The speed of determining the signs of the development of a pathological condition and the timely delivery of the sick person to the nearest hospital depend on his chances of survival, recovery and return to his usual way of life. Cardiologists recommend carrying out initial measures within three hours - a longer period of time will activate irreversible consequences, leading to loss of ability to work and further disability.
What should be done first when a person has a stroke?
Advertising:
Wherever the stroke occurs and no matter what the stroke is, both the patient himself (if his condition allows) and those around him must act according to a clear algorithm:
- Do not panic!!!
- Assess the patient’s general condition: consciousness, breathing, heartbeat, blood pressure.
- Identify the obvious signs of a stroke: unilateral paralysis of an arm and leg, a distorted face, speech impairment, lack of consciousness, convulsions.
- Call an ambulance by calling 103!
- Find out the circumstances of the illness (briefly if possible).
- Provide resuscitation measures (artificial respiration, cardiac massage), but only if they are necessary (lack of breathing, heartbeat and dilated pupils).
- Position the patient correctly - on his back or side, either with his head and torso slightly elevated, or strictly horizontally.
- Provide conditions for good oxygen access to the lungs and blood circulation throughout the body.
- Monitor the patient's condition.
- Arrange transportation to the nearest hospital.
The emergency care described above is general and does not include some situations that are possible during a stroke. The sequence of events does not always have to be strictly the same as in the given algorithm. In case of critical impairment of the patient's condition, one has to act very quickly, performing several actions simultaneously. Therefore, if possible, 2-3 people should be involved in providing assistance. In any case, following the algorithm, you can save the patient’s life and improve the prognosis for recovery
Research needed to prevent stroke
To eliminate the risk of stroke, CITILAB recommends a special laboratory diagnostic program “Stop Stroke”. It allows you to specifically and reliably identify risk factors for the development of acute cerebrovascular accidents and assess the likelihood of their occurrence in the near future.
To the “Stop Stroke” program. Screening" includes:
- Complete blood count (CBC/Diff - 5 leukocyte fractions)
- Glycosylated hemoglobin (HBA1c)
- Creatinine
- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
- Profile “Lipid status”
- Extended coagulogram
Be healthy!
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
A detailed description of all emergency steps.
Each activity that includes first aid for a stroke requires proper execution. It is very important to adhere to subtleties, since any “little detail” can be fatal.
No fuss
No matter how serious the patient’s condition, do not panic or fuss. You must act quickly, harmoniously and consistently. Fear, fuss, haste, and unnecessary movements lengthen the time it takes to provide assistance.
Reassure the patient
Every conscious person with a stroke is definitely worried. After all, this disease is sudden, so the body’s stress reaction cannot be avoided. Anxiety will aggravate the condition of the brain. Try to reassure the patient, convince him that everything is not so scary, this happens and doctors will definitely help solve the problem.
Call an ambulance
Calling an ambulance is the first priority. Even the slightest suspicion of a stroke is an indication to call. Specialists will better understand the situation.
Call 103, tell the dispatcher what happened and where. It will take no more than a minute. While the ambulance is on the way, you will provide emergency care.
Assess your general condition
First of all, pay attention to:
- Consciousness: its complete absence or any degree of confusion (lethargy, drowsiness) is a sign of a severe stroke. Mild forms are not accompanied by impaired consciousness.
- Breathing: it may not be impaired, or it may be absent, intermittent, noisy, frequent or rare. Artificial respiration can be performed only in the complete absence of respiratory movements.
- Pulse and heartbeat: they can be clearly audible, rapid, arrhythmic or weakened. But only if they are not detected at all, you can do indirect cardiac massage
- Assess the patient's condition and determine the need for cardiopulmonary resuscitation
Identify the signs of a stroke
Stroke patients may have:
- severe headache, dizziness (ask what is bothering the person);
- short-term or persistent loss of consciousness;
- distorted face (ask him to smile, bare his teeth, stick out his tongue);
- impaired or lack of speech (ask to say something);
- weakness, numbness of the arms and legs on one side, or their complete immobility (ask them to raise their arms in front of you);
- visual impairment;
- impaired coordination of movements.
Lack of consciousness or any combination of these signs is a high probability of a stroke.
Correct position of the patient
Regardless of whether the consciousness and general condition of a stroke patient is impaired or not, he needs rest. Any movements, especially independent movement, are strictly prohibited. The position could be:
- On the back with the head and chest raised - with preserved consciousness.
- Horizontally on the side with the head turned to one side - in the absence of consciousness, vomiting, convulsions.
Correct position of the patient in the absence of consciousness
- Horizontally on the back with the head slightly thrown back or turned to the side - during transportation and resuscitation measures.
It is forbidden to turn a person on his stomach or lower his head below his body position!
