution of the blood due to fluid retention in the body). During anemic hypoxia, oxygen is normally bound and transported by the blood to organs and tissues. But due to the fact that there is too little hemoglobin, insufficient oxygen is brought to the tissues and hypoxia occurs in them.
Hypoxia, caused by a change in the quality of hemoglobin, is associated with poisoning by various toxic substances, which lead to the formation of forms of hemoglobin that are not capable of carrying oxygen (methemoglobin or carboxyhemoglobin). When the quality of hemoglobin changes, its quantity remains normal, but it loses its ability to carry oxygen. As a result, when passing through the lungs, hemoglobin is not saturated with oxygen and the blood flow does not deliver it to the cells of all organs and tissues. A change in the quality of hemoglobin occurs when poisoned by a number of chemicals, such as carbon monoxide (carbon monoxide), sulfur, nitrites, nitrates, etc.
Tissue (histotoxic) hypoxia
Tissue (histotoxic) hypoxia develops against the background of impaired ability of organ cells to absorb oxygen. The cause of tissue hypoxia is reduced activity or deficiency of mitochondrial respiratory chain enzymes, which convert oxygen into forms in which it is used by cells to carry out all life processes.
Disruption of respiratory chain enzymes can occur in the following cases:
- Suppression of the activity of respiratory chain enzymes in case of poisoning with cyanide, ether, urethane, barbiturates and alcohol;
- Lack of enzymes of the respiratory chain due to deficiency of vitamins B1, B2, PP and B5;
- Disruption of the enzymes of the respiratory chain due to poisoning with nitrates, microbial toxins, exposure to large amounts of thyroid hormones, etc.;
- Damage to the structure of enzymes due to exposure to radioactive radiation, uremia, cachexia, severe infectious diseases, etc.
Tissue hypoxia can exist for a long period of time.
Substrate hypoxia
substrate hypoxia
Substrate hypoxia develops with normal oxygen delivery to tissues, but in conditions of a lack of basic nutrients that undergo oxygen oxidation. Substrate hypoxia can develop during fasting, diabetes and other conditions when there is not enough glucose and fatty acids in the cells.
Overload hypoxia
overload hypoxia
Overload hypoxia can develop during heavy physical work, when cells intensively consume oxygen. In such cases, the cells simply do not have enough oxygen delivered. Such physiological hypoxia is not dangerous and goes away after completing the stage of high physical activity.
Mixed hypoxia
Mixed hypoxia is a combination of several types of endogenous hypoxia and occurs with severe, life-threatening lesions of various organs and systems, such as shock, poisoning, coma, etc.
Acute hypoxia
Acute hypoxia develops quickly, within several tens of minutes, and persists for a limited period of time, ending either with the elimination of oxygen starvation, or with irreversible changes in organs that will lead to severe illness or even death. Acute hypoxia usually accompanies acute conditions in which blood flow, quantity and quality of hemoglobin sharply change, such as, for example, blood loss, cyanide poisoning, heart attack, etc.
acute hypoxia
Any variant of acute hypoxia must be eliminated as soon as possible, since the body will be able to maintain the normal functioning of organs and tissues for a limited period of time until compensatory and adaptive reactions are exhausted. And when the compensatory-adaptive reactions are completely exhausted, the most important organs and tissues (primarily the brain and heart) will begin to die under the influence of hypoxia.
In principle, acute hypoxia is more dangerous than chronic hypoxia, since it can quickly lead to disability, organ failure or death. And chronic hypoxia can exist for years, giving the body the opportunity to adapt and live and function quite normally.
Chronic hypoxia
chronic hypoxia
Chronic hypoxia develops over several days, weeks, months or even years, and occurs with long-term diseases. The body adapts to chronic hypoxia by changing the structure of cells to new conditions, which allows organs to function quite normally. In principle, chronic hypoxia is safer than acute hypoxia, because develops slowly and the body is able to adapt to new conditions using compensation mechanisms.
Hypoxia: consequences, causes, signs, symptoms, treatment
Hypoxia (literal translation from Greek - “little oxygen”) is a state of oxygen starvation of the entire body and individual organs and tissues, caused by various external and internal factors.
