The times of Hamlet, Rasputin and Cleopatra have long since sunk into oblivion, and the topic of acute poisoning does not lose its relevance to this day. More than 400 thousand become their victims every year on the planet. What is acute poisoning and why is it so important to know its symptoms?
Every year more and more toxic chemical compounds accumulate in the environment. Simply put, we come across potentially toxic substances every day and risk experiencing all the “delights” of the symptoms of poisoning through our own sad experience.
Tragedy can befall a person by an absurd accident or by accident - doctors call such poisoning unintentional. Unfortunately, there are also deliberate poisonings - they have long been used to settle accounts with one’s own life or get rid of competitors.
What poisonings are most common? What symptoms and signs indicate poisoning? How should first aid be provided? Let's try to figure it out...
A few words about poisons
According to scientists, any substance that enters the body can cause poisoning - after all, much depends not only on the concentration of the poison, but also on its quantity. Substances that are common and necessary for normal functioning of the body can become toxic in excessive quantities.
Under certain circumstances, even ordinary water can become dangerous: if you drink about 7 liters per day, you can get acute poisoning and even die from intoxication. Symptoms of water poisoning are associated with disruption of water and electrolyte metabolism in the body: swelling, cramps, vomiting, interruptions in heart function, diarrhea.
Toxic substances can enter the human body in all possible ways: through the mouth, skin, respiratory organs, by injection into the rectum, vein or ear canal. The severity of poisoning, symptoms and treatment, emergency measures to remove poison from the body depend on the type and amount of the toxic substance, and, of course, on the routes of its penetration.
The first symptoms of poisoning may appear immediately after the poison enters the body or within several hours or even days. First of all, the brain, liver, kidneys, and intestines are affected by toxic substances. These organs “give signals” - symptoms of poisoning that cannot be ignored!
Main signs of food intoxication
When pathogenic microflora multiply in the human body, intoxication of the body occurs. This manifests itself with pronounced symptoms. If against their background there is a significant deterioration in the condition, urgent measures must be taken. The first signs of food poisoning, in most cases, appear within 2-6 hours after dangerous microorganisms, along with low-quality or spoiled food, enter the body.
When intoxicated, severe weakness and increased body temperature are always noted. Sometimes indicators can reach critical values. Additionally, nausea and vomiting occur. Other symptoms depend on the type of toxin and the characteristics of the body. May be observed:
- Heartburn.
- Diarrhea.
- Heavy salivation
- Increased flatulence.
Against the background of weakness and malaise, aversion to food occurs and chills appear. In severe cases, there is a drop in blood pressure, clouding or loss of consciousness.
Alcohol poisoning
Symptoms most often occur in the morning. Many consider them a kind of “retribution” for a stormy evening. This condition is more often called a hangover rather than alcohol poisoning.
Symptoms depend on the concentration of ethyl alcohol in the blood. At the beginning of intoxication, this is euphoria and talkativeness, with an increase in alcohol concentration - impaired speech and coordination of movements. The liver begins the process of recycling alcohol into simpler substances, aldehyde, water, carbon dioxide. It is acetaldehyde that is “to blame” for morning ailments: headache, thirst, nausea, dry mouth, dizziness.
Be careful!
In order for alcohol poisoning to occur, an adult needs on average about 200 ml of 40% ethanol; alcohol poisoning in a child occurs when drinking 30 ml of 40% ethanol (vodka).
Food poisoning. Symptoms
Almost all food products pose potential dangers and health risks. In some products, the level of food additives - the so-called "yes" - is "off the charts", others are contaminated with pathogenic bacteria, and others were simply consumed unwashed. Food poisoning, unfortunately, is not uncommon these days. If the rules for preparing, processing, and storing food are not followed, food poisoning may occur.
Food poisoning in an adult (child) can be:
- microbial, that is, associated with pathogenic bacteria (salmonellosis);
- non-microbial - associated with poisons of animal or plant origin. For example, mushroom poisoning or poisoning with the Japanese delicacy - poisonous fugu fish.
Also, symptoms of food poisoning in adults occur when consuming foods containing pesticides and heavy metal salts.
By the way, poisoning from fish, seafood and caviar is far from rare, since the waters of the world’s oceans are polluted with salts of heavy metals and other man-made “chemicals”.
Food poisoning in an adult can be associated with banal laziness in preparing food at home and the habit of eating at various public catering establishments. Food poisoning in a child is most often associated with his “knowledge of the world”: often children put into their mouths everything that interests them as soon as their parents turn away.
The most common symptoms of food poisoning:
- nausea;
- vomiting of eaten food;
- diarrhea (diarrhea).
Mushroom poisoning also causes convulsions, hallucinations, jaundice, and pain in the right side.
When starting treatment at home, do not forget to rinse your stomach from poor-quality food and take Enterosgel sorbent, or better yet, do not take risks and consult a doctor!
How to deal with the consequences of food poisoning
metaprebiotics
diarrhea
digestive problems
microflora
microbiota
Food poisoning (intoxication) is a severe functional disorder of the gastrointestinal tract, which is provoked by pathogens and their metabolic products (toxins), as well as factors not related to pathogenic microflora. Food poisoning caused by consumption of low-quality and thermally unprocessed food of animal and plant origin is more common among the population. Not only any type of poisoning in the midst of an illness is dangerous, but also the consequences that a person faces after recovery.
Symptoms of food poisoning
The pathogenic microorganisms themselves, their metabolic products or other toxic substances, aggressively affect the gastrointestinal tract along its entire length. Food poisoning is accompanied by dehydration (dehydration), damage to the mucous membrane of the stomach and intestines, and an imbalance of intestinal microflora.
The following are common symptoms of food poisoning:
- nausea and vomiting;
- stool disorders in the form of diarrhea (the frequency of the urge to defecate and the consistency of stool depends on the severity of poisoning);
- pain in the umbilical, left or right iliac region;
- bitter taste in the mouth;
- muscle weakness;
- general malaise;
- pale skin;
- headache;
- increased body temperature;
- dyspnea;
- drowsiness.
