Kidney functions
excretory
The nephrons (the structural units of the kidneys) filter the blood, resulting in the formation of urine.
Excreted in urine:
- Protein metabolism residues: urea, creatinine, ammonium salts, sulfuric, phosphoric, uric acids.
- Excess water, salts, micro- and macro-elements, glucose.
- Hormones.
- Harmful substances of third-party origin, including medications.
Homeostatic
Homeostasis means the balance of the internal environment of the body. The amount and ratio of vital substances (for example, water, sodium, potassium, etc.) can fluctuate only within limited limits - even a slight imbalance leads to disease.
The kidneys “monitor” that the amount of substances excreted corresponds to the amount of substances received. This maintains water-salt, acid-base, electrolytic, and osmotic homeostasis. This means that a constant volume of blood, external and intracellular fluid is ensured, the uninterrupted flow of metabolic processes is ensured, and a normal level of blood pressure is maintained.
Endocrine
This is the synthesis of some biologically active substances and hormones.
For example, the kidneys produce the hormone erythropoietin, which stimulates the production of red blood cells in the bone marrow. They also complete the formation of active vitamin D3 (calcitriol), which forms bone tissue.
Metabolic
Participation in the breakdown of proteins and the construction of part of cell membranes. Synthesis of glucose from other substances.
What is kidney failure
If the kidneys cannot fully cope with their tasks, this condition is called renal failure.
The disease is divided into two forms - acute and chronic:
- Acute kidney failure or acute kidney injury (AKI) is a disease that develops over several days or weeks. It is potentially reversible - organ function is often restored. However, this does not always happen, and the patient develops chronic renal failure.
- Chronic renal failure (CRF) is a slowly progressive kidney pathology leading to irreversible impairment of their function. The disease develops from several months to several years.
AKI develops into chronic renal failure if the acute injury lasts more than 3 months and kidney function is not fully restored after the causes are eliminated. And also if the causes are permanent - for example, with autoimmune destruction of kidney cells.
If one kidney is damaged and the other is functioning normally, the healthy organ will take over the functions of both. The person will feel healthy both subjectively and according to laboratory indicators. Therefore, kidney failure occurs when both kidneys are affected.
Both acute and chronic decline in organ function can occur at any age, but occurs more often in older people.
How does kidney failure manifest?
Symptoms depend on the form and stage of development of the disease:
- With AKI, the first symptoms are a sharp decrease or cessation of urination.
- With CPP, the progression of symptoms occurs slowly. At an early stage, a consequence of kidney dysfunction may be the kidneys' inability to reduce the volume of urine at night by reabsorbing water from it. Therefore, with a mild form of the disease, the only symptom may be nocturia - frequent urination at night.
As the pathology progresses, the filtering and excretory function of the kidneys is impaired. Metabolic acids are not removed from the body, so the acid-base balance of the blood shifts to the acidic side (acidosis). Urea, phosphorus, nitrogenous substances accumulate in the blood, and an excess of salts occurs. This self-poisoning of the body is called uremia, or urine leakage.
How renal failure manifests itself in uremia can be understood by the presence of the following symptoms:
- decreased appetite;
- apathy, general weakness;
- thirst;
- unpleasant taste in the mouth;
- sleep disorder;
- memory impairment;
- decrease in body temperature to an average of 35C;
- nausea.
If treatment is unsuccessful and the disease develops further, intoxication spreads to the nervous system. A person experiences involuntary muscle twitching and inhibition of reactions.
The body begins to rid itself of toxins in other ways, such as through continuous vomiting and diarrhea. The smell of ammonia appears from the mouth.
Nitrogenous substances are released through the skin and mucous membranes, which leads to their irritation, and then to uremic gastritis, tracheitis, and stomatitis. Severe pathology may occur - inflammation of the heart muscle (pericarditis).
When the lungs fill with fluid and the pericardium is damaged, shortness of breath occurs.
In the terminal stages of uremia, whitish urea crystals (uremic frost) appear on the patient’s nose, chin and neck. Blood pressure drops and confusion occurs.
Death may occur from uremic coma.
In severe stages of renal failure, the functioning of almost all body systems occurs.
In this case, the kidneys cannot produce the hormone erythropoietin in sufficient quantities, so the patient’s red blood cell count drops and anemia develops.
Calcitriol production is also reduced, leading to bone fragility. In children, kidney failure leads to delayed bone growth.
Hypertension and heart failure develop.
A persistent increase in uric acid levels often leads to gout.
