How are respiratory failure classified by severity?
The main criteria on which the classification is based are the measurement of blood gas balance, primarily the partial pressure of oxygen
(PaO2), carbon dioxide in arterial blood, as well as blood oxygen saturation (SaO2).
When determining the severity, it is important to identify the form in which the disease occurs.
DN shapes depending on the nature of the flow
There are two forms of DN - acute and chronic.
Differences between the chronic form and the acute form:
- chronic form of
DN - develops gradually, may not have symptoms for a long time. Usually appears after an untreated acute form; - acute
DN - develops quickly, in some cases symptoms appear within a few minutes. In most cases, the pathology is accompanied by hemodynamic disturbances (indicators of blood movement through the vessels).
The disease in a chronic form without exacerbations requires regular monitoring of the patient by a doctor.
Acute respiratory failure is more dangerous than chronic respiratory failure and requires immediate treatment.
Classification according to severity includes 3 types of chronic and 4 types of acute forms of pathology.
Severity of chronic DN
As DN develops, the symptoms become more complex and the patient’s condition worsens.
Diagnosing the disease at the initial stage simplifies and speeds up the treatment process.
| Degrees of DN | Types | Symptoms |
| I | Asymptomatic (hidden) |
|
| II | Compensated |
|
| III | Decompensated |
|
Symptoms in chronic deficiency are not as intense as in the acute form.
How is acute respiratory failure classified?
There are 4 degrees of severity of acute DN:
I degree
. It is characterized by shortness of breath (may appear on inhalation or exhalation), increased heart rate.
- PaO2 - from 60 to 79 mm Hg;
- SaO2 - 91-94%.
II degree
. The skin is marbled, bluish. Convulsions are possible, consciousness becomes darkened. When breathing, even at rest, additional muscles are activated.
- PaO2 - 41-59 mm Hg;
- SaO2 - from 75 to 90%.
III degree
. Shortness of breath: sharp shortness of breath is replaced by attacks of respiratory arrest, a decrease in the number of breaths per minute. Even at rest, the lips retain a rich bluish tint.
- PaO2 - from 31 to 40 mm Hg;
- SaO2 - from 62 to 74%.
IV degree
. State of hypoxic coma: breathing is rare, accompanied by convulsions. Possible respiratory arrest. Cyanosis of the skin of the whole body, blood pressure at a critically low level.
- PaO2 - up to 30 mm Hg;
- SaO2 - below 60%.
IV degree corresponds to a terminal condition and requires emergency assistance.
In the body of a healthy person, PaO2 is above 80 mm Hg, the level of SaO2 is above 95%.
If the indicators are outside the normal range, this indicates a high risk of developing respiratory failure.
What are the symptoms of the disease
The main symptom of the disease is the presence of shortness of breath. It appears as rapid, complicated breathing, for which auxiliary muscles are used; this does not happen with standard inhalation and exhalation. The remaining symptoms are expressed by hypoxemia and hypercapnia.
Lack of oxygen in the alveoli provokes increased stress on the respiratory muscles. This specific time ensures that the gas content of the blood fluid is maintained. When the respiratory muscles become tired, the oxygen saturation of the blood decreases and the volume of CO2 increases.
An additional symptom is cyanosis, the degree of manifestation of which indicates the complexity of the disease. The subcompensation stage is accompanied by cyanosis of the lips and nail plates; with decompensation, the disease spreads and becomes generalized in the terminal stage. Hemodynamic manifestations characteristic of hypoxemia are expressed in the form of low blood pressure and an increase in heart rate.
Chronic respiratory failure is accompanied by increased breathing; its reduction to 12 per minute is a stern warning signal about possible respiratory arrest. It is typical to involve muscles that are not involved in breathing (neck muscles, work of the abdominal muscles during exhalation, flaring of the nose).
The patients' fingers outwardly become like drumsticks, limbs, warm, moist. Hypercapnia manifests itself as dilation of blood vessels on the face and oral mucosa. When it intensifies, a darkening of consciousness appears at times. Hypercapnic suppression of the respiratory center may reduce shortness of breath.
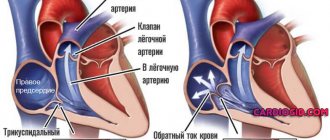
This leads to a misunderstanding of the situation, because it is assumed that the patient is better. After a few years, cardiopulmonary pathology develops. The etiology is an increase in pressure in the artery of the lung along with overload of the right heart. It is expressed as increased shortness of breath, the formation of edema in the lower extremities.
With the development of pulmonary pathology, the patient’s anxiety gives way to slowness, consciousness is lost, and failure to provide assistance threatens to fall into a coma. Babies are affected by convulsions, the skin surface becomes bluish in color, becomes cold and damp.
Hypercapnia is accompanied by a change in the color of the skin surface to purple. In the initial stages, patients experience an increase in blood pressure and heart rate.
How are the severity of pathology in children determined?