Toxins released by pathogenic microorganisms negatively affect the thermoregulation center located in the hypothalamus. The result of this influence is chills and fever. Diarrhea due to food poisoning is profuse in nature. Diarrhea and vomiting lead to significant loss of body fluids and the development of dehydration. Dehydration or dehydration is accompanied by increased heart rate and increased blood pressure.
The first symptoms of intoxication become apparent within 24 hours from the moment pathogens and other toxic compounds enter the body. Depending on the severity of poisoning, body temperature can range from 37.3-40 degrees.
Classification of food poisoning
Foodborne illnesses are divided into 2 main groups:
- Microbial origin. Food intoxication of microbial origin develops when microorganisms of a bacterial or fungal nature enter the body with food. Poisoning can be caused by enterococci, staphylococci, botulinum bacillus, bicilli, vibrios, E. coli, aspergillus, microscopic fungi, and penicillium.
- Non-microbial origin. This type of toxic infection is triggered by natural poisons of both plant and animal origin. Such components are found in the core of apricot kernels, poisonous wild berries and mushrooms, some weeds, sprouted potatoes, burbot caviar, and mussels.
Also, food poisoning can develop when salts of heavy metals, pesticides, nitrosamines and cyclic hydrocarbons enter the body.
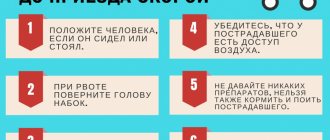
First aid for food poisoning
If symptoms of food poisoning occur, you must follow the following algorithm:
- A person should be given 3-5 glasses of clean water to drink, and then induce a gag reflex by pressing two fingers on the root of the tongue. The procedure should be repeated until the water coming out is clean.
- After cleansing the stomach, it is necessary to give the victim an enterosorbent 4 times in a row with an interval of 15 minutes.
- The patient should be wrapped up and ensure complete rest. In the first 24 hours, the victim must refrain from eating food.
Nutrition after poisoning
In order not to worsen your general condition, it is important to know what you can eat after poisoning and what it is better to avoid. It is recommended to start eating on the second day after poisoning. You should start with weak chicken broth, moving on to pureed rice soups. The diet includes weak black tea without sugar, day-old white bread, crackers and crackers, baked apples without sugar, semolina, oatmeal, buckwheat porridge with water, lean fish, steamed or boiled.
Exclude semi-finished products, fried and fatty foods, fatty meats and fish, fresh vegetables and fruits, confectionery, baked goods, sauces, seasonings, spices, and fast food from the diet. The food consumed should not create additional stress on the digestive system and should not provoke diarrhea or irritation of the gastrointestinal mucosa. After suffering a food poisoning, it is very important to take care of restoring the intestinal microflora, since in 75% of cases, intestinal dysbiosis develops after poisoning.
It will take a lot of time for the body to restore normal microflora on its own, and it will not be able to do this fully. The question arises of how to restore the intestinal microflora by resorting to outside help. Metaprebiotics are a real first aid for an organism weakened by food poisoning and its consequences.
Stimbifide Plus is a fundamentally new product , which contains fructopolysaccharides and fructooligosaccharides, as well as calcium lactate. Together, these components actively restore the balance of intestinal microflora, providing it with a natural nutrient substrate and preventing the proliferation of pathogenic microorganisms.
It has been clinically proven that even the best prebiotic among modern brands does not compete in terms of effectiveness with metaprebiotics. Metaprebiotic Stimbifid Plus not only prevents and treats dysbiosis after food poisoning, but also helps to carefully restore the epithelium of the gastrointestinal tract, which has been damaged by bacterial waste products and other toxic components.
In addition, for severe food poisoning, antibiotics may be prescribed. Stimbifid Plus will help avoid the consequences of antibiotic therapy. It is necessary to start taking the metaprebiotic as early as possible, and continue to take Stimbifide Plus for 1.5-2 weeks after the general condition has normalized.
14.09.2020
48832
18
/ Doctor Stimbifeed
If the article was useful to you, share it with your friends:
Poisoning with acids (alkalis)
Intoxication with these chemicals is possible through inhalation of vapors, contact with the skin or in the stomach.
Poisoning by acid vapors is manifested by burns of the mucous membranes, bleeding, dry cough, bloody vomiting, pain in the mouth and chest.
Poisoning by household chemical vapors is accompanied by headache, cough, abdominal pain, nausea, and an unpleasant taste in the mouth.
Redness of the eyes, burning, runny nose, headache, nausea - typical symptoms of poisoning with vapors of varnishes and paints and traditional companions of home repairs!
What types of toxic substances are poisoned and how do they affect the body?
What are they poisoning people with?
- Chemical warfare agents
Toxic substances are chemical compounds with a high degree of toxicity that are used as chemical weapons. Their special properties include the ability to be used to infect territory, food and military equipment, as well as to tactically defeat the enemy. These chemical compounds penetrate into the human body through the digestive tract, respiratory system, skin pores and mucous membranes.
Chemical weapons created on the basis of toxic substances (CA) were actively used during the First World War. The massive use of chemical warfare agents (CWA) has officially ceased since 1997, although behind the scenes research in this area continues. Data on new developments are under the control of intelligence services and rarely become publicly available. Among the chemical agents that have received publicity, the most dangerous are the drugs from the following list.
- Potently toxic substances
Potently toxic substances (STS) are chemical compounds used in the economy that are highly toxic and can, under certain conditions (mainly accidents at chemically hazardous facilities), cause mass poisoning of people and animals, as well as contaminate the environment. Currently, instead of the term SDYAV, the term Emergency Chemically Hazardous Substance (HAS) is used.