Signs and symptoms
Initially, there may be no noticeable symptoms of decreased kidney function. However, as chronic kidney disease progresses and kidney function continues to decline, some symptoms may become apparent.
The list of main signs of chronic kidney disease includes:
- Changes in urination: frequent urination at night, painful urination, cloudy or foamy urine
- Peripheral edema: swelling in the arms and legs due to decreased body fluid production.
- Fatigue: feeling tired due to anemia, which develops due to decreased production of erythropoietin (EPO) in the kidneys.
- Itchy skin: Toxins accumulate in the blood and can cause significant itching.
- Loss of appetite and weight: The buildup of waste in the blood can cause loss of appetite, nausea, vomiting and lead to weight loss.
- Shortness of breath: develops due to associated anemia or fluid accumulation in the lungs.
- Dizziness: Associated with decreased oxygen supply to the brain.
Frequent urination
Fatigue
Causes of kidney failure
Kidney failure develops for three main reasons:
- circulatory disorders of organs;
- nephron damage;
- blockage of the urinary tract.
Two pathologies most often lead to the development of chronic renal failure:
- Diabetes.
- Severe hypertension (high blood pressure).
It is these diseases that lead to damage to the small vessels that feed the kidneys and persistent disruption of their blood circulation.
In some cases, it is impossible to identify the cause of the disease.
Causes of chronic kidney disease (CKD)
- Diabetes. Diabetic nephropathy is a common complication of diabetes.
- High blood pressure. Arterial hypertension is the main cause of CKD, as well as kidney pathologies cause an increase in blood pressure, since the organ is involved in the regulation of pressure. About nine out of ten patients with CKD stages 3-5 suffer from hypertension.
- Aging of the kidney. With age, organ function decreases. About half of people over 75 years of age have some degree of CKD.
- Glomerulonephritis.
- Renal artery stenosis.
- Polycystic kidney disease.
- Recurrent kidney infections.
- Systemic lupus erythematosus.
Diagnostics
The doctor performs a visual examination of the patient and prescribes laboratory and instrumental tests.
Blood chemistry:
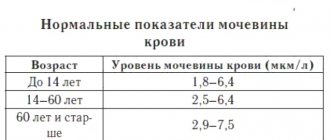
- Determination of the level of metabolic end products in the blood: creatinine, uric acid and nitrogen.
- Establishing the level of blood acidity (detection of acidosis).
- Determination of the amount of electrolytes in the blood.
General blood analysis:
Determination of hemoglobin and red blood cell levels. Indicators below normal may indicate a loss of the kidneys’ ability to participate in the synthesis of red blood cells.
Urine tests:
- A general clinical analysis allows you to determine the presence of protein, blood, and pathological cells in the urine.
- Biochemical - reveals the amount of electrolytes - sodium, potassium, calcium, phosphate compounds.
Of the hardware studies, ultrasound and CT (computed tomography) are most often prescribed.
In severe cases, a kidney biopsy is used - a tissue analysis that allows one to judge the extent and nature of its damage. It is not prescribed if the ultrasound revealed a significant reduction in organs and scar changes.
Treatment of kidney failure
The chronic form of the disease usually progresses even with treatment. However, the speed of the process can be reduced and the patient’s quality of life improved.
This depends on controlling the disease that led to the development of chronic renal failure. For example, in case of diabetes mellitus, it is very important to maintain normal sugar levels, as well as blood pressure levels in case of hypertension - otherwise the quality of kidney function will rapidly decline.
Measures taken to preserve kidney function are extremely important:
- Limit fluid intake.
- Refusal to take a number of medications that place increased stress on the kidneys.
- Diet therapy. Restriction in the diet of foods and drinks high in sodium, phosphorus, and potassium. This includes table salt, dairy products, liver, legumes, nuts, and the amount of protein is also strictly dosed. In the case of acute renal failure, the diet must be followed until the patient recovers, in case of chronic renal failure - throughout life.
- Drug therapy. Prescribed by a doctor based on test results.
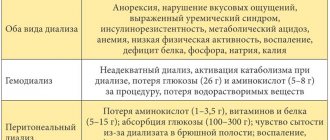
- Dialysis. Hardware removal of waste products. It is performed for severe and predictably long-term renal dysfunction. For severe chronic renal failure, it is used on an ongoing basis.
The patient must constantly monitor blood biochemistry - the level of creatinine, urea and phosphates in the blood, its acidity, and also undergo regular urine tests.
In case of complications - anemia, heart failure, osteodystrophy, etc. – it is necessary to involve targeted therapy.
If severe chronic renal failure develops, a person is advised to undergo a kidney transplant.
