A thermal burn is a specific injury to the skin and (sometimes) underlying tissue due to exposure to high temperatures. Sources of thermal effects can be both solids and liquids, as well as steam or gas. As a rule, contact with a carrier of excess heat occurs as a result of a violation of safety standards for working with its sources or as a result of an accident. Sunburns should also be partially classified as thermal. They arise due to the combined effect on the skin and mucous membranes of both ultraviolet rays, which themselves have a destructive effect on the body, and the thermal energy of solar radiation.
When exposed to thermal energy, the body primarily injures the skin (or mucous membranes). If the intensity of the thermal effect is high, then the injury can affect not only all layers of the skin, but also the tissues located underneath it. Depending on the depth of tissue damage, in clinical practice there are 4 degrees of burns, each of which has its own symptoms and clinical features, on the basis of which the treatment program is based. Therefore, before moving on to considering the treatment of thermal burns, you should familiarize yourself with them.
What is a thermal burn and how does it manifest itself?
Prolonged exposure to high temperatures on the skin causes burns. The greatest danger is thermal burns from water, hot objects, fire, steam and various types of gases under pressure. The consequences depend on the area affected and the general health of the person. It wouldn’t hurt for everyone to know what first aid is for a thermal burn, in order to, if necessary, alleviate the condition of the victim before emergency help arrives, and sometimes even save a life.
Most often, thermal burns occur from contact of the body with a hot object. Skin lesions can be superficial or very deep, characterized by tissue redness and swelling. In severe cases, internal organs are affected. Home treatment is allowed in the following cases:
- first degree burn, when there are no blisters, and therefore deep tissues are not damaged;
- the size of the damage is no larger than the palm of your hand;
- there are no lesions on the feet, hands, or face;
- there is no suppuration or inflammation in the burned area.
Possible complications of a thermal burn:
- sepsis (when more than 20% of the body surface is damaged);
- pneumonia;
- secondary infection in the form of gangrene, abscess.
What is a thermal burn?
Thermal burn
is a burn that is caused by contact with a liquid, solid or gaseous heat source. Such a heat source can be hot bodies, flames, steam, or hot liquids. The first place in statistics is occupied by flame burns (about 84% of all thermal burns), followed by burns with liquid substances and electrical burns (approximately 7% for each type). In 2% of victims, burns were caused by other factors.
A thermal burn can damage several layers of skin at once: epidermis (outer layer), dermis, subcutaneous tissue. Depending on the number of damaged layers, four degrees of thermal burns are distinguished. Often a burn includes all these degrees at the same time. Many doctors, when describing burns, classify them according to the depth of the damage: superficial, partial, complete.
The severity of the burn also depends on the area of the affected tissue. It is expressed as a percentage relative to the area of the entire surface of the skin. When roughly assessing a burn, the so-called “palm rule” is used: the area of the human palm is equal to one percent of the body area.
Degrees of thermal burns
It is customary to distinguish four degrees of burns depending on the depth and severity of the injury. Burns of the 1st and 2nd degrees are considered superficial, 3rd and 4th - deep.
- First degree thermal burn
The affected area swells and turns red. A person is disturbed by pain and burning, especially acutely felt when touched. The skin temperature in the affected area increases. The listed symptoms last for 2, sometimes 3 days, gradually disappearing. The burn site continues to disturb the victim for some time; the epidermis begins to peel off. Gradually (after 3-5 days) the injured area looks almost healthy. - Thermal burn of the second degree
This burn occurs due to prolonged or sudden exposure to high temperature. There is also redness and swelling of the tissues, but blisters also form. They are filled with tissue fluid exuding from dilated skin vessels. Later, the contents of the blisters, due to protein coagulation, turn from a transparent mass into a jelly-like mass containing leukocytes. The tissue fluid and the skin of the blisters themselves protect the tissues located under the lesion from injury and infection; for this reason, the blisters cannot be opened. Patients with a second degree burn typically suffer from severe pain. But after a few days, tissue irritation and circulatory disturbance begin to decrease, and the liquid is gradually absorbed. At the bottom of the blisters, epidermal cells are actively dividing, and after a week a new stratum corneum begins to appear. - Third degree thermal burn
It occurs during prolonged exposure to high temperature. It is characterized by skin necrosis - tissue necrosis, which can be dry or wet. When tissue is exposed to steam or boiling water, wet necrosis usually occurs. The skin becomes swollen, pasty, acquires a yellowish tint, and may become covered with blisters. This inflammation occurs in a manner similar to the melting of dead tissue. When necrosis is dry, the skin is also dry, dense, dark brown or black. The edges of the area with dead tissue are clearly visible. Healing of burns of this degree occurs through scarring. However, when at least small areas of the germ layer of the epithelium are preserved, epithelization cannot be ruled out. - IV degree thermal burn
This is, without exaggeration, the most terrible degree of burns. Often such burns cover a large area. All layers of the skin and even tissues located outside it die: subcutaneous fat, tendons, muscles, bones. Several large blisters often merge into one huge one; the skin color becomes dark red, reaching black. Such damage threatens not only human health, but also human life. III and IV degree burns are, of course, more dangerous, but superficial burns can also be fatal if they involve more than a third of the body surface.