Main features of SDYAV:
- the ability to be carried over long distances in the direction of the wind, where it can cause injury to people;
- volumetric action, that is, the ability of contaminated air to penetrate unsealed rooms; a wide variety of SDYAVs, which creates difficulties in creating filter gas masks;
- the ability of many SDYAVs to have not only a direct effect, but also to infect people through water, products, and surrounding objects.
In the case of simultaneous contamination with two or more toxic agents, it can cause a combined effect on the body of several poisons. In this case, the toxic effect can be enhanced (synergism) or weakened (antagonism).
The most important characteristic of the danger of SDYAV is the relative density of their vapors (gases). If the vapor density of a substance is less than 1, this means that it is lighter than air and will dissipate quickly. The greatest danger is posed by SDYAV, the relative density of vapors of which is greater than 1, they remain at the surface of the earth longer (for example, chlorine), accumulate in various depressions in the area, and their impact on people will be longer.
Ways of influence of SDYAV on the human body:
- with food and water (oral);
- through the skin and mucous membranes (cutaneous-resorptive);
- by inhalation (inhalation).
- Poisons of plant and animal origin
Poisonous plants are those whose contact with or ingestion, even in small quantities, causes health problems.
Poisoning with plant poisons usually occurs as a result of eating fruits, leaves or roots of poisonous plants, which are unknowingly mistaken for edible. In this case, poisonings are most often accidental (children, tourists). The cause of poisoning may be the use of unknown plants for self-medication or violation of the conditions of cultivation and processing of raw materials. Many poisonous plants have a toxic effect on several organs and systems, but most of them are selectively toxic.
What could be the consequences of poisoning?
Chemical warfare agents:
Their effect on humans is usually divided into five groups: suffocating, irritating, tear-producing, generally toxic and skin-active.
Asphyxiating agents include phosgene, diphosgene, chlorine, and chloropicrin. Of these, the first two are the most important. Air containing asphyxiating substances, penetrating into the human respiratory organs, causes a disease, the degree of which depends on the amount of agent that has penetrated inside. The effect of chlorine and chloropicrin affects immediately: cough, suffocation, sputum production, chest pain, weakness. In severe cases, serious lung disease develops and fills with fluid.
Irritating agents - the most characteristic of them is adamsite - primarily affect the mucous membranes of the upper respiratory tract: nose, larynx, causing frequent and painful sneezing, profuse nasal discharge, pain in the chest, gums, salivation, vomiting. All this goes away after 23 hours if the affected person is taken out of the poisoned atmosphere and given help.
Tear-producing agents, such as chloroacetophenone, act primarily on the eyes, which become red, teary, and sore that it becomes impossible to see surrounding objects. But if you help the affected person, all these painful phenomena pass within an hour and subsequently disappear without a trace.
Commonly poisonous toxic substances are hydrocyanic acid and carbon monoxide, which, penetrating together with the inhaled air into the lungs and through the lungs into the blood, produce a generally poisonous effect on the body. Hydrocyanic acid acts especially quickly and severely, which immediately leads to loss of consciousness and convulsions. To prevent this serious injury, it is necessary to put on a gas mask as quickly as possible to prevent hydrocyanic acid from penetrating into the lungs. Those who have been burned experience a sharp headache, dizziness, nausea, vomiting, and in severe cases, they lose consciousness and stop breathing.
Skin agents, for example, mustard gas and others, affect any human organ, wherever they enter in a liquid or vapor state. Mustard gas vapors affect the eyes and lungs; liquid mustard gas, once on the skin, causes the formation of blisters within a few hours, under which ulcers then open.
Potently toxic substances:
There are the following symptoms of human poisoning:
- Burning sensation in the nasopharynx.
- Lack of air if the poison affects the respiratory and cardiovascular systems.
- A bitter taste in the mouth, which is accompanied in most cases of poisoning by excessive salivation.
- During intoxication, severe pain is observed in the epigastric zone, which may indicate inflammation of the pancreas.
- If you are poisoned by narcotic substances, convulsive seizures often occur, the skin acquires a bluish tint, and the pupils decrease in size.
The main symptomatic signs of poisoning and poison intoxication are nausea and vomiting, especially if the toxic substance penetrates the stomach. The first symptoms of poisoning may appear within 30 minutes, but sometimes more than a day may pass before signs of intoxication appear.
The main severe consequences are the following pathological conditions: Gradual death of liver tissue, internal bleeding, which causes death in the absence of timely medical care, cardiac arrest.
Poisons of plant and animal origin:
Ingestion of poisonous plants leads to the development of acute gastroenteritis and causes severe abdominal pain, nausea, vomiting, and diarrhea. These symptoms are nonspecific and are caused by a high content of various organic acids that irritate the mucous membrane of the stomach and intestines.
Due to rapid dehydration of the body, severe weakness, shortness of breath, and weakened cardiac activity may develop. This group includes plants containing saponin (black nightshade, sprouted potatoes, mustard).
Plants containing glycosides (digitalis, lily of the valley, adonis, oleander) primarily disrupt cardiac activity. Small doses of tincture from these plants stimulate the heart muscle and regulate the heart rate. Large doses lead to poisoning, rhythm disturbances, and fainting. Due to the destructive effect on the mucous membrane of the gastrointestinal tract, they can cause nausea, vomiting, and diarrhea.
The most unusual poisonings and how they were done
- Poisoning of Russian banker Ivan Kivelidi
Method: highly toxic poison applied to the landline telephone receiver in his office.
In 1995, Kivelidi's office was broken into and a poison of unknown origin was applied to the telephone receiver. During the telephone conversation, the earphone membrane of the handset vibrated and particles of a toxic substance fell on the businessman’s skin. However, secretary Kivelidi was the first to die, although she was only wiping dust in her office. Two days later he himself died, and a month and a half later the pathologist who performed the autopsy of the banker died.
- Francisca Ballesteros poisoning her family
Method: medications in certain combinations and proportions.
