Chronic venous insufficiency (CVI) is a pathology that develops due to a violation of the outflow of blood from the veins of the extremities. Frequent symptoms are changes in skin color, cramps, swelling, pain. The most common is chronic venous insufficiency of the lower extremities.
Often, patients ignore the first symptoms of CVI and turn to a phlebologist with deteriorated health and the condition of the lower extremities. At the earliest stages, the disease is treated conservatively; when pronounced signs of impaired venous circulation appear, complex therapy is required, usually including treatment of varicose veins, nutritional correction, physical activity and wearing compression garments (1, English).
From the article you will learn the causes of chronic venous insufficiency and features of the development of the disease. Classic symptoms and method of diagnosis according to the international classification. Diagnostics and therapy are discussed in detail.
Prevalence of the disease
In the world, those diagnosed with chronic venous insufficiency in different countries range from 15 to 25%, depending on the development of medicine in the country. In Russia, symptoms of CVI are observed in every second person aged 20–50 years, of which up to 15% have an established diagnosis, and 4% suffer from a severe form of the disease with complications in the form of trophic ulcers.
Chronic venous insufficiency is caused by upright posture, as a result of excessive stress on the legs. The impetus for its development can be congenital and acquired pathological conditions, injuries and prolonged physical activity. CVI is not always accompanied by visible changes in the veins; in most cases (mild form) it is a feeling of heaviness in the legs, swelling in the evenings, increased fatigue, pain when forced to stand for long periods of time.
CVI - treatment at home
Don't be afraid if you are diagnosed with CVI. Treatment with folk remedies will alleviate the situation. For example, venotonic drugs will help. They strengthen the walls of blood vessels, stimulate microcirculation, and quickly relieve the feeling of tired legs and swelling. Patients are also treated with blood thinning medications.
Do you need to relieve the pain of CVI? Treatment with traditional methods:
- Apple vinegar. Twice a day for 30 minutes. Apply gauze soaked in vinegar to your feet for 30 minutes. Keep your legs higher. Reviews about the product are contradictory, but the majority note a positive, weak effect.
- Bell pepper. Dilute a teaspoon of pepper powder in a glass of hot water and drink three times a day. The product stops leg pain and improves blood flow. But CVI does not go away that easily, treatment, the results are still not the same as when treated by a professional phlebologist.
Causes of CVI
Most often, venous insufficiency occurs with varicose veins, as well as against the background of such diseases and pathological conditions as:
- congenital pathology of the venous system;
- congenital aplasia and hypoaplasia of the deep veins;
- congenital arteriovenous fistulas;
- congenital osteohypertrophic nevus with varicose veins;
- suffered acute thrombosis of the main veins;
- Klippel-Trenaunay syndrome;
- previous phlebothrombosis.
In recent years, a new cause for the development of chronic venous insufficiency has emerged, which is increasingly being identified - phlebopathy. This name refers to the state of venous stagnation in the absence of clinical signs of pathology. In rare cases, CVI begins to develop after a trauma (bruise, rupture, deep burns or hypothermia).
Establishing diagnosis
CVI is often equated with varicose veins, which is not correct. Varicose veins are one of the manifestations of pathology.
Diagnosis is based on medical history, examination and additional diagnostic methods. The specialist’s task is to determine the presence of chronic venous insufficiency, diagnosis according to the CEAP classification, and formulate treatment tactics.
An ultrasound of the veins is mandatory - only an ultrasound examination allows one to study the condition of the venous apparatus and make an accurate diagnosis.
The main ultrasound diagnostic methods include Dopplerography and angioscanning.
Doppler ultrasound
Used to study blood flow and diagnose reflux. Informative for the study of superficial veins with the presence of telangiectasia and reticular varicose veins (class C1). In patients with suspected damage to the deep veins of the extremities, with trophic ulcers, the method is often uninformative.
Ultrasound angioscanning
Visualization of deep and superficial veins, assessment of blood flow. According to the results of ultrasound scanning, unaffected veins, vessels with signs of reflux of non-post-thrombotic origin, and vessels changed as a result of previous thrombosis are determined. The method gives a complete picture of the condition of the superficial and deep veins of the lower extremities, and well visualizes the changed vessels.