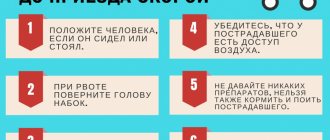
First aid for thermal burns
- The first thing to do as quickly as possible is to extinguish the flame (if there is one) on the victim’s clothing and skin. It is necessary to throw off burning clothes from a person or throw a cloth over his body to stop the access of air to the fire. A burning area of clothing can be covered with earth, sand, snow, or doused with water.
- Try to calm the victim and the people around him.
- Carefully remove from the injured person any smoldering remains of things that do not get into the wound. Under no circumstances should you remove clothing that is stuck to a burn. You should also not touch the burned body with your hands.
- If it is a sunburn, you need to move the affected person to the shade.
- If you do not have information about what happened, quickly clarify the circumstances of the accident (“the child knocked over a bowl of hot broth,” “clothes caught fire from the fire,” etc.).
- Hold the affected part of the body for 10-20 minutes under running cold running water (you can put it in a container with cool, clean water). This must be done so that the heated wound does not deepen or expand. In addition, it activates blood circulation in the wound. However, ice should not be used to cool the burned area to avoid the possibility of another injury - frostbite. In extreme cases (if there is no water nearby), cooling the wound with urine is allowed, but in practice there is almost never a reason to use this method.
- Apply any available anti-burn agent (ointment, gel) to the affected surface, and apply a sterile (if possible) dry bandage on top. You cannot use cotton wool, only gauze, bandages - fabric materials. It happens that you have neither anti-burn agent nor sterile bandages at hand, then you should apply any dry, clean bandage to the wound. You should not apply any folk remedies to the burn: vegetable oil, vodka solutions, kefir, sour cream, etc. You should also not apply Kalanchoe or aloe leaves or other “miracle remedies” to the burned skin. In case of a first degree burn (if there is no extensive damage to the skin or blisters), a bandage may not be applied at all, only an anti-burn gel can be applied.
- If there are extensive burns of the extremities, you need to carefully fix them with a splint (any available means), raising the burned arms (legs).
- If a large area of the body is burned and there are signs of burn shock (the person is weak, pale, has increased anxiety, there is tachycardia and a drop in blood pressure, cold sweat, breathing and heart rate are disturbed), you should give him as much liquid as possible to drink - juice, compote or plain clean water. Thanks to the intake of fluid into the body, intoxication resulting from the penetration of decay products of burnt tissue into the blood will decrease.
- If the victim complains of pain, then in order to avoid painful shock, you should give him any available painkiller (spasmalgon, analgin, etc.).
- If a person has no cardiac and (or) respiratory activity, cardiopulmonary resuscitation (artificial respiration, chest compressions) should be performed.
- In case of severe burns, call an ambulance for hospitalization of the victim or independently deliver him to a specialized medical institution. It is preferable to use, since not everyone can accurately say in which hospital or department burns are treated. It’s good when it’s a specialized clinic or at least a specialized department.
Treatment of thermal burns
Treatment of patients who have received thermal burns should include a set of means aimed at correcting the disorders that appeared in the body due to the burn. Antishock therapy should be adequate to the stage of medical care, the severity of burn shock and the age of the victim. It should include the following activities:
- pain relief;
- replenishment of blood deficiency (its components);
- prevention, treatment of hypoxia;
- correction of water-electrolyte, protein metabolism and acid-base balance of the blood;
- fight against intoxication;
- compensation of the body's energy costs;
- prevention, treatment of heart disorders;
- prevention, treatment of acute hepatic-renal failure.