In 1990, Francisca Ballesteros poisoned her eight-month-old daughter with an alcoholism drug. 14 years later, by mixing sedatives available in the house, she poisoned her husband and eldest daughter. After their death, the woman tried to poison her son, but he managed to survive. She was sentenced to 84 years in prison on September 26, 2005.
- The case of former FSB lieutenant colonel Alexander Litvinenko
Method: radioactive polonium-210 mixed into tea. In November 2006, Alexander Litvinenko, a former lieutenant colonel of the FSB, who was the co-author of the book “The FSB Explodes Russia” and the author of the book “Lubyansk Criminal Group”, in which he accuses the Russian special services of organizing the bombings of residential buildings in Russia in 1999 and other terrorist attacks, dies in London. which, in his opinion, was the rise to power of Vladimir Putin.
As a result of the investigation, it was found that Litvinenko had mixed particles of the radioactive substance polonium into his tea. The amount of poison in his cup exceeded the average lethal dose by 200 times. 20 days later he died from radiation sickness.
- Poisoning of ex-President of Ukraine Viktor Yushchenko
Method: toxic substance dioxin mixed into food. In September 2004, Ukrainian presidential candidate Viktor Yushchenko attended two different dinners in one evening. The next day he felt ill - in his opinion, at one of the events he was poisoned with an unknown poison. The version of dioxin poisoning arose a week after Yushchenko developed facial asymmetry during treatment in an Austrian clinic - external signs of dioxin intoxication. The politician managed to survive, but his face remained forever covered with scars.
- Assassination of Kim Jong Nam
Method: handkerchief with nerve agent VX. On February 13, 2017, two girls approached the brother of the North Korean leader at a Malaysian airport. The first distracted him, and the second threw a scarf with poison over his face. 15 minutes after this, Kim Jong Nam died. The nerve agent VX is banned by the 1993 Chemical Weapons Convention.
- Murder of men by Elfriede Blauensteiner, nicknamed the Black Widow
Method: a combination of drugs to lower blood sugar and antidepressants.
Elfrida advertised in the newspaper looking for patients in need of care. Finding a wealthy client, the Black Widow poisoned him and appropriated the wealth for herself. Thus, the woman killed three men, after which she was caught and received a life sentence in 1997.
- Poisoning of former Prime Minister of Georgia Zurab Zhvania
Method: iron pentacarbonyl in the drink. On February 3, 2005, Zurab Zhvania was found dead in a rented Georgian apartment. The Georgian version says that the poisoning occurred due to a carbon monoxide leak. The unofficial version is that Zhvania was poisoned with the toxic substance iron pentacarbonyl. This substance consists of the components carbon monoxide and iron. One drop of it releases all the iron from the body and allows carbon monoxide to exhibit poisonous properties.
Today, August 20, it became known about the poisoning of politician Alexei Navalny. He was urgently hospitalized in Omsk and is now unconscious in intensive care. Navalny felt ill on a plane flying from Tomsk to Moscow, because of this the plane urgently landed in Omsk, said the press secretary of the founder of the Anti-Corruption Foundation (FBK) Kira Yarmysh.
Navalny has not yet been diagnosed, so it cannot be said that the politician was definitely poisoned. However, the media began to write about supposed variants of the substance that could cause such an effect. We are talking about sodium hydroxybutyrate.
The substance sodium hydroxybutyrate (sodium salt of γ-hydroxybutyric acid) is a synthetic salt and drug that is used for general anesthesia during surgical interventions, treatment of neuroses accompanied by sleep disorders and ophthalmological pathologies.
Previously, this drug was used exclusively for treatment, and in the harsh “anti-alcohol era”, those who liked to drink mixed the solution in the ampoule with vodka, since osibutyrate potentiated the effect of ethanol and to obtain the effect of intoxication it was necessary to drink a smaller dose. As a rule, sodium hydroxybutyrate poisoning occurs only after chronic long-term use, since in large doses the substance can cause vomiting.
Read also
Russian physicists have studied the conditions under which Newton's third law does not work
After the introduction of the Russian vaccine, 144 side effects were found in volunteers
Scientists have discovered the composition of an asteroid of unknown origin 'Oumuamua
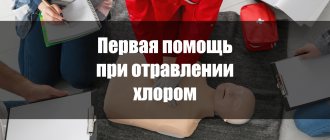
Chlorine poisoning. Symptoms
Chlorine compounds are used in everyday life to clean surfaces, disinfect pool water and bleach laundry. Since chlorine has become firmly established in our daily lives, it is important to know what symptoms of poisoning with chlorine-containing substances may bother victims.
Dry cough, choking, sore throat, drooling, watery eyes, vomiting - these are the signs of chlorine poisoning.
Depending on the severity of intoxication in the body, chlorine poisoning can be mild, moderate and severe. Poisoning in children of any degree can only be treated in a hospital!
After carrying out the first emergency measures (gastric lavage and taking Enterosgel sorbent), the victim is hospitalized for medical care.
What are food poisonings?
This concept includes all cases of ingestion of food products containing pathogenic microorganisms or their toxins, as well as any other toxic substances. Depending on the specific source of the disease, all food poisoning is briefly classified into three main types. Below is a diagram reflecting the main ones.
The diagram shows that all pathologies with an established etiology are divided into two main groups:
- microbial origin;
- non-microbial nature.
Also rare in medical practice, food poisoning of the third type occurs - with an unknown etiology. In other words, there is no exact information about the reason for their development.
An example of such a disease is Haffa disease. This is poisoning, accompanied by impaired kidney function and severe muscle pain, which can even limit the ability to move. This pathology occurs in residents of certain bodies of water, and its connection with fish such as pike perch, perch and pike has been proven. But scientists still cannot name the exact reason (specific conditions or substances) that provokes its development.
With the development of science and research methods, such food poisoning with an unknown etiology is becoming less and less common, but they still occur. Therefore, it is so important to strictly adhere to the principles of food hygiene, because still not all diseases have a clear algorithm for providing medical care.