DN in a child usually occurs in an acute form. The main differences between pathology in adults and children are different levels of blood gas parameters.
| Severity | Indicators (in mmHg) | Symptoms |
| I | — Ra oxygen drops to 60-80 |
|
| II |
|
|
| III |
|
|
| IV (hypoxic coma) |
|
|
If signs of DN 3 and 4 severity are detected, the child requires emergency hospitalization and intensive care. Treatment of children with mild DN (stages 1 and 2) is possible at home.
Causes
A disruption in the functioning of the cardiopulmonary system occurs due to one of the following situations:
- Spasm or blockage of the pulmonary artery by blood clots.
- The occurrence of blood clots in the heart cavity.
- Acute stage of bronchial asthma.
- Rapid development of pneumonia.
- Lung injury.
The root cause of the development of cardiopulmonary failure is serious changes in the functioning of the heart. This could be ischemia, heart attack, or valve dysfunction. With the development of this disease, gradual, but sometimes irreversible changes occur in the pulmonary system of the body. These include:
- Pulmonary hypertension, which is hereditary.
- Development of an inflammatory process in the lungs.
- Exacerbation of chronic diseases.
How to determine the severity of respiratory failure
To definitively diagnose the disease and its stage, it is enough to determine the level of blood gases.
Early diagnosis of DN includes examination of external respiration, identification of obstructive and restrictive disorders.
An examination for suspected DN necessarily includes spirometry and peak flowmetry, and arterial blood is taken for analysis.
The algorithm for determining respiratory failure consists of the following diagnostic criteria:
- oxygen tension (Pa) - lower than 45-50;
- carbon dioxide tension is higher than 50-60 (indicators in mmHg).
There is a low likelihood that a patient will undergo a blood gas test without good reason. Most often, diagnosis is carried out only when the pathology has manifested itself in the form of obvious
signs.
Diagnostics
You should start looking for the causes and treatment of shortness of breath immediately after you begin to notice such changes. The following methods are used to diagnose respiratory failure:
- Collection of anamnesis of the disease. The doctor carefully studies the patient’s medical history, his complaints, and learns his lifestyle.
- External examination of the patient. By studying the skin, chest muscles, and heart rhythm, the doctor can confirm or refute his guesses.
- Blood gas analysis is a reliable test. If there are deviations, a disease of the chest organs can be assumed.
The doctor makes the final diagnosis after a comprehensive diagnosis. It must be confirmed by laboratory tests.
How to recognize respiratory failure
Common clinical symptoms of DN include:
- rapid breathing, periodically changing to slow breathing;
- no breathing sounds are heard;
- pulse is unstable;
- retracted area between the ribs;
- the breathing process is difficult, it requires the use of additional muscles;
- the upper and lower limbs, the tip of the nose and the nasolabial triangle acquire a bluish tint;
- the patient has a pre-fainting state, loss of consciousness is possible;
- there is an increase in cardiac output (the volume of blood that is ejected by heart contractions per minute);
- the appearance of respiratory distress syndrome.
If at least a few symptoms of DN appear, the patient should undergo an examination, find out the reasons for the development of the pathology, and adhere to the doctor’s recommendations.
4.Treatment
The main directions are the restoration of airway patency, respiratory movements, cardiac activity, vascular tone, blood volume and composition. As a rule, the patient is intubated and connected to a ventilator (artificial lung ventilation), or an oxygen mask, nasal catheter, etc. is used. Bronchodilators, antispasmodics, analgesics or anesthetics, respiratory stimulants, blood substitutes and other compounds according to indications are administered symptomatically.
Measures are taken for drainage, removal of foreign bodies and accumulated substances, detoxification, desensitization, etc.
The prognosis is always serious - too much depends on the reasons that caused ARF, on accompanying circumstances and complications, on individual factors, but most importantly, on the timeliness and adequacy of the provision of pre-medical and medical care.
Sign up for a consultation
What to do if you have ARF
First aid for respiratory failure should be provided after calling an ambulance. There is no talk of waiting for a local therapist in case of ARF.
The algorithm of actions is as follows:
- Call an ambulance.
- You can seat the person near the table so that he can put his hands on the table and raise his shoulders higher - closer to his chin. This will allow the auxiliary respiratory muscles to have more range of motion.
- Try to calm the victim.
- Free him from his outerwear, unfasten all the buttons and the belt of his trousers so that nothing interferes with his breathing.
- Provide fresh air flow from windows and vents.
- Constantly reassure the patient and be with him.
- If a person has asthma, help him take 1-2 breaths from his inhaler.
- If such symptoms occur after eating fish or canned food, give him “Activated carbon” or other sorbents.
If ARF develops as a result of a foreign body entering the throat, an urgent need to perform the Heimlich maneuver: stand behind the victim, clasp him with both hands. Clench one hand into a fist and place the palm of your other hand under it. Now, with a pushing movement directed upward, bending our elbows, we press on the abdominal area “under the stomach” until the victim’s airways are completely cleared.
If the development of ARF was preceded by a cold or a barking cough, it is recommended to inhale with a 0.05% naphthysine solution through a nebulizer before the ambulance arrives: 3-4 drops per 5 ml of saline solution.
When signs of ARF are present in a person who has been in a car accident, then it is possible to remove him from the car or shift him only after fixing his cervical spine with a Shants-type collar.