Without adequate treatment, kidney failure is fatal.
Chronic renal failure (CRF) is a gradual deterioration of kidney function over a long period of time. In modern literature, the term “chronic kidney disease” is found, which has a slightly broader meaning and implies a decrease in kidney function for three months or more.
The function of the kidneys is to maintain a normal balance of fluids and salts in the body, as well as to remove protein metabolic products (nitrogenous waste) from the body, forming urine. With chronic renal failure, blood purification does not occur sufficiently, which over time can lead to serious complications.
In the early stages of chronic kidney failure, there may be no symptoms. The disease is often discovered when kidney function deteriorates significantly.
It is very important to diagnose ESRD as early as possible in order to promptly begin treatment to slow the rate of decline in kidney function, since long-term kidney damage is irreversible. Without treatment, kidney function may deteriorate critically, which may require hemodialysis (artificial blood purification using an artificial kidney machine).
In some cases, the only treatment for a patient with chronic renal failure may be a kidney transplant.
Synonyms Russian
Chronic kidney disease, chronic renal failure, CKD, kidney shrinkage, nephrosclerosis, uremia.
English synonyms
Chronic Renal Failure, Chronic Kidney Disease, Chronic Kidney Failure, Chronic Renal Disease, CRF, CKF, CKD, CRD, Uremia.
Symptoms
Signs and symptoms of kidney failure may not appear for a long time. Symptoms can vary and include:
- nausea, vomiting, loss of appetite;
- frequent night urination;
- fatigue, fatigue;
- dry, pale skin, persistent itching;
- high blood pressure (hypertension);
- muscle twitching, tingling in different parts of the body, convulsions;
- bleeding from the gastrointestinal tract, gums, nose;
- perversion of taste;
- decreased libido, amenorrhea (lack of menstruation);
- swelling of the feet and ankles;
- decrease in intellectual activity.
Signs and symptoms of chronic renal failure are nonspecific, meaning they can occur in other diseases.
General information about the disease
Chronic kidney failure is a condition characterized by gradual deterioration of kidney function over months or years.
CRF is an important medical problem. Millions of people around the world suffer from this disease, and the number of cases is steadily increasing every year. There are 300-500 patients with chronic renal failure per million adults.
The kidneys are the main organ of the human excretory system. Normally, they maintain the ratio of water and active substances in the body, regulate the volume and composition of blood plasma. In addition, they produce a number of hormones - biologically active molecules.
Filtration of blood in the kidneys is carried out due to the functioning of the renal glomeruli. Each kidney contains a million glomeruli. Each renal glomerulus is a plexus of capillaries, in the form of a glomerulus, surrounded by a capsule. Passing through the glomeruli, the liquid part of the blood is filtered, after which primary urine is formed. The glomeruli normally allow only the liquid portion of the blood to pass through—proteins and other large molecules do not pass through the kidneys.
Next, primary urine enters the renal tubules - thin tubes in the kidneys. In the renal tubules, most of this fluid is reabsorbed (a process called reabsorption), and a small portion passes as urine into the renal pelvis, and then into the ureter and bladder. When enough urine has accumulated in the bladder, it is expelled from the body during urination.
About 150 liters of fluid pass through the kidneys per day, from which 1.5-2 liters of urine are formed. This is how the composition and volume of plasma is regulated.
In chronic renal failure, due to various reasons, the kidney tissue is replaced by scar tissue, the structure of the kidneys changes, the area of healthy tissue decreases, as a result of which the volume of filtered blood gradually decreases. At the same time, the remaining glomeruli and tubules hypertrophy, enhancing their function to compensate for this condition. Losing 75% of kidney tissue results in only a 50% reduction in blood filtration volume.
As a result, the volume of blood filtration decreases, the ratio of water and salts (electrolytes) in the body is disturbed, which is manifested by nausea, vomiting, muscle twitching, fluid accumulates in the tissues, which is manifested by edema, shortness of breath (due to the accumulation of fluid in the lungs). The density of urine decreases, it becomes lighter, and the patient begins to be bothered by frequent night urination.
Over time, the concentration in the blood of nitrogenous wastes (urea and creatinine) - the main end products of protein metabolism - increases significantly, which only serves as a sign of deterioration in kidney function, but does not manifest itself in any symptoms. An increase in urea leads to nausea, abdominal pain, and headache. Other nitrogenous wastes lead to persistent skin itching.
Symptoms of chronic renal failure do not appear immediately due to the large compensatory capabilities of the kidneys. Even with moderate kidney failure, there may be no symptoms.