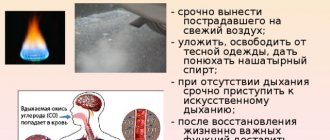
Carbon monoxide poisoning
Unfortunately, none of us is immune from carbon monoxide poisoning, because this substance is formed during combustion processes. Gas poisoning (CO) sometimes occurs in country houses due to faulty stove heating, in garages with poor ventilation, in fires and in hazardous industries.
Symptoms of carbon monoxide poisoning
The patient experiences drowsiness, headache, redness of the skin, chest pain, lacrimation, dry cough, and hallucinations. In severe cases, gas poisoning can cause fainting or complete loss of consciousness.
It is important to recognize these symptoms in time and start treatment at home in a timely manner! It is necessary to take the poisoned victim out of the room, provide access to fresh air and call an ambulance. To reduce the toxic effect of gas on the victim’s body, Enterosgel sorbent can be used.
Arsenic poisoning
Arsenic gets its name from its use in controlling rats and mice. Arsenic poisoning can result from an industrial accident, accidental ingestion, suicide, or homicide.
Symptoms of rat poison poisoning
- Heartbeat;
- Nausea;
- Dyspnea;
- Vomit;
- General weakness;
- Diarrhea;
- Convulsions;
- Loss of consciousness;
- Stomach ache.
Acute arsenic poisoning can result in acute renal failure. With chronic poisoning, nervous system disorders occur, skin cancer and lung cancer develop.
Publications in the media
Organophosphorus substances (hexaethyltetraphosphate, demeton, diazinon, dipterex [trichlorfon, chlorophos], malathion [karbofos], octamethylpyrophosphamide, parathion [thiophos], systox, tetraethylpyrophosphate, chlorthione, metaphos) are widely used in agriculture as insecticides, fungicides, herbicides, defoliants ; in everyday life - against domestic insects, for treating garden plots. Organophosphorus substances (OPS) also include some chemical warfare agents (nerve gases). Frequency. 5–10% of patients admitted to poison control centers. The predominant gender is male. Etiology and pathogenesis • Poisoning occurs when FOVs enter the body through the mouth, skin, respiratory tract • When entering through the mouth, absorption begins in the oral cavity and continues in the stomach and small intestine • FOVs quickly penetrate the bloodstream and are evenly distributed in organs and tissues (more high concentrations - in the kidneys, liver, lungs, intestines, central nervous system) • Poisoning can be acute and chronic (with prolonged contact with substances) • OPAs in the body are almost completely subject to metabolic transformations through various processes •• Oxidative processes take place in cell microsomes ( liver and other tissues) mixed-function oxidases. Recovery processes are especially active in the liver and kidneys with the participation of reductases in the presence of the coenzyme NADP. These transformations of OPA proceed according to the type of lethal synthesis (the resulting metabolites are many times more toxic than the original compound), which occurs primarily in the liver, so the oral route of entry of OPA poses the greatest danger • Enzymatic hydrolysis with the participation of hydrolases (phosphatases, carboxylesterases, carboxylamidases) is the main method of neutralization FOV • The leading link in the mechanism of action of most FOVs is inhibition (irreversible 4–5 hours after the onset of exposure) of the catalytic function of cholinesterase, leading to the accumulation of endogenous acetylcholine and continuous excitation of cholinoreactive systems (muscarinic and nicotine-like effects). FOVs also have a direct blocking effect on cholinergic receptors (curare-like effect) • Noncholinergic mechanisms of action (effects on proteolytic enzymes, the blood coagulation system, toxic effects on the liver, etc.) usually play an important role when small doses of FOVs are repeatedly introduced into the body • Pathomorphological changes • • Hydropic changes in the nerve cells of the cortex, the phenomenon of diffuse karyocytolysis in the cells of the cortex and subcortical formations •• Sharp changes in the vessels of the cortex and brain stem, alternation of dilated and spastically contracted areas •• Dystrophic changes in the myocardium, liver, kidneys.
Risk factors • Improper storage of FOV • Use of FOV for self-medication of skin diseases (head lice, scabies) • Alcoholism • Mental illnesses. Clinical picture of acute OPV poisoning • Main clinical symptoms • Miosis is one of the most characteristic signs of OPV intoxication. can serve as a criterion for the severity of the patient’s condition (in severe poisoning, pinpoint pupils persist for a long time, there is no reaction to light; miosis sometimes persists for several hours after death). Visual impairment (blurred vision, diplopia) •• Main types of mental disorders ••• Early asthenic syndrome - general weakness, headache, dizziness, inability to concentrate, anxiety (usually with mild or chronic poisoning) ••• Intoxication psychosis - severe psychomotor excitement, a feeling of panic, disorientation in time and surroundings ••• Coma - severe depression or lack of reaction of the pupils to light; inhibition of corneal reflexes, pain sensitivity; decreased muscle tone and tendon reflexes. Possible superficial coma with muscle hypertonicity, increased tendon reflexes •• Damage to the peripheral nervous system ••• Decreased muscle tone, muscle soreness on palpation ••• Hyperkinesis of the myoclonic type (fibrillary twitching) is the most characteristic symptom. In some cases, myofibrillations spread to the facial muscles, pectoralis major muscles, muscles of the upper and lower extremities; fibrillary twitching of the tongue muscles occurs in all cases of oral poisoning with OPA. The prevalence and frequency of myofibrillation correspond to the severity of poisoning ••• Choreic type hyperkinesis (wave-like muscle contractions) - in severe poisoning •• Respiratory disorders ••• Obstructive-aspiration form (in 80–85%) due to bronchorrhea. The secretion that foams during breathing clogs the airways and is released from the mouth and nose. The clinical picture resembles acute pulmonary edema, which can cause incorrect diagnosis and treatment ••• The central form is caused by dysfunction of the respiratory muscles: hypertonicity of the respiratory muscles and chest rigidity, then muscle paralysis •• Impaired cardiovascular functions ••• Early hypertensive syndrome due to severe hyperadrenalineemia (systolic pressure up to 200–250 mm Hg, diastolic pressure up to 150–160 mm Hg) ••• Severe bradycardia (up to 30 per minute), slowing of intraventricular conduction, AV block ••• B severe cases (exotoxic shock) - a sharp decrease in stroke volume of blood, bcc, drop in blood pressure, central venous pressure and peripheral vascular resistance, ventricular fibrillation •• Disorders of the gastrointestinal tract and liver ••• Severe spasm of the smooth muscles of the stomach and intestines (intestinal colic) can occur even with mild poisoning (when other symptoms of intoxication are mild), accompanied by nausea, vomiting, cramping abdominal pain, diarrhea ••• Impaired liver function, cholestasis. Patients with alcoholism may develop toxic hepatopathy.