Causes of hypoxia
- Hypoxic (exogenous) - with a decrease in the oxygen content in the inhaled air (stuffy, unventilated rooms, high altitude conditions, high-altitude flight without oxygen equipment);
- Respiratory (respiratory) - when there is a complete or partial violation of the movement of air in the lungs (example: suffocation, drowning, swelling of the bronchial mucosa, bronchospasm, pulmonary edema, pneumonia, etc.);
- Hemic (blood) - with a decrease in the oxygen capacity of the blood, i.e. when the blood loses the ability to attach oxygen to the hemoglobin of red blood cells (the main oxygen carrier). Most often occurs with carbon monoxide poisoning, with hemolysis of red blood cells, with anemia (anemia);
- Circulatory - in case of cardiovascular failure, when the movement of oxygen-enriched blood to tissues and organs is difficult or impossible (example: myocardial infarction, heart defects, vasculitis, vascular damage in diabetes, etc.);
- Histotoxic (tissue) - when the absorption of oxygen by the tissues of the body is impaired (example: some poisons and salts of heavy metals can block enzymes involved in “tissue respiration”);
- Overload - due to excessive functional load on an organ or tissue (example: excessive load on muscles during hard work, when the need for oxygen is higher than its actual flow into the tissue);
- Mixed - a combination of several of the above options.
Signs and symptoms of hypoxia, mechanisms of the body’s defense against hypoxia
Signs of hypoxia are very diverse and almost always depend on the degree of its severity, duration of exposure and the cause of its occurrence. We will present the most basic symptoms and explain their causes.
Hypoxia can be acute (develops within a few minutes, hours) from the onset of exposure to the causative factor, or it can be chronic (develops slowly, over several months or years).
Acute hypoxia has a more pronounced clinical picture and severe, rapidly developing consequences for the body, which may be irreversible. Chronic hypoxia because develops slowly, allows the patient’s body to adapt to it, so patients with severe respiratory failure due to chronic pulmonary diseases live for a long time without dramatic symptoms. At the same time, chronic hypoxia also leads to irreversible consequences.
Basic mechanisms of the body's defense against hypoxia
1) Increasing the breathing rate to increase the supply of oxygen to the lungs and its further transport by the blood. At first, breathing is frequent and deep, however, as the respiratory center is depleted, it becomes rare and superficial.
2) Increased heart rate, increased blood pressure and increased cardiac output. Thus, the body, experiencing oxygen starvation, tries to “distribute” as much oxygen as possible into the tissues as quickly as possible.
3) Release of deposited blood into the bloodstream and increased formation of red blood cells - to increase the number of oxygen carriers.
4) Slowing down the functioning of certain tissues, organs and systems in order to reduce oxygen consumption.
5) Transition to “alternative sources of energy”. Since there is not enough oxygen to fully meet the body’s energy needs, alternative sources of energy are launched to provide almost all processes occurring in the body. This defense mechanism is called anaerobic glycolysis, i.e. the breakdown of carbohydrates (the main source of energy that is released during their breakdown) without the participation of oxygen. However, the downside of this process is the accumulation of undesirable products such as lactic acid, as well as a shift in the acid-base balance to the acidic side (acidosis). Under conditions of acidosis, the full severity of hypoxia begins to manifest itself. Microcirculation in tissues is disrupted, breathing and blood circulation become ineffective, and ultimately, complete depletion of reserves occurs and breathing and blood circulation stop, i.e. death.
The above mechanisms during acute short-term hypoxia are quickly depleted, which leads to the death of the patient. In chronic hypoxia, they are able to function for a long time, compensating for oxygen starvation, but they bring constant suffering to the patient.
The central nervous system is primarily affected. The brain always receives 20% of the body's total oxygen, this is the so-called. “oxygen debt” of the body, which is explained by the colossal need of the brain for oxygen. Mild disorders caused by brain hypoxia include: headaches, drowsiness, lethargy, fatigue, and impaired concentration. Severe signs of hypoxia: disorientation in space, disturbances of consciousness up to coma, cerebral edema. Patients suffering from chronic hypoxia acquire severe personality disorders associated with the so-called. hypoxic encephalopathy.
Low oxygen content in tissues is manifested by their discoloration in a bluish color (cyanosis). Cyanosis can be diffuse (widespread), for example with bronchospasm. There is acrocyanosis - a bluish color of the fingers and nail plates, and there may be cyanosis of the nasolabial triangle. For example, in acute and chronic cardiac and respiratory failure.