Kidney failure can develop after a variety of diseases that damage the kidneys. The most common reasons for this are:
- diabetes mellitus type 1 or 2;
- high blood pressure (arterial hypertension);
- atherosclerosis – deposition of cholesterol in the walls of the renal arteries, preventing normal blood flow in them;
- glomerulonephritis is a group of diseases that have different causes, common to which is inflammation at the level of the renal glomeruli;
- urolithiasis – the appearance of kidney stones;
- chronic pyelonephritis – chronic inflammation of the kidney tissue;
- tuberculosis;
- polycystic kidney disease is a hereditary disease manifested by the formation of cavities in the kidney tissue (cysts);
- long-term blockage of the urinary tract, which can occur with adenoma or prostate cancer.
In recent years, instead of the term “chronic renal failure,” the term “chronic kidney disease” has increasingly been used, which implies a decrease in kidney function for three months or more. Chronic kidney disease is classified into five stages depending on the degree of impairment of glomerular filtration. The first 2 stages indicate mild renal dysfunction. The third, fourth and fifth stages correspond directly to renal failure itself. The last stage is called the terminal (final) stage. The final stage of chronic renal failure, when kidney function is critically reduced and the patient is bothered by many complaints, is called uremia.
Chronic renal failure can lead to the development of a wide range of different complications:
- Anemia. Normally, the kidneys produce the hormone erythropoietin, which stimulates the formation of red blood cells (the main blood cells that carry oxygen from the lungs to organs and tissues) in the bone marrow. As the area of healthy kidney tissue decreases, the production of erythropoietin and red blood cells decreases, anemia occurs (decrease in the level of red blood cells and hemoglobin in the blood), which is manifested by weakness and fatigue.
- Pericarditis is the accumulation of fluid in the lining surrounding the heart (pericardium). This condition can threaten the normal contractions of the heart and lead to the death of the patient.
- Encephalopathy. The term encephalopathy refers to a condition associated with the toxic effects of nitrogenous waste on the brain. In severe cases, this can lead to coma.
- Ulcers of the gastrointestinal tract, which can lead to spontaneous bleeding.
- Bone damage. Almost all patients with chronic renal failure have impaired calcium and phosphorus metabolism, which leads to softening of the bones and an increased risk of fractures.
- Heart or pulmonary failure. Fluid retention in the body with chronic renal failure can lead to the development or aggravate heart or lung failure, manifested by shortness of breath and edema.
- Myocardial infarction, stroke. CRF accelerates the progression of atherosclerosis, a condition in which cholesterol plaques are deposited in the walls of arteries, which can restrict blood flow through the vessel. If this occurs in the heart arteries, damage to the heart muscle occurs (myocardial infarction), and blockage of the brain vessels leads to a stroke - an acute circulatory disorder in the brain.
- Increased levels of potassium in the blood (hyperkalemia) can lead to arrhythmia, an abnormal heart rhythm that threatens the patient's life.
- A decreased immune response makes the patient more vulnerable to infections and other diseases.
- Restless legs syndrome. A condition associated with unpleasant sensations in the legs, which force a person to constantly move them.
- Complications of pregnancy that are dangerous for the fetus and mother.
In most cases, chronic renal failure progresses steadily and irreversibly until the terminal stage. The rate of this progression varies between patients. The disease progresses more quickly in individuals with a very low level of glomerular filtration, in young men, as well as in those who excrete a lot of protein in their urine.
A timely diagnosis and adequate treatment can significantly prolong the life of patients with chronic renal failure.
Who is at risk?
- Suffering from diabetes.
- Suffering from arterial hypertension - high blood pressure.
- Elderly.
- Suffering from any chronic kidney disease.
- Persons with high cholesterol levels.
- Obese people.
- Smokers.
- Having relatives suffering from chronic renal failure.
Diagnostics
The diagnosis is made on the basis of elevated levels of nitrogenous wastes - creatinine and urea. An ultrasound examination of the kidneys is also required. To clarify the condition of the body and the degree of damage to organs and systems of the body, a wide range of laboratory tests are performed.
Laboratory research
- Urea and creatinine in blood serum. These are nitrogenous wastes (protein breakdown products) that can only be excreted by the body through urine. A progressive increase in creatinine is the main diagnostic sign of chronic renal failure. The level of urea, unlike creatinine, does not always correspond to the severity of renal dysfunction. Recently, to more accurately assess the degree of renal dysfunction, a special indicator has been used - glomerular filtration rate. It is determined using different formulas taking into account the patient’s height, weight and gender.
- General blood analysis.