• Stages of FOV poisoning •• Stage I—excitement (develops, as a rule, 15–20 minutes after the arrival of the toxic substance) ••• Dizziness, headache, decreased visual acuity; nausea, vomiting, cramping abdominal pain; feeling of fear, aggressive behavior ••• Objectively - moderate miosis, sweating, hypersalivation, slight bronchorrhea; Blood pressure is increased, moderate tachycardia •• Stage II - hyperkinesis and convulsions ••• Lethargy, stupor, in severe cases, coma. Hyperkinesis of choreic and myoclonic types (myofibrillation), most often in the face, chest and legs, in severe cases - fibrillation of almost all muscles of the body. Generalized epileptiform convulsions and tonic convulsions are possible; chest rigidity with a decrease in its excursion ••• Severe miosis, pupillary reaction to light is absent ••• Severe sweating, hypersalivation, bronchorrhea ••• Bradycardia or severe tachycardia. Severe hypertensive syndrome (BP increased to 240/160 mm Hg), then collapse ••• Painful tenesmus, involuntary loose stools •• Stage III - paralysis ••• Paralysis of skeletal muscles ••• Deep coma, usually with complete areflexia; miosis, hyperhidrosis are pronounced ••• The predominance of central forms of respiratory impairment, severe bradycardia or tachycardia (with ventricular fibrillation), a significant drop in blood pressure •• Relapse of intoxication (occurs 2–8 days after poisoning in 5–6%).
• The picture of poisoning as a whole depends little on the method of entry of the OPV into the body •• With inhalation and contact of the OPV with the eyes - long-term miosis •• With percutaneous entry - muscle fibrillations at the site of contact with the poison •• With ingestion - early onset of nausea, vomiting , acute abdominal pain, diarrhea and other dyspeptic disorders.
Chronic poisoning of OPV • Central nervous system - asthenia, decreased mental activity, emotional lability, decreased professional skills, especially when working requiring precise actions; less often - diencephalic syndrome • CVS - bradycardia, sinus arrhythmia, arterial hypotension • Peripheral nervous system - polyneuritis, radiculoneuritis • Impaired liver function, chronic gastritis • Allergic dermatitis (sometimes).
Laboratory studies • Determination of cholinesterase activity in whole blood, plasma, erythrocytes by potentiometric, photoelectrocolorimetric methods (according to the Hestrin method, the normal activity of cholinesterase in whole blood is 1.92–2.6 µmol) •• Usually the percentage of cholinesterase to the norm is used ••• The first symptoms of intoxication appear when the level of cholinesterase decreases by more than 30% ••• In severe poisoning, the indicator is reduced to 5–10% of the normal value •• Large individual fluctuations (±30%) of the normal activity of cholinesterase in whole blood should be taken into account, which significantly complicates diagnosis . • Determination of a toxic substance in blood, plasma, biological media by gas-liquid chromatography •• I stage of poisoning - concentrations of OPA in the blood are usually at the limit of detection (trace) •• II–III stage of poisoning - 0.5–29.6 mcg are determined in the blood /ml chlorophos, 0.1–3.0 µg/ml karbofos, up to 3.0 µg/ml metaphos. • Coagulogram - increased plasma tolerance to heparin, decreased recalcification time, decreased fibrinolytic activity (hypercoagulation). In the decompensated phase of shock with a sharp drop in blood pressure - hypocoagulation and fibrinolysis. Special research methods • ECG •• Sharp bradycardia (up to 20–40 per minute), widening of the QRS complex, slowing of intraventricular conduction, AV block, ventricular fibrillation •• In chronic poisoning: bradycardia, sinus arrhythmias, decreased voltage of the P wave, high wave T in the chest leads • On the chest x-ray - increased bronchovascular pattern.
Differential diagnosis • Pulmonary edema - in case of FOV poisoning, the appearance of foamy sputum from the mouth and nose is due to increased secretion of the bronchial glands, while, unlike pulmonary edema, the pressure in the pulmonary circle is reduced • Acute surgical diseases of the abdominal organs (with the development of intestinal colic) - it is necessary to identify other symptoms of FOV poisoning, clarify the anamnesis • Acute cerebrovascular accident (with the development of coma) - with FOV poisoning, as a rule, miosis and hyperhidrosis are noted, there are no focal neurological symptoms.