Changes in the shape of the nails and distal phalanges of the fingers. With chronic hypoxia, the nails thicken and acquire a round shape reminiscent of “watch glasses”. The distal (ungual) phalanges of the fingers thicken, giving the fingers a “drumstick” appearance.
Diagnosis of hypoxia
In addition to the characteristic symptom complex described above, laboratory and instrumental research methods are used to diagnose hypoxia.
• Pulse oximetry is the easiest way to determine hypoxia. It is enough to put a pulse oximeter on your finger and in a few seconds the oxygen saturation (saturation) of the blood will be determined. Normally, this figure is not lower than 95%.
• Study of the gas composition and acid-base balance of arterial and venous blood. This type allows for a quantitative assessment of the main indicators of the body’s homeostasis: partial pressure of oxygen, carbon dioxide, blood pH, the state of the carbonate and bicarbonate buffer, etc.
• Study of exhaled air gases. For example, capnography, CO-metry, etc.
Treatment of hypoxia
Therapeutic measures should be aimed at eliminating the cause of hypoxia, combating oxygen deficiency, and correcting changes in the homeostasis system.
Sometimes, to combat hypoxia, simply ventilating the room or walking in the fresh air is enough. In cases of hypoxia, which is the result of diseases of the lungs, heart, blood or poisoning, more serious measures are required.
• Hypoxic (exogenous) - the use of oxygen equipment (oxygen devices, oxygen cartridges, oxygen pillows, etc.);
• Respiratory (respiratory) - the use of bronchodilators, antihypoxants, respiratory analeptics, etc., the use of oxygen concentrators or centralized oxygen supply, up to artificial ventilation. In chronic respiratory hypoxia, oxygen treatment becomes one of the main components;
• Hemic (blood) - blood transfusion, stimulation of hematopoiesis, oxygen treatment;
• Circulatory - corrective operations on the heart and (or) blood vessels, cardiac glycosides and other drugs with a cardiotropic effect. Anticoagulants, antiplatelet agents to improve microcirculation. In some cases, oxygen therapy is used.
• Histoxic (tissue) - antidotes for poisoning, artificial ventilation, drugs that improve oxygen utilization by tissues, hyperbaric oxygenation;
As can be seen from the above, oxygen treatment is used for almost all types of hypoxia: from breathing with a mixture of oxygen cartridges or an oxygen concentrator to artificial ventilation. In addition, to combat hypoxia, drugs are used to restore the acid-base balance in the blood, neuroprotectors and cardioprotectors.
Oxygen cartridges are a budget-friendly and convenient means of treating hypoxia. They do not require setup, special handling or maintenance skills, and are convenient to take with you. Below is a selection of the most popular oxygen tank models:
However, it is worth considering that oxygen cans have some disadvantages. Firstly, canisters tend to run out - on average, a nine-liter canister is enough for 70 - 100 breaths, and if long-term treatment is necessary, then a large supply will be needed. Secondly, if hypoxia is a concomitant effect of another disease, the cans will most likely be useless.
In such cases, oxygen concentrators have an undeniable advantage. These are devices that produce an oxygen-enriched mixture for breathing from the surrounding air. This oxygen therapy compensates for hypoxia, which leads to a decrease in shortness of breath and intoxication:
———————————————————————
The article was prepared by Vadim Mikhailovich Gershevich (thoracic surgeon, candidate of medical sciences).
Still have questions? Call us now on our toll-free line 8 (800) 100-75-76 and we will be happy to provide expert advice and answer all your questions.
Myocardial hypoxia
myocardial hypoxia
Myocardial hypoxia is one of the most dangerous diseases and is characterized by insufficient oxygen supply to the heart muscle.
This condition occurs when there is a sudden decrease in oxygen supply to the heart muscle. Cells do not have time to adapt to changed conditions. Metabolism continues in them, but it becomes incomplete, and under-oxidized metabolites accumulate. If hypoxia persists, cardiac muscle tissue dies.
Clinically, this condition is manifested by attacks of chest pain, increasing their duration and intensity. Subsequently, myocardial infarction develops - necrosis of the heart muscle with loss of its contractile function.