In a specialized clinic (specialized department), primary care of burns is performed under anesthesia. Gentle treatment of wounds and the skin surrounding them is carried out with gauze wipes soaked in warm soapy water or a 0.5% solution of ammonia. After this, the burn surface is carefully washed with warm water or alcohol (40-70 degrees), dried and irrigated with antiseptic solutions.
Very dirty burn areas are cleaned with a 3% hydrogen peroxide solution. Particles of the epidermis are removed from superficial burns with tweezers or scissors. Small blisters are not opened, but large detached blisters are cut at the base and then emptied by lightly pressing them with a gauze swab. For burns caused by tar or bitumen, use purified gasoline.
With the open method of treatment, a thin layer of a special ointment or another synthetic (biological) coating is applied to the surface of the wound. With a closed method of treatment, a bandage with a special ointment (synthomycin, streptomycin) or emulsion (for example, sulfidine) is applied to the burn. Vishnevsky's anti-burn oil-balsamic emulsion is also effective. Such dressings do not interfere with the healing of the burn, do not cause pain when changing, and provide high-quality protection of the wound from infection. The bandage is carefully bandaged, lightly pressing on the tissue. It should not move; if the disease progresses successfully, the bandage is not removed until 7-9 days. This period is enough for the burn surface to epithelialize.
If the limbs are burned, immobilization is required, i.e. temporary immobilization. Any position convenient for the victim can be selected. In order to avoid the negative consequences of immobilization, every 2-3 days it is necessary to pause immobilization in order to make movements in the joints.
There is no single correct opinion on what should be done with burn blisters. Some doctors quickly remove them, explaining that their internal contents are not sterile; other doctors release liquid from the blisters, but do not remove the blisters themselves.
To restore the body of a victim who has received a fourth-degree burn, prompt, competent treatment and skin grafting are required.
Forecast of thermal burns
Pathophysiological changes that inevitably develop in the body affected by a burn provoke disturbances in the vital systems of the body and even threaten human life. The prognosis largely depends on the area of the lesion, the extent of the lesion and the age of the victim. Mortality from burns is high in old people over 60 years of age and children under 3 years of age. However, even for patients of this age, burns cannot be considered a death sentence.
A critical condition is considered to be 100% - a total burn of the first degree, and burns of the second-third degree when more than a third of the body surface is affected. Life-threatening are third- and fourth-degree burns that affect the genitals, face, perineum (if they affect 10% of the body surface), and burns of the torso and limbs if the affected area is more than 15%. For more accurate predictions of burns, special methods have been developed - the “Rule of Hundreds”, “Frank Index”, which take into account the depth, extent of the affected area and the age of the victim.
You need to know: if the thermal effect on the skin lasts longer than 1 minute and exceeds 45 ° C, this inevitably leads to overheating of cells and their death due to inactivation of enzymes, protein denaturation, paralysis of tissue respiration and other metabolic disorders. After the cessation of thermal exposure, hyperthermia in the tissues does not stop, but continues and even becomes more active!
Pathogenesis of thermal burn
A thermal burn causes local changes in the skin that go through several stages of development.
The most comfortable body temperature to ensure normal biological activity of enzymes is +36…+37 ℃. The range of +37…+41 ℃ is also acceptable, and at +42 ℃ protein destruction begins.
When the body is exposed to high temperatures, burns of varying degrees of severity occur. Moreover, not only the temperature of the damaging agent is important, but also the time of exposure. The depth of tissue damage directly depends on the time of exposure to the damaging factor due to the physical properties of the skin. Brief exposure to even very hot objects and liquids may not result in a burn.
In case of deep burns, three lesion zones are distinguished: the coagulation zone, the paranecrosis zone and the peripheral zone.
Damage to the epidermal barrier leads to bacterial infection, fluid loss, and impaired thermoregulation. A tissue burn is accompanied by edema and hypothermia, since thermoregulation decreases as the dermis is damaged and is completely absent in open wounds.
The severity of the victim’s condition depends on the area of the affected surface and the depth of the burn. In the first days, the severity of the condition is influenced mainly by the extent of the lesion, and in subsequent days - by its depth.