TREATMENT General recommendations • Hospitalization to a poison control center • In the absence of symptoms, but a decrease in cholinesterase activity, the patient should be observed in the hospital for at least 2-3 days; in order to avoid late manifestations of intoxication, specific therapy is prescribed with minimal doses of anticholinergic drugs and cholinesterase reactivators (reactivators - only in the first days after poisoning). Management tactics • When inhaling, the victim must be removed from the room with contaminated air. • If FOV gets on the skin and eyes, the affected areas are treated with alkaline solutions. • If ingested - gastric lavage through a tube followed by the introduction of a sorbent (activated carbon, petroleum jelly), emetics, high siphon enemas •• At stages II–III of poisoning, repeated gastric lavages are indicated at intervals of 4–6 hours until the smell of FOV disappears in lavage waters •• Gastric lavage and siphon enemas are done daily until the symptoms of poisoning are eliminated. • Specific antidote therapy. • Ensuring adequate ventilation of the lungs •• Oral toilet •• Tracheal intubation - in case of central respiratory failure, severe bronchorrhea (to remove secretions), coma (to prevent aspiration during gastric lavage) •• Lower tracheostomy - in case of severe bronchorrhea with disturbance breathing according to the central type (rigidity or paralysis of the chest) •• ALV - in case of breathing failure according to the central type. In case of hypertonicity of the chest muscles, mechanical ventilation is possible only after the administration of muscle relaxants •• Washing the bronchial tree (2% sodium bicarbonate solution or 0.9% sodium chloride solution with the addition of 500,000 units of penicillin) - in case of dryness of the bronchial mucous membranes due to the administration of large doses of atropine. • Subsequently - infusion therapy, forced diuresis. • Early hemosorption, peritoneal dialysis, hemodialysis •• Most FOVs quickly leave the vascular bed, depositing in tissues or hydrolyzing, so it is advisable to use these methods in the first hours from the moment of poisoning (primarily in case of poisoning with karbofos) •• Indications - severe poisoning, reduction cholinesterase activity by 50% or more •• Duration of hemodialysis - at least 7 hours •• Hemodialysis is also indicated for 2–3 days after hemosorption if cholinesterase activity is low and symptoms of poisoning persist (to remove from the body OPA metabolites that are not determined by laboratory methods). • If the cholinesterase content decreases by 30% or more and myocardial conductivity is impaired - transfusion of fresh donor blood •• Effective for 3-4 days after poisoning when treated with conservative methods •• After artificial detoxification, blood transfusion can be performed almost immediately after its completion. • Symptomatic therapy - elimination of severe respiratory and hemodynamic disorders, relief of seizures and psychomotor agitation, elimination of complications. Specific (antidote) therapy is aimed at blocking m-cholinergic receptors (for example, atropine), as well as restoring cholinesterase activity (cholinesterase reactivators, for example, oximes). • Atropinization •• Intensive atropinization is necessary for all patients from the first hour of treatment until all symptoms of the muscarinic-like action of FOV are relieved and signs of atropinization appear (dry skin and mucous membranes, moderate tachycardia, dilated pupils) ••• Stage I: 2–3 mg (2 –3 ml of 0.1% atropine solution) IV ••• Stage II: 20–25 mg (20–25 ml of 0.1% atropine solution) IV ••• Stage III: 30– 35 mg (30–35 ml of 0.1% atropine solution) IV •• Maintenance atropinization for the period of poison elimination (up to 2–4 days) ••• Stage I: 4–6 mg/day ••• II stage: 30–50 mg/day ••• Stage III: 100–150 mg/day. • Cholinesterase reagents are administered in parallel with intensive and maintenance atropinization during the first day from the moment of poisoning. Use at a later stage is ineffective and dangerous due to a pronounced toxic effect (impaired intracardiac conduction, relapse of acute symptoms of OPV poisoning, toxic hepatopathy) •• Trimedoxine bromide (a cholinesterase reactivator of predominantly peripheral action) ••• Stage I: 150 mg each (1 ml 15% solution) IM; total dose per course of treatment is 150–450 mg ••• stage II–III: 150 mg every 1–3 hours; total dose per course of treatment 1.2–2 g •• Dietixime (cholinesterase reactivator of central and peripheral action): initial dose 300–500 mg (3–5 ml of 10% solution) IM; if necessary, repeat 2-3 times with an interval of 3-4 hours (total dose - up to 5-6 g) •• Isonitrosine (a centrally acting cholinesterase reactivator) is used either alone or in combination with trimedoxine bromide, 1.2 g ( 3 ml of 40% solution) IM or IV; if necessary, the injections are repeated after 30-40 minutes (total dose - no more than 3-4 g). Isonitrosine is used in combination with trimedoxine bromide at stage II for severe disturbances of mental activity (lethargy, coma). • Specific therapy is carried out under constant monitoring of cholinesterase activity •• With effective treatment, cholinesterase activity begins to recover 2-3 days after poisoning and increases by the end of the week by 20-40%; the normal level is restored after 3–6 months •• With active methods of detoxification (hemosorption, hemodialysis), maintenance doses of anticholinergics and reactivators must be increased by 25–30%. Nonspecific drug therapy • Muscle relaxants - for hypertonicity of the chest muscles, which interferes with mechanical ventilation. The administration of listenone, which inhibits cholinesterase, is contraindicated • In acute cardiovascular failure - low molecular weight solutions, GCs (for example, hydrocortisone 250-300 mg), norepinephrine, dopamine • For the prevention of psychomotor agitation and convulsions - magnesium sulfate (25% solution 10 ml), chlorpromazine (2.5% solution 2–4 ml), diazepam (0.5% solution 2–4 ml) • For severe delirium and convulsive status - non-inhalational anesthesia, for example sodium oxybate ( 40–60 ml of 20% solution) • For various types of respiratory disorders, antibiotics are used to prevent pneumonia (for example, benzylpenicillin at least 10 million units/day) • The administration of morphine, cardiac glycosides, aminophylline is strictly contraindicated.
Complications • Pneumonia - as a result of severe breathing problems and microcirculation in the lungs; the main cause of death in patients in the late period of poisoning • Late intoxication psychoses usually have the character of alcoholic delirium (in alcohol abusers) with a complete disorder of consciousness, hallucinations, hyperthermia and neurological signs of cerebral edema • Polyneuritis - usually a few days after poisoning. Prognosis • Serious and depends on the amount of the toxic substance (the lethal dose of karbofos or chlorophos if ingested is about 5 g) and the timeliness of the assistance provided • In patients with symptoms of shock when poisoning with FOV, the mortality rate is approximately 60%. Reduction. OPA - organophosphorus substances
ICD-10 • T60.0 Toxic effects of organophosphorus and carbamate insecticides
Symptoms of mercury poisoning
Intoxication of the body with mercury compounds can be acute and chronic. Mercury vapor poisoning is possible in hazardous industries. Poisoning occurs when a fluorescent lamp is damaged, or mercury poisoning from a thermometer.