If there are cramps
Convulsive syndrome in the form of severe tension of the whole body or periodic twitching of the limbs is a sign of a severe stroke. What to do with the patient in this case:
- Lay on your side with your head turned to prevent saliva and vomit from entering your respiratory tract.
- If you can, place any object wrapped in cloth between the jaws. It is rarely possible to do this, so do not make much effort - it will do more harm than good. Do not try to push the jaws apart with your fingers - this is impossible. Better grab the corners of the lower jaw, try to bring it forward. Do not insert your fingers into the patient's mouth (risk of injury and loss of a finger).
- Keep the patient in this position until the convulsions end. Be prepared for the possibility that they may happen again.
On the importance of the circumstances of the disease
If possible, find out exactly how the person got sick. This is very important, since some symptoms of stroke can also be observed in other diseases:
- traumatic brain injury;
- diabetes mellitus;
- brain tumors;
- poisoning with alcohol or other toxic substances.
Resuscitation: conditions and rules
Advertising:
An extremely severe stroke, affecting vital centers, or accompanied by severe cerebral edema, occurs with signs of clinical death:
- complete lack of breathing;
- dilation of the pupils of both eyes (if only one pupil is dilated - a sign of a stroke or hemorrhage in the hemisphere on the affected side);
- complete absence of cardiac activity.
Follow these steps:
- Place the person on their back on a hard surface.
- Turn your head to the side, use your fingers to free the oral cavity from mucus and foreign objects (dentures, blood clots).
- Throw your head back well.
- Grab the corners of the lower jaw with 2–5 fingers of both hands, pushing it forward, while using your thumbs to slightly open the patient’s mouth.
- Artificial respiration: cover the patient’s lips with any cloth, and, pressing your lips tightly, take two deep breaths (mouth-to-mouth method).
- Heart massage: Place your right hand on top of your left (or vice versa), interlocking your fingers. Applying your lower palm to the junction of the lower and middle parts of the patient's sternum, apply pressure to the chest (about 100 per minute). Every 30 movements should alternate with 2 breaths of artificial respiration.
What medications can be given for a stroke?
If an ambulance is called immediately after a stroke occurs, it is not recommended to give the patient any medications on your own. If delivery to the hospital is delayed, the following drugs (preferably in the form of intravenous injections) help support brain cells at home:
- Piracetam, Thiocetam, Nootropil;
- Actovegin, Ceraxon, Cortexin;
- Furosemide, Lasix;
- L-lysine escinate.
Self-help for stroke
The ability to help yourself with a stroke is limited. In 80–85% of cases, a stroke occurs suddenly, manifested by a sharp deterioration in condition or loss of consciousness. Therefore, patients cannot help themselves. If you experience stroke-like symptoms:
- take a horizontal position with the head end raised;
- tell someone you feel bad;
- call an ambulance (103);
- adhere to strict bed rest, do not worry and do not move excessively;
- release the chest and neck from constricting objects.
Helping yourself if you have a stroke
Signs of stroke in women and men
In terms of incidence, stroke remains second only to cancer. In addition, it is a common cause of disability.
A little about the terms:
- A stroke is a sudden disruption of blood flow in the brain or spinal cord.
- A microstroke (correctly, a transient ischemic attack) is a disruption of blood flow due to a spasm or a general decrease in blood flow, lasting no more than three hours.
On the first day, it is impossible to distinguish between the symptoms of a stroke and a microstroke without special examinations.
There are no fundamental differences in the signs of stroke in women and men. Manifestations usually appear suddenly.
The main first signs of a stroke are as follows:
- weakness or awkwardness in an arm or leg on one side;
- numbness in the limbs on one side;
- impaired speech understanding;
- difficulty pronouncing words and composing sentences;
- dizziness;
- loss of balance;
- unsteady gait;
- difficulties in performing habitual movements (lighting a match, picking up a cup);
- headache of varying intensity;
- seizures;
- numbness of half the face, lip or tongue;
- smoothing the nasolabial fold on one side;
- loss of consciousness;
- vomit.
A sign of the onset of a stroke may also be one of these symptoms.
External signs of a stroke can vary. If you suspect a violation of cerebral blood flow, you can ask the person to perform a few simple tests:
- smile;
- close your eyes tightly;
- stick out tongue;
- say a simple tongue twister (Karl stole corals from Clara);
- extend your arms in front of you;
- take several steps along one line.
If any test shows abnormalities, even doubtful ones, you should seek medical help immediately. Early signs of a stroke can be vague, and only a full examination reveals the scale of the problem.
If the stroke is hemorrhagic
Symptoms that speak in favor of hemorrhagic stroke:
- arose abruptly at the height of physical or psycho-emotional stress;
- there is no consciousness;
- have convulsions;
- the neck muscles are tense, it is impossible to bend the head;
- high blood pressure.