Symptoms
A sign of a 3rd degree burn is necrosis of the skin in the affected area - necrosis, which can be dry or wet. The first occurs when interacting with hot solid objects. The skin at the site of injury becomes brown or black. Wet necrosis occurs when exposed to hot liquids or steam. At the site of injury, the skin takes on a swollen, yellowish appearance and may become blistered.
It is important to distinguish the severity of a 3rd degree burn. It is classified into forms IIIa and IIIb, which differ in the following characteristics:
- in form IIIa, all layers of the skin are damaged, large blisters form, and the wound is covered with a scab;
- form IIIb is more severe, not only the skin is affected, but also the subcutaneous fat. The blisters are filled with bloody contents, the crust looks like a wrinkled scab.
Causes of thermal burns
The main causes of thermal burns are industrial accidents and carelessness at home. You can get burned:
- flame (most often this is a second degree burn, which affects the respiratory and visual organs);
- liquid (often this is II–III degree of damage involving deep tissues);
- steam (shallow but extensive burn);
- with a hot object (II–IV degree of damage) with a clear contour and deep damage and possible peeling of tissue.
Stages and symptoms of thermal injuries
First aid for thermal burns is carried out taking into account the stage (depth) of tissue damage. In medicine there are four stages:
- I - partial damage to the surface layer of the skin. Accompanied by slight swelling, burning, redness;
- II - complete damage to the skin surface. Characterized by blistering, burning pain;
- III - the lesion reaches the deep layers of the skin. There are grades IIIa and IIIb. The first is accompanied by fragmentary damage to the deep layers and the formation of dry dark crusts (scabs). The second is characterized by the death of layers of the epidermis and damage to fatty tissue;
- IV - the most dangerous burns, in which all layers of skin, muscle, bone tissue and tendons are injured.
In every case, except for the mildest skin injuries, you should immediately call an ambulance. You should not try to apply medications yourself, treat the affected areas with alcohol, or carry out other manipulations. The main thing is to alleviate the victim’s condition before the doctors arrive. Specialists will assess the extent of the damage, provide professional assistance, and, if necessary, hospitalize you.
Diagnostics
The doctor assesses the depth and area of tissue damage. Depending on the results of the examination, urine and blood tests and x-rays may be prescribed.
Fire victims may experience intoxication by combustion products and damage to the respiratory tract by carbon monoxide (swelling, tissue injury, soot). Their symptoms appear within several hours (sometimes minutes): difficulty breathing, cough with sputum. To identify such pathologies, the following are carried out:
- Endoscopic examination of the upper respiratory tract.
- Chest X-ray (to assess the condition of the lower respiratory tract).
First aid for victims of thermal burns
Competent first aid actions for thermal burns will reduce the risk of dangerous complications and contribute to the rapid restoration of tissues and the victim himself. Emergency assistance involves the following algorithm of actions:
- Stop contact of the affected area of the body with the traumatic factor.
- Place the affected area under tap water pressure for 10–15 minutes. It is important to stop the penetration of temperature effects deeper. This can be achieved by cooling. Ice cannot be used for this purpose. A sharp change in temperature will lead to cell death.
- If we are talking about a burn with boiling liquid, it is necessary to free the damaged area from clothing without touching the wound. If the fabric is stuck to the body, you cannot forcibly tear it off; you can only cut off the excess pieces of material around it.
- Apply a sterile bandage to the wound using special pharmaceutical products.
- Give the victim a pain reliever.
- To reduce intoxication due to the release of decay products of dead tissue into the blood, the victim is given warm mineral water without gas or plain water, adding 0.5 tsp to it. salt and soda per 1 liter.
Before providing first aid to the victim at home, you must call the ambulance service.
KEYLONS. A LITTLE ABOUT THE MECHANISM OF CELL CYCLE REGULATION
Research in the field of skin regeneration and the general mechanisms of the cell cycle has been conducted since the middle of the last century. R. Weiss and J. Kavanau, W. S. Bullough and T. Rytomaa, V. I. Prilutsky and Yu. A. Romanov are the founders of the theory of cell division. P. Nurse, Leland H. Harwell and R. Timothy Hunt are modern researchers of the principles of regulation of the work of individual cells and the body as a whole.
Disruption of the process of cell division (impairment of cell mitosis) is a source of not only cancer. Limited regeneration leads to aging of cells and aging of the body as a whole. In case of injuries and pathologies, low tissue regeneration significantly prolongs the healing process.