Myocardial hypoxia can be caused by the following reasons:
- low oxygen content in atmospheric air;
- diseases of the lungs with impaired gas exchange in them;
- decrease in the amount of blood flowing through the myocardium due to pathology of the coronary arteries;
- deterioration of the blood's ability to carry oxygen, for example, with carbon monoxide poisoning;
- disruption of oxygen utilization by the cells themselves, for example, in case of poisoning with cyanides and heavy metals.
How to identify the problem?
To identify heart problems, you should undergo a thorough examination by a specialist. He will take a medical history and conduct an examination. It is also recommended to use pulse oximetry to check the level of oxygen in the blood - today it is not a problem to carry it out even at home using a portable device. In addition, X-rays of the lungs and ultrasound of the heart are prescribed to exclude pathologies that can lead to a state of hypoxemia. It is recommended to take a blood test to check for a sufficient amount of hemoglobin and the absence of anemia.
How often should healthy people check their saturation? More details
Consequences of hypoxia
The consequences of hypoxia can be different and depend on the period of time during which oxygen starvation was eliminated and how long it lasted. If hypoxia was eliminated during a period when the compensatory mechanisms were not exhausted, then there will be no negative consequences; after some time, the organs and tissues will completely return to their normal mode of operation. But if hypoxia was eliminated during the period of decompensation, when compensatory mechanisms were exhausted, then the consequences depend on the duration of oxygen starvation. The longer the period of hypoxia against the background of decompensation of adaptive mechanisms, the stronger and deeper the damage to various organs and systems. Moreover, the longer hypoxia lasts, the more organs are damaged.
During hypoxia, the brain suffers the most, since it can withstand without oxygen for 3-4 minutes, and from the 5th minute necrosis will begin to form in the tissues. The heart muscle, kidneys and liver are able to tolerate a period of complete absence of oxygen for 30-40 minutes.
The consequences of hypoxia are always due to the fact that in cells, in the absence of oxygen, the process of oxygen-free oxidation of fats and glucose begins, which leads to the formation of lactic acid and other toxic metabolic products that accumulate and ultimately damage the cell membrane, leading to its death. When hypoxia lasts long enough from the toxic products of improper metabolism, a large number of cells in various organs die, forming entire areas of dead tissue. Such areas sharply worsen the functioning of the organ, which is manifested by corresponding symptoms, and in the future, even with the restoration of oxygen flow, will lead to a persistent deterioration in the functioning of the affected tissues.
The main consequences of hypoxia are always caused by disruption of the central nervous system, since it is the brain that suffers primarily from oxygen deficiency. Therefore, the consequences of hypoxia are often expressed in the development of a neuropsychiatric syndrome, including parkinsonism, psychosis and dementia. In 50-70% of cases, neuropsychiatric syndrome can be cured. In addition, a consequence of hypoxia is exercise intolerance, when with minimal exertion a person experiences palpitations, shortness of breath, weakness, headache, dizziness and pain in the heart area. Also, the consequences of hypoxia can be hemorrhages in various organs and fatty degeneration of muscle, myocardial and liver cells, which will lead to disruptions in their functioning with clinical symptoms of failure of one or another organ, which can no longer be eliminated in the future.
Hypoxia - causes
The causes of exogenous hypoxia may be the following factors:
- Thin atmosphere at altitude (mountain sickness, altitude sickness, pilot sickness);
- Being in tight spaces with large crowds of people;
- Being in mines, wells or in any enclosed spaces (for example, submarines, etc.) with no communication with the outside environment;
- Poor ventilation of premises;
- Working in diving suits or breathing through a gas mask;
- Severe air pollution or smog in the city of residence;
- Malfunction of anesthesia-respiratory equipment.