- Hemoglobin and red blood cells. The level of hemoglobin and red blood cells in chronic renal failure is usually reduced, characterizing the development of anemia.
- Hematocrit Hematocrit is an indicator characterizing blood viscosity and is the ratio of the volume of blood cells to the total volume of blood. In chronic renal failure, the hematocrit is usually significantly reduced.
- Platelets. The number of platelets (blood platelets) is often reduced in chronic renal failure, reflecting an increased tendency to bleed.
- Density of urine. Renal failure is characterized by a significant decrease in urine density.
- Red blood cells. An increase in the level of red blood cells in the urine may indicate glomerulonephritis as a cause of chronic renal failure.
- Leukocytes. A significant number of white blood cells in the urine is a sign of a urinary tract infection.
- Protein. The more protein is excreted in the urine during chronic renal failure, the faster the disease progresses.
- Cylinders. Casts of fragments formed in the lumen of the renal tubules. A characteristic sign of chronic renal failure are waxy casts.
- Triglycerides. In patients with chronic renal failure, the level of triglycerides, a type of fat found in the blood, is especially common.
- Cholesterol. Total cholesterol may be normal, but the content of “good” cholesterol—high-density lipoprotein cholesterol (HDL)—is often reduced and the content of “bad” cholesterol—low-density lipoprotein cholesterol (LDL) is increased.
- Serum calcium and phosphorus. Chronic renal failure is characterized by decreased serum calcium, while phosphorus levels are usually elevated.
- Alkaline phosphatase. Alkaline phosphatase is an enzyme that is found in large quantities in the bile ducts and bone tissue. With chronic renal failure, bone tissue is destroyed, so the amount of alkaline phosphatase in the blood increases due to its bone fraction
- Kidney biopsy. In diagnostically difficult cases, a kidney biopsy may be required - the removal of a small piece of kidney tissue, which is examined under a microscope, which makes it possible to identify the characteristic signs of chronic renal failure - replacement of the kidney glomeruli with scar tissue.
Other research methods
- Ultrasound examination (ultrasound) of the kidneys. With chronic renal failure, there is a decrease in the kidneys (wrinkling) along with thinning of their outer layer. Ultrasound can also be used to detect kidney tumors, stones or cysts.
- Computed tomography (CT) and magnetic resonance imaging (MRI) of the abdominal cavity. The studies are more sensitive than ultrasound. They allow you to detect tumors, cysts and stones up to 5 mm in size.
Treatment
Chronic renal failure cannot be cured, but its progression can be slowed or even stopped. Treatment is given to relieve symptoms and prevent complications.
Strict blood pressure control is indicated for all patients with chronic renal failure; patients with diabetes need to maintain blood glucose levels within normal limits. Typically, lowering cholesterol levels with statin drugs is required.
It is recommended to limit the intake of salt and proteins, foods rich in potassium.
To treat anemia, erythropoietin is prescribed, an artificial analogue of the hormone that stimulates the formation of red blood cells, sometimes together with iron supplements. Red blood cell transfusions are rarely required.
It is usually necessary to prescribe vitamin D to improve bone metabolism, as well as calcium salts, which bind excess phosphates in the blood.
Typically, most patients also receive diuretics.
The dose of drugs excreted through the kidneys in the urine requires adjustment in chronic renal failure.
If there is a significant decrease in kidney function, hemodialysis is performed - mechanical filtration of the patient’s blood using an “artificial kidney” apparatus.
Prevention
- Losing excess weight.
- Normalization of cholesterol levels in the blood.
- To give up smoking.
- Observation by a doctor and strict adherence to prescriptions if you have diabetes, high blood pressure or kidney disease.
Recommended tests
- General blood analysis
- General urine analysis with microscopy
- Serum creatinine
- Urea in serum
- Biochemical parameters - lipid profile
- Serum iron
- Iron binding capacity of serum
- Ferritin
- Total alkaline phosphatase
- Rehberg test (endogenous creatinine clearance)
- Potassium, sodium, chlorine in serum
- Serum calcium
- Serum phosphorus
- Erythropoietin
- Parathyroid hormone, intact
- Vitamin D, 25-hydroxy (calciferol)
Literature
- Corey Foster, Neville F. Mistry, Parvin F. Peddi, Shivak Sharma, The Washington Manual of Medical Therapeuticts (33rd ed.). Lippincott Williams & Wilkins Philadelphia, 2010.
- Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill Medical Publishing Division, 2011.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, classification and stratification. Am J Kidney Dis 39 (suppl 1), 2000.
- Meyer TW et al: Uremia. N Engl J Med 357:1316, 2007.