During pregnancy, acute thrombosis, chronic arterial insufficiency, pathologies of the kidneys and liver and many other diseases, ultrasound angioscanning is an important tool for the differential diagnosis of CVI; it identifies pathologies with high accuracy, which allows you to prescribe the correct treatment.
X-ray contrast venography (venography)
Injection of a contrast agent into the vascular bed, followed by a series of x-rays. Currently, the technique is rarely performed, since ultrasound research methods have become much more informative and accessible.
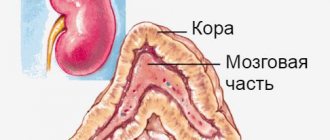
The mechanism of the onset and development of the disease
Under the influence of gravity, the blood in the vessels descends to the lower extremities, the body has to make efforts to lift it. Venous valves prevent blood from flowing downwards, which are actively helped in this by physical activity, muscle contraction and bending of the knees. The combination of these factors ensures normal blood flow.
Maintaining a constant resistance to gravity is possible due to physiological changes in the lumen of blood vessels when changing body position, the operation of the valve apparatus and the tone (elasticity) of the venous wall. If one of these component mechanisms is disrupted, pathological processes begin to affect the entire system as a whole. Loss of elasticity of the section of the vein below the valve, and its expansion leads to valvular incompetence, the inability to maintain blood flow for subsequent rise. Stagnation of fluid leads to increased pressure to move blood upward. But, over time, increased pressure increases the volume of the part of the vein that has lost its elasticity.
Venous reflux (reverse flow of blood from top to bottom) can join the pathological process. The liquid begins to stagnate and put pressure on the walls of the vessel. As a result, blood plasma leaks into the surrounding tissue, causing swelling. The situation develops similarly with initial valvular insufficiency.
Simultaneously with circulatory failure, the lymphatic system is also overloaded. Trophic disorders contribute to the formation of trophic ulcers. Trophic ulcers are long-term non-healing wounds (6 months or more) affecting the skin and tissues. They form on the lower leg, are surrounded by an area of inflammation, and have a high risk of infection.
Risk factors for CVI
A number of factors significantly increase the risk of developing chronic venous insufficiency, these include:
- Genetic predisposition, including pathologies of connective tissue and weakness of the vascular wall.
- Taking hormone-containing drugs, including hormonal contraceptives.
- Low physical activity, sedentary lifestyle, constant heavy lifting, excess weight.
- Chronic constipation.
CVI is more often diagnosed in women, since the formation of venous insufficiency is influenced by a high concentration of estrogens (female steroid sex hormones). The period of pregnancy and childbirth and the use of hormonal contraceptives have a negative impact. With age, the likelihood of developing the disease increases in both sexes due to prolonged exposure to adverse factors.
Classification of CVI
- 1st degree:
is expressed in a feeling of heaviness, aching pain, passing, minor swelling and night cramps.
- 2nd degree:
persistent swelling, hyperpigmentation (darkening of the skin of the affected limb), lipodermatosclerosis (dystrophic changes in fatty tissue), dry and weeping eczema (serous inflammation of the dermis).
- 3rd degree:
To the above signs of stage 2, trophic ulcers, current or already healed, are added.
- There is also 0 degree
when the patient does not observe changes, there are no complaints, however, the pathological processes have already started. The treatment method for patients with zero degree CVI differs from the treatment of patients at other stages.
In international practice, chronic venous insufficiency is divided into 6 degrees according to clinical manifestations, including zero (CEAP system). The disease also has an etiological classification based on its causes:
- EC is a congenital pathology.
- ES is an acquired form as a result of thrombosis, varicose veins, or trauma.
- EP is an unclear cause of venous insufficiency.
There is also an anatomical classification based on location, taking into account pathophysiology, disability scale and a number of other factors.
Symptoms of chronic venous insufficiency
At an early stage, chronic venous insufficiency has a broad clinical picture, expressed in one symptom, followed by a chaotic addition of other manifestations. As a rule, they appear or intensify after long periods of sitting or standing, as well as during periods of increased physical activity:
- heaviness in the legs;
- fatigue, buzzing;
- aching pain;
- transient swelling;
- numbness, temporary loss of sensation;
- cramps that occur at night.