Outstanding examples of self-repair are known to everyone: severed tails, damaged hearts, and spinal cords in amphibians are restored (repaired) in a very short time. What signals does the body give to tissues so that they begin to grow, what is the growth factor? But first, about the life path of cells. A cell is the elementary unit of all living organisms. All living things are made up of cells. Regeneration, cell reproduction by mitosis occurs as follows: genetic material is reproduced inside the cell (this ensures the genetic identity of the daughter cells), after which the cell divides.
The process of cell division from the start of the mechanism to the actual division is called proliferation. Proliferation is regulated both by the cell itself and its environment. The main signal for triggering the cell division mechanism is provided by the plasma membrane of the cell. The membrane has special receptors on its surface that evaluate the “environment” around the cell and trigger the process of proliferation. These signals can come from neighboring cells, as well as from the interaction of cells with various compounds that stimulate entry into the cell cycle. These compounds are called growth factors.
But in tissues there are also substances that limit cell division. These are the Kaylons.
Keylons
- substances contained in tissue (simple proteins or glycoproteins) that specifically suppress cell division and DNA synthesis in this tissue. Keylons do not have species specificity. The action of kelons is to suppress or slow down the rate of cell division in the tissues that produce them. For example, keylons of the Basal Layer of the Epidermis act only on the Epidermis.
Cell regeneration is described by a growth regulation model. This model explains how body tissues carry out self-regulation. Any tissue capable of regeneration consists of two types of cells: cells capable of dividing and cells that cannot divide: proliferating and differentiated cells. The behavior of proliferating cells is controlled by differentiated cells: Kaylons are produced in differentiated cells and act on cells capable of dividing - proliferating cells. If for some reason the number of differentiated functioning cells decreases (for example, after injury), the inhibitory effect of the keylons weakens and the population size is restored. This ensures a balance between tissue growth and loss and explains the regeneration process.
Treatment for thermal damage
Complex treatment for burns involves the use of local healing agents, anti-inflammatory drugs, and measures to prevent infection of the affected tissues. The recovery process takes place in stages:
- Inflammatory process. Dead tissue melts, and the wound is gradually cleared of decay products and foreign particles.
- Recovery period. Connective and granulation tissue is formed.
- Epithelization. The damaged area is covered with skin, a scar is formed, and the tissues heal.
In order for the healing process to go according to plan and without complications, it is important to take all necessary measures to stop the pathological effects even before the doctors arrive. To do this, you need to take into account a number of prohibitions regarding the rules for caring for the victim. What you should never do:
- remove stuck clothing from damaged skin;
- apply ice to the burn (causes frostbite);
- touch the wound with your hands, especially dirty ones.
- open blisters, since infection will quickly penetrate into open wounds;
- cover the wound with an adhesive plaster if it is not intended for the treatment of burns;
- treat burned skin with kefir, alcohol, herbal decoction, etc.;
- apply aloe to the wound;
- use cotton swabs to clean the wound (the fibers will get stuck and cause inflammation).
In addition to the above, you should not use any ointments, oils or creams without medical advice. If used incorrectly and untimely, they will only complicate further wound care and slow down the recovery process. Treatment of burns should be prescribed and supervised by a physician.
Drugs
Providing first aid for thermal burns greatly influences the further course of treatment and the prospects for recovery.
On the first day, analgesic and antihistamines are administered intravenously. Novocaine blockades are used as an antishock agent, depending on the location of the burn. If more than 15% of the victim’s body is affected, regardless of the degree of burn, inhalation of humidified oxygen is used.
In order to equalize hemodynamics, infusion therapy with blood substitutes is used, and in cases of weakened cardiac activity, caffeine-containing drugs are used.
First aid at home must be provided correctly, no matter how minor the burn.
First of all, it is necessary to remove the damaging factor and, if possible, cool the burn site. The victim should be given plenty of fluids, and if the pain is severe, an over-the-counter analgesic can be given. In case of severe injuries, you should limit yourself to this and wait for the arrival of doctors.
In milder cases, you can clean the burn site with chlorhexidine and apply a special atraumatic dressing.
Physiotherapy
Physiotherapeutic methods for treating thermal burns are prescribed depending on the stage of treatment.
- UV therapy is aimed at tissue regeneration. With the help of ultrasound therapy, the rejection of dead tissue is accelerated, micromassage of the underlying tissue is performed, which helps improve blood supply. They also have an antibacterial effect and enhance the effect of medications.