In addition to standard care, such patients need:
- The position is strictly with the head end elevated (except for convulsions or resuscitation).
- Applying an ice pack to the head (preferably to the half in which hemorrhage is suspected - opposite to the immobilized tense limbs).
Focal symptoms
1. Unilateral (right or left) motor disorders in the limbs in the form of paresis (decreased muscle strength) or paralysis (complete lack of movement in the limb) are the most common symptoms of stroke. Test. You can identify paresis in the following way: ask the patient to hold his arms outstretched forward for a few seconds; the affected arm will drop faster. In case of complete paralysis, the patient will not be able to hold his hand in front of him at all.
2. Speech disorders (dysarthria, aphasia). In the case of aphasia, both the understanding of addressed speech (the patient will not comply with requests and commands) and his own speech production may be impaired - the patient cannot construct his own speech. Dysarthria is manifested by unclear, “blurred” speech, there is a feeling of “porridge in the mouth”, the patient’s perception of the addressed speech does not suffer. Test. To identify the presence of speech disorders, ask the patient to say his name or say a simple phrase.
3. Facial asymmetry (smoothness of the nasolabial fold). Test. It is necessary to ask the patient to smile or show teeth and gums.
4. Unilateral (in the arm and/or leg) sensitivity disorders (hypoesthesia) – there is a feeling as if the patient was “lying down” on his limb; he may not feel touching it. Test. To identify sensory disorders, it is necessary to apply injections to symmetrical areas of the limbs on the right and left. If there are sensory disorders, the patient will not feel the injections on one side or feel them significantly weakened.
5. Oculomotor disorders. Paresis of gaze to the side may occur (restriction of movements of the eyeballs), up to a forced tonic rotation of the eyeballs. An ominous symptom is anisocoria (different pupil sizes), which usually occurs due to dislocation of the brain (in this case, due to superior - temporotentorial - herniation). Test. To check gaze paresis, it is necessary to ask the patient to follow an object moving horizontally and illuminate the pupils with a flashlight to compare their sizes and photoreaction.
6. With a stroke, there may be other focal symptoms - hemianopsia (loss of half the visual fields), dysphagia (swallowing disorders) and others.
Features of providing assistance on the street
If a stroke occurs on the street, first aid has the following features:
- Involve several people to help. Organize the actions of each of them, clearly distributing responsibilities (someone calls an ambulance, and someone assesses the general condition, etc.).
- Having placed the patient in the desired position, free the neck and chest to make it easier for him to breathe (remove the tie, unfasten the buttons, loosen the belt).
- Wrap up the limbs, cover the person with warm clothes (in cold weather), massage and rub them.
- If you have a mobile phone or contacts with relatives, inform them about what happened.
General cerebral symptoms
This group of symptoms includes: disturbances in the level of consciousness, headache, nausea, vomiting, dizziness, convulsions. General cerebral symptoms are characteristic signs of increased intracranial pressure with subarachnoid or intracerebral hemorrhage, extensive cerebral infarction.
Criteria for clear consciousness:
the patient is awake, correctly assesses the environment, is oriented in time, place, situation and his own personality.
There are quantitative (unproductive) and qualitative (productive) forms of disturbance of the level of consciousness.
Quantitative (“depression of consciousness”) forms include: stunning
(superficial and deep),
stupor, coma
(first, second and third degree). Currently, it is generally accepted to use assessments of the degree of depression of consciousness - the Glasgow scale.
Stunning (moderate, deep) - characterized by impaired attention, loss of coherence of thoughts or actions. When stunned, the patient is awake, but he is lethargic, drowsy, quickly becomes exhausted and falls asleep.
Stupor - the patient opens his eyes only after exposure to a strong stimulus (loud sound, pain, strong smell, etc.) The reaction to verbal instructions is weak or absent, there is no speech production. At the same time, targeted and local defensive reactions remain intact.
Coma is a complete loss of consciousness; we cannot awaken the patient. Superficial coma (first degree) - it is impossible to wake the patient, he reacts to painful stimuli with simple, erratic movements, there is no opening of the eyes to any irritation. Vital functions are not depressed.
Deep coma (second degree) - the patient does not respond with motor reactions to painful stimuli. Most reflexes are suppressed, but breathing and hemodynamics are still not there.
Atonic coma (third degree) is the complete absence of the patient’s response even to very strong painful stimulation. Muscle atony, areflexia, impaired or absent breathing, depression of cardiac activity may be observed.
Qualitative changes in consciousness consist in the fact that the patient is awake, but productive contact with him is difficult or impossible due to severe psychotic disorders. Examples of such conditions are dementia, delirium, twilight state of consciousness and a number of others. Psychomotor agitation is often observed.