The causes of various types of endogenous hypoxia may be the following factors:
- Respiratory diseases (pneumonia, pneumothorax, hydrothorax, hemothorax, destruction of alveolar surfactant, pulmonary edema, pulmonary embolism, tracheitis, bronchitis, emphysema, sarcoidosis, asbestosis, bronchospasm, etc.);
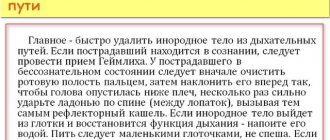
- Foreign bodies in the bronchi (for example, accidental swallowing of various objects by children, choking, etc.);
- Asphyxia of any origin (for example, due to compression of the neck, etc.);
- Congenital and acquired heart defects (non-closure of the foramen ovale or the duct of Batal, rheumatism, etc.);
- Damage to the respiratory center of the central nervous system due to injuries, tumors and other diseases of the brain, as well as when it is suppressed by toxic substances;
- Impaired breathing mechanics due to fractures and displacements of the chest bones, damage to the diaphragm or muscle spasms;
- Cardiac dysfunction caused by various heart diseases and pathologies (heart attack, cardiosclerosis, heart failure, electrolyte imbalance, cardiac tamponade, pericardial obliteration, blockade of electrical impulses in the heart, etc.);
- A sharp narrowing of blood vessels in various organs;
- Arteriovenous shunting (transfer of arterial blood into veins through vascular shunts before it reaches organs and tissues and releases oxygen to cells);
- Stagnation of blood in the inferior or superior vena cava system;
- Thrombosis;
- Poisoning with chemicals that cause the formation of inactive hemoglobin (for example, cyanide, carbon monoxide, lewisite, etc.);
- Anemia;
- Acute blood loss;
- Disseminated intravascular coagulation syndrome (DIC syndrome);
- Impaired metabolism of carbohydrates and fats (for example, diabetes, obesity, etc.);
- Shock and coma;
- Excessive physical activity;
- Malignant tumors of any location;
- Chronic kidney and blood diseases (for example, leukemia, anemia, etc.);
- Deficiency of vitamins PP, B1, B2 and B5;
- Thyroid diseases;
- Damage to cells by radiation, tissue breakdown products due to cachexia, severe infections or uremia;
- Drug and alcohol abuse;
- Prolonged fasting.
Symptoms (signs) of hypoxia
symptoms of hypoxia
In the fulminant form of hypoxia, clinical symptoms do not have time to appear, since death occurs within a very short period of time (up to 2 minutes).
The acute form of hypoxia lasts up to 2-3 hours, and during this period there is a failure of all organs and systems at once, primarily the central nervous system, respiration and heart (heart rate becomes less frequent, blood pressure drops, breathing becomes irregular, etc.). If hypoxia is not eliminated during this period, then organ failure progresses to coma and agony, followed by death.
Subacute and chronic forms of hypoxia are manifested by the so-called hypoxic syndrome. Against the background of hypoxic syndrome, symptoms from the central nervous system first appear, since the brain is most sensitive to oxygen deficiency, as a result of which foci of necrosis (dead areas), hemorrhages and other types of cell destruction quickly appear in its tissues. Due to necrosis, hemorrhage and death of brain cells against the background of oxygen deficiency at the initial stage of hypoxia, a person develops euphoria, he is in an excited state, and he is tormented by motor restlessness. One's own condition is not assessed critically.
With further progression of hypoxia, the following signs of depression of the cerebral cortex appear, which are similar in manifestations to alcohol intoxication:
- Drowsiness;
- Lethargy;
- Headache and dizziness;
- Noise in ears;
- Lethargy;
- Impaired consciousness;
- Involuntary passage of urine and feces;
- Nausea and vomiting;
- Movement coordination disorder;
- Cramps.
Convulsions during hypoxia appear when exposed to external stimuli. Moreover, a convulsive attack usually begins with twitching of the muscles of the face, hands and feet with the addition of random muscle contractions of the abdomen. Sometimes during convulsions opisthotonus , which represents a person arched with straightened neck and back muscles, head thrown back and arms bent at the elbows. The posture of a person in opisthotonus resembles the gymnastic figure “bridge”.
In addition to symptoms of depression of the cerebral cortex, a person also experiences pain in the heart area, irregular breathing, shortness of breath, a sharp decrease in vascular tone, tachycardia (an increase in heart rate of more than 70 beats per minute), a drop in blood pressure, cyanosis (blueness of the skin), decrease in body temperature. But when poisoned with substances that inactivate hemoglobin (for example, cyanides, nitrites, nitrates, carbon monoxide, etc.), human skin becomes pinkish in color.
With prolonged hypoxia with the slow development of damage to the central nervous system, a person may develop mental disorders in the form of delirium (“delirium tremens”), Korsakov’s syndrome (loss of orientation, amnesia, replacement of real events by fictitious events, etc.) and dementia.