- Ozone therapy has a bactericidal, immunomodulatory, detoxifying effect, stimulates the formation of granulations and epithelium.
Treatment options also include magnetic therapy, low-intensity laser therapy, light therapy, mechanical-vacuum therapy, and treatment using air-plasma flow. Remember that any treatment and medications can only be prescribed to you by a doctor.
Operation
Surgical treatment is prescribed for severe thermal burns. It involves several types of surgical intervention:
- necrotomy - dissection of a circular burn scab;
- necrectomy - excision of non-viable tissue;
- if necessary, amputation of limbs;
- plastic closure of a burn wound
- reconstructive and plastic measures.
Treatment methods
There are two approaches to the treatment of 3rd degree burns: conservative, or closed, and surgical.
How to treat a 3rd degree burn is determined by the doctor. The choice of technique depends on the scale of the lesion. Grade IIIA burns require long-term conservative therapy in combination with surgical treatment. Deep burns are treated only with surgical methods in a hospital.
Conservative treatment
First of all, the doctor will assess the severity of the harm and take measures to prevent wound infection. For this purpose, bandages with antiseptic and iodine-containing preparations are used. Daily dressings with drugs that help drain purulent discharge and reject scabs prevent intoxication of the body.
At the regeneration stage, balsamic dressings are used to stimulate the growth of granulation tissue. In the postoperative period, sponge dressings with anti-inflammatory drugs are used.
Surgery
There are several methods, each of which requires a specific sequence of actions:
- surgical removal of necrotic tissue from the wound;
- necrotomy - dissection of the scab to viable tissue to improve blood supply;
- necrectomy - excision of necrotic tissue in order to create conditions for epithelization or in preparation for skin transplantation;
- amputation of a limb or part thereof on an arm or leg;
- excision of granulations;
- skin plastic surgery in areas of high functionality and aesthetically important areas.
Physiotherapy
At the initial stage of treatment, physical therapy is used to relieve pain and prevent infection. At the granulation stage - to accelerate the rejection of necrotic tissue and stimulate epithelization. In the postoperative period - in order to accelerate the survival of implants and prevent the formation of scars and contractures.
As the burn site heals, the following methods are used: ultraviolet irradiation, ultrasound, laser irradiation, phototherapy, cryotherapy, ozone therapy, magnetic therapy in accordance with the algorithm prescribed by the doctor.
Forecast of thermal burns
In case of thermal burns, predicting the further course of the disease depends mainly on the area and depth of the lesion, as well as on the presence of concomitant diseases. Extensive and deep burns can pose a serious danger to human health and life.
When predicting the condition of a victim, two main methods are used: the “hundreds” rule and the Frank index. The “hundreds” rule only applies to adult patients. It consists of summing the patient’s age and the relative area of the affected surface to the total body area. With values:
- less than 60 – the prognosis is favorable;
- from 61 to 80 – moderately favorable;
- from 81 to 100 - doubtful;
- 100 - the prognosis is unfavorable.
The age of the victim plays a significant role in determining the immune and reparative capabilities of the body.
The Frank index takes into account the total area of superficial and triple the area of deep burns:
- less than 30 – the prognosis is favorable;
- from 31 to 60 - moderately favorable;
- from 61 to 90 - doubtful;
- 90 or more - the prognosis is unfavorable.
Complications
Thermal burns are often accompanied by complications, which are usually classified into primary, secondary and late.
- Primary complications resulting from injury are typical only for 4th degree burns. These include charring and mummification of soft tissues, thrombosis of large arteries and veins.
- Secondary complications often arise due to infection and can affect the skin, soft tissues, blood vessels and nerves, and internal organs. These include gangrene, abscesses, hepatitis, osteomyelitis, etc.
- Late complications develop during or after healing of burn wounds. These are pyelonephritis, hepatitis, dysfunction of joints and limbs, in some cases burn dermatitis and eczema.
Local complications of thermal burns include the formation of scabs, contractures and scars. A scab is a hard, necrotic tissue that encircles the limbs, neck or torso, the so-called circular scab. The scab puts pressure on the tissue, causing ischemia - a local disruption of blood flow, which can cause breathing problems. Scars and contractures form with high-grade burns and can lead to limited joint mobility. Do not self-medicate, be sure to consult your doctor.