Symptoms that occur when inhaling mercury vapor include: drooling, dry cough, vomiting, headache and abdominal pain, and frequent urination. Poisoning in children often occurs due to parental negligence: remember, you cannot leave the first aid kit in a place accessible to the baby - this risks not only a broken thermometer, but also drug poisoning!
Chronic mercury intoxication causes depression, insomnia and other disorders of the central nervous system, skin rashes, sweating, and hair loss.
Thallium poisoning
Thallium is a highly toxic poison that enters the body through the skin, respiratory and digestive organs. Thallium poisoning is rare in everyday life; this poison is more often used for criminal purposes.
How many hours does it take for signs of poisoning to develop? Symptoms in adults occur within 3 hours and resemble an acute viral infection: runny nose, dry cough, diarrhea, vomiting, abdominal pain. Among the late manifestations of intoxication: hair loss, memory impairment, paralysis.
Main types of food poisoning
Food poisoning is caused by various bacteria. The most well-known pathological condition is dysentery. Its development is associated with the entry of the pathogenic Shigella bacillus into the human body. The disease always begins acutely. First of all, there is a sharp increase in body temperature to 39°C. This leads to the development of a feverish state accompanied by chills. Also, there is pain in the lower abdomen. They are paroxysmal in nature.
Additional signs of poisoning:
- Constant nausea and severe vomiting.
- Increased flatulence.
- Painful urge to defecate.
- Frequent diarrhea, characterized by loose, watery and scanty stools that may contain bloody inclusions.
Against the background of a general deterioration of the condition, there are risks of dehydration and a drop in blood pressure. You can become infected with dysentery if you do not follow the rules of personal hygiene.
A dangerous type of food poisoning is salmonellosis. It is caused by bacteria of the genus Salmonella. Features of the disease is the rapid development of an acute condition. It is characterized by:
A sharp increase in body temperature to high levels.
- Cramping pain in the abdomen.
- Severe vomiting.
- Frequent watery stools with foam and a specific odor.
Against the background of severe and rapid dehydration, there is a risk of dehydration shock and a decrease in blood pressure.
Poisoning in animals
Don’t think that only humans can get poisoned. “Our smaller brothers” often suffer from poisoning. The reason for this is the well-known hunting instinct, when a dog or cat conducts a “study” of new substances, testing them to their teeth.
- Symptoms of poisoning in cats and dogs arise from intoxication with various chemicals, poor quality food, medications, and insect bites;
- Symptoms of poisoning in dogs and other pets: lethargy, drooling, refusal to eat, vomiting, loss of coordination, diarrhea, dilated pupils, convulsions.
If signs of poisoning appear, contact your veterinarian!
First aid
If signs of intoxication appear, you must urgently call an ambulance. Before the arrival of specialists, it is necessary to rinse the stomach. To do this, a person must drink a large amount of warm, clean water or a weak chamomile decoction, after which vomiting should be provoked. It is also necessary to do an enema if possible. Be sure to buy and take absorbents after gastric lavage.
Because vomiting and diarrhea can lead to dehydration, you should drink plenty of fluids regularly once your condition has stabilized. These can be herbal teas without added sugar, compote or infusion of dried fruits, still mineral water. In severe cases, oral rehydration solution is prescribed for recovery.
In order to minimize the risks of food poisoning, it is important to strictly observe the rules of personal hygiene. It is imperative to wash your hands before eating, treat foods that are eaten raw with boiling water, and observe the shelf life of foods. At the slightest suspicion that the products have spoiled, they should be discarded.
Enterosgel and treatment of poisoning
The ability of carbon (coal) and silicon (clay) sorbents to absorb harmful substances has been known for a long time. Our ancestors intuitively understood that wounds heal better if they are sprinkled with ashes or covered with clay. Ashes and clay were used for stomach pain, fever and other illnesses.
However, the low absorbency and tablet forms of enterosorbents limited their medicinal properties until recently. The invention of Enterosgel, a new generation gel-like sorbent, at the end of the 20th century opened up additional opportunities for saving lives and treating patients with poisoning.
Enterosgel is especially effective for oral poisoning. Often, its timely use relieves all symptoms of food poisoning, since it absorbs and removes not only toxins, but also pathogenic bacteria, without disturbing the normal intestinal flora. Toxins do not have time to be absorbed into the blood, and bacteria do not have time to multiply and show aggression. Enterosgel removes from the gastrointestinal tract the products of secondary inflammation and intoxication that accompany poisoning with caustic substances.
No matter how the poison enters the body, it enters the intestinal lumen through the intestinal mucosa and is then reabsorbed. Therefore, Enterosgel is used for almost all types of acute poisoning.
Enterosgel is also used to prevent chronic poisoning in people employed in hazardous work.
Features of food poisoning
Very often, food poisoning is associated with eating poisonous mushrooms. The most dangerous is the toadstool. After consuming just a few grams, there are life-threatening risks. The danger of food poisoning from toadstool is that the clinical picture appears only after 12-24 hours. During this time, toxins enter the blood, which causes general intoxication of the body. In case of fly agaric poisoning, pronounced signs of food poisoning appear after 20-40 minutes.
In case of mushroom poisoning, in addition to the main symptoms, other dangerous manifestations may occur. This:
- Cramps.
- Muscle pain.
- Dyspnea.
- Hallucinations.
Food poisoning from dairy products is often recorded in the autumn and spring. They are the sources of potential infection if storage conditions are not observed. Low-quality dairy products in most cases become the cause of mass poisoning. Symptoms of intoxication in this case:
- Cramping pain in the abdomen.
- Stomach upset.
- Nausea and vomiting.