Headache is most typical for hemorrhagic forms of stroke. For example, with subarachnoid hemorrhage, the headache is very intense, unusual in nature, appears like a “blow” to the head, and there may be a feeling of heat, pulsation, or a hot wave inside the head.
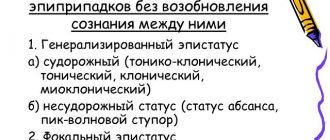
Convulsive seizures (tonic, tonic-clonic, clonic-tonic, generalized or local) are often observed at the onset of a stroke (primarily hemorrhagic).
Dizziness, nausea, and vomiting are not symptoms specific to acute stroke, but are often the leading reason for seeking medical help at “03” services or a clinic. In addition, like other general cerebral symptoms, they indicate the need for emergency symptomatic therapy.
Features of providing assistance at home or in any enclosed space
If a stroke occurs indoors (at home, in an office, in a store, etc.), then in addition to standard first aid, pay attention to:
- Free access of fresh air to the patient: open the window, door.
- Release your chest and neck.
- If possible, measure your blood pressure. If it is elevated (more than 150/90 - 160/100 mmHg), you can give antihypertensive drugs under the tongue (Captopress, Farmadipin, Metoprolol), lightly press on the solar plexus or on closed eyes. If it is low, raise your legs, but do not lower your head, massage the area of the carotid arteries on the sides of the neck.
How to provide first aid for a stroke indoors
What to do before the ambulance arrives?
Don't just stand there until the ambulance arrives. First of all, you need to put the person on a flat surface in a horizontal position. If a person has fallen, then you just need to give him a more comfortable position. It is important to control your breathing. If it is completely absent, place the person on his side, clean the oral cavity of food debris, vomit or dentures. They can be a barrier to normal breathing. To make breathing easier, you also need to unbutton your blouse or other tight items. It is advisable to loosen the belt. Open a window and allow fresh air to flow.
what to do before the ambulance arrives
If you have a tonometer at hand, you should immediately measure your blood pressure and record the readings. With high pressure, you need to raise your head, and with low pressure, you need to raise your legs. If a person has convulsions, under no circumstances should you try to restrain the person. Just put something soft under your head to avoid injuring your head. The only thing worth doing at the end of a seizure is to turn the person on his side.
It is strictly forbidden to unclench your jaw, try to insert any objects into your mouth, or fix your tongue. Such actions will only lead to harm to the person providing assistance. You should not worry about asphyxia through tongue swallowing; this is not possible during a convulsion.
If breathing and heartbeat stop, CPR should be started immediately. All resuscitation actions must be performed until the ambulance arrives.
First aid effectiveness and prognosis
According to statistics, correctly provided emergency care for stroke patients with delivery to a medical facility within the first three hours:
- saves the lives of 50–60% of patients with severe massive strokes;
- in 75–90% it allows people with minor strokes to fully recover;
- improves the recovery abilities of brain cells by 60–70% in case of any stroke (better in case of ischemic stroke).
Remember that a stroke can happen to anyone at any time. Get ready to take the first step to help fight this disease!
Types and causes of stroke
- Ischemic - vascular spasm causes disruption of normal blood circulation.
- Hemorrhagic - rupture of blood vessels leads to hemorrhage in the brain.
Ischemic stroke occurs most often. People over 65 years of age and women during menopause are susceptible to it. Recently, it has also often been registered in people at a relatively active, young age - 35-40 years old, especially in those who are engaged in intellectual work.
The main cause of stroke is arterial hypertension. Risk factors also include atherosclerosis, coronary heart disease, diabetes mellitus, and excess weight. In women, smoking while taking contraceptives.
Ischemic and hemorrhagic stroke
The sooner a person receives the right help, the less irreversible damage occurs in the nervous tissue. During an ischemic stroke, the so-called “ischemic penumbra zone” is formed - the penumbra - these are living cells that suffer from a lack of nutrients, but retain the ability to absorb them. It is precisely because of the gradual death of neurons that Neuron
A nerve cell consisting of a body and processes extending from it.
Structural unit of the nervous system. in this area, the area of damage in the brain can expand over time. The penumbra zone is the main goal of neuroprotective treatment. Neuroprotective treatment
is aimed at increasing the survival of nerve cells in adverse conditions, which helps to protect and restore the normal functioning and nutrition of neurons.
Therefore, the first signs of ischemic stroke are already a reason to start neuroprotective therapy.
Hemorrhagic stroke often has more severe and life-threatening consequences. The mechanism of damage in this case is the complex effect of the pressure of the spilled blood on the nervous tissue due to the resulting vascular spasm. With hemorrhagic strokes, irreversible damage to brain cells occurs more often and faster. But the use of neuroprotective medications can still help reduce the severity of nerve tissue damage.