With further progression of hypoxia, blood pressure drops to 20-40 mmHg. Art. and a coma occurs with loss of brain function. If blood pressure drops below 20 mmHg. Art., then death occurs. In the period before death, a person may experience agonizing breathing in the form of rare convulsive attempts to breathe.
How to recognize the problem?
Hypoxemia is represented by a number of symptoms that you should definitely pay attention to in order to consult a doctor in time. After all, a lack of oxygen can be an extremely dangerous condition that leads to an imbalance in the body as a whole.
So, hypoxemia will be indicated:
- increased heart rate and breathing;
- drowsiness;
- change in skin color towards pallor;
- weakness in general;
- dizziness.
If you ignore such signals from the body, later manifestations may develop, fraught with serious complications. For example, disruptions in the functioning of the heart, the development of severe swelling, problems with the functioning of the brain, as it does not receive enough nutrition. The skin may also take on a bluish tint. A person may experience anxiety, forgetfulness, and sleep problems. Potential complications include decreased blood pressure, stroke conditions, risks of developing pulmonary edema, convulsive effects, and heart rhythm disturbances.
Degrees of hypoxia
Depending on the severity and severity of oxygen deficiency, the following degrees of hypoxia are distinguished:
- Mild (usually detected only during physical activity);
- Moderate (phenomena of hypoxic syndrome appear at rest);
- Severe (the symptoms of hypoxic syndrome are strongly expressed and there is a tendency to transition to a coma);
- Critical (hypoxic syndrome has led to coma or shock, which can result in agony and death).
Treatment of oxygen starvation
In practice, mixed forms of hypoxia usually develop , as a result of which the treatment of oxygen deficiency in all cases should be comprehensive, aimed simultaneously at eliminating the causative factor and maintaining an adequate supply of oxygen to the cells of various organs and tissues.
To maintain a normal level of oxygen supply to cells in any type of hypoxia, hyperbaric oxygenation (HBO) - barotherapy - is used. In barotherapy, pressure chambers are used in which a person is under increased pressure with a high oxygen content. Due to the increased pressure, oxygen is additionally dissolved directly in the blood plasma, without contacting red blood cells, which allows its delivery to organs and tissues in the required quantity, regardless of the activity and functional usefulness of hemoglobin. Thanks to hyperbaric oxygenation, it is possible not only to supply organs with oxygen, but also to dilate the blood vessels of the brain and heart, so that the latter can work at full capacity.
In addition to hyperbaric oxygenation, cardiac drugs and drugs that increase blood pressure are used for circulatory hypoxia. If necessary, a blood transfusion is performed (if blood loss incompatible with life has occurred).
For hemic hypoxia, in addition to hyperbaric oxygenation, the following therapeutic measures are carried out:
- Blood or red blood cell transfusion;
- Introduction of oxygen carriers (Perftoran, etc.);
- Hemosorption and plasmapheresis to remove toxic metabolic products from the blood;
- Introduction of substances capable of performing the functions of enzymes of the respiratory chain (vitamin C, methylene blue, etc.);
- Introduction of glucose as the main substance that provides cells with energy to carry out vital processes;
- Administration of steroid hormones to eliminate severe oxygen starvation of tissues.
Prevention of hypoxia
Effective prevention of hypoxia is to avoid conditions in which the body may experience oxygen starvation. To do this, you need to lead an active lifestyle, be in the fresh air every day, exercise, eat well, and promptly treat existing chronic diseases. When working in an office, you need to periodically ventilate the room (at least 2-3 times during the working day) to saturate the air with oxygen and remove carbon dioxide from it.
prevention of hypoxia in a pressure chamber
It is also recommended to undergo a course of barotherapy (oxygen capsules and pressure chambers) several times a year, which helps reduce cases of oxygen starvation in the body.
Preventive actions
There are also a number of preventive measures that will reduce the risk of developing hypoxemia and prevent the development of serious complications. At the same time, they are quite simple and accessible to everyone. So, on the list of preventive measures:
- walks in the fresh air every day;
- physical activity, which should be moderate;
- practice breathing exercises (in consultation with a doctor);
- using vitamins and minerals in your diet;
- timely examinations by specialists to identify risks of developing cardiovascular and pulmonary diseases;
- rejection of bad habits.
Doctors note that hypoxemia is a preventable condition. The main thing is not to ignore signals from the body and correctly build your daily schedule.
There are contraindications, you should consult your doctor