If you regularly experience at least one of these symptoms, you should consult a doctor. Subsequently, with the development of pathology, pigmentation of the skin of the lower leg will occur, the skin will lose elasticity and become dry.
As it progresses (stages 2 and 3), symptoms such as:
- persistent swelling;
- increased pain during exercise;
- formation of ulcers and eczema;
- phlebeurysm.
Lack of blood circulation negatively affects not only the affected area, but also the entire body as a whole. Dizziness and fainting, high mental and physical fatigue may occur. Signs of heart failure are also noted: heart rhythm disturbances, pale skin, shortness of breath.
What happens if venous insufficiency is not treated?
Venous insufficiency is a trigger for a number of disorders and diseases with more serious consequences:
- Skin changes (pigmentation)
- Eczema (skin inflammation)
- Ulcers (venous ulcers)
Compression jersey medi
Thanks to the breathable and elastic material, compression jersey provides high wearing comfort. Modern medical compression hosiery is visually indistinguishable from model hosiery, but provides high medical effectiveness when used.
The human body
How do veins work?
Vienna
Product Tips
Ideal compression product
Compression hosiery
Diagnosis and treatment of CVI
At an appointment with a phlebologist at the Ambulatory Surgery Center, the patient is diagnosed based on the medical history, the patient’s complaints, and the results of the study. The main method of instrumental examination is duplex ultrasound scanning. In our clinic, functional diagnostic doctors during the study not only confirm the presence of CVI, but also help surgeons determine the extent of damage to the venous system and the choice of tactics for further action. In some cases, the attending physician may prescribe a duplex angioscan or X-ray contrast study (phlebography).
Treatment of chronic venous insufficiency is a set of measures, the purpose of which is to restore the functionality of the venous and lymphatic systems, eliminate the pathologies that arise from them and prevent relapses. The method of therapy is selected individually for each patient, taking into account the degree of pathological changes, medical history, age and concomitant diseases.
Conservative treatment
A course of treatment is prescribed, lasting on average 2 - 3 months, then after a certain period it is resumed. The course usually includes:
- medicines (phlebotrobic drugs);
- local use of antiseptic ointments;
- corticosteroid drugs;
- elastic compression (bandages and compression hosiery);
- treatment of associated secondary infections;
- elevated position of the legs when lying down.
In some cases, antibiotics and diuretics are prescribed to reduce swelling. The greatest role in the routine treatment of CVI is played by elastic compression, including hardware, pneumatic, and leg elevation. Compression is indicated for all patients, even those with ulcers. In this case, I use elastic bandaging, and then wear special stockings. They should create a distal pressure of 20–30 mm Hg. for patients of the first stage, 30–40 mm Hg. – second and up to 60 mm Hg. at the third.
The effectiveness of therapy directly depends on the active participation of the patient. He needs to strictly follow the doctor’s recommendations and build his life in such a way that conditions that aggravate the course of the disease are not created.
Surgery
Surgery is performed only in 10% of patients with:
- severe concomitant diseases;
- trophic disorders;
- transformed tributaries of the great (small) saphenous veins;
- relapse of varicose veins and in other similar cases.
For this purpose, a minimally invasive surgery technique is chosen - miniphlebectomy.
. The operation is performed under local anesthesia. Through small punctures, the vascular surgeon gains access to the affected areas of the veins to perform ligation (vessel ligation), vein removal, and valve reconstruction. The tasks of a vascular surgeon include eliminating pathological blood discharge and truncation of varicose veins. After the operation, an hour later, the patient can go home; a hospital stay is not required.
CVI - Diagnostics
Typically, patients turn to a phlebologist when obvious signs of CVI are visible to the naked eye, and the diagnosis is easy to make. Specialized clinics use ultrasound methods to diagnose CVI:
- the condition of blood vessels is studied;
- assesses how blood flows through them;
- Disturbances in the functioning of venous valves are considered.
Ultrasound scanning gives a complete picture of the causes of CVI
With an ultrasound examination, the doctor receives a three-dimensional image of the vessel, reliable information about its functioning, and can make an objective diagnosis.