Kinds
Depending on the cause of development, primary idiopathic nephrotic syndrome and secondary glomerulopathies are distinguished. The following types of primary idiopathic nephrotic syndrome are distinguished:
- minimal change disease;
- membranous glomerulopathy;
- focal segmental glomerulosclerosis;
- membrane-proliferative (mesangiocapillary) glomerulonephritis;
- other proliferative glomerulonephritis.
Secondary nephrotic syndrome occurs within the framework of the following pathology:
- Infections (infectious endocarditis, syphilis, leprosy, hepatitis B and C, mononucleosis, cytomegalovirus infection, chickenpox, HIV, malaria, toxoplasmosis, schistosomiasis);
- Use of medications and narcotic drugs (gold preparations, penicillamine, bismuth preparations, lithium, probenecid, high doses of captopril, paramethadone, heroin);
- Systemic diseases (systemic lupus erythematosus, Sharpe's syndrome, rheumatoid arthritis, dermatomyositis, Henoch-Schönlein purpura, primary and secondary amyloidosis, polyarteritis, Takayasu's syndrome, Goodpasture's syndrome, dermatitis herpetiformis, Sjögren's syndrome, sarcoidosis, cryoglobulinemia, ulcerative colitis;
- Metabolic disorders (diabetes mellitus, hypothyroidism, familial Mediterranean fever);
- Malignant neoplasms (Hodgkin's disease, non-Hodgkin's lymphoma, chronic lymphocytic leukemia, multiple myeloma, malignant melanoma, carcinoma of the lung, colon, stomach, breast, cervix, ovary, thyroid and kidney);
- Allergic reactions (insect bites, hay fever, serum sickness);
- Congenital diseases (Alport syndrome, Fabry disease, sickle cell anemia, alpha1-antitrypsin deficiency).
Nephrotic syndrome can sometimes develop in patients suffering from preeclampsia, IgA nephropathy, and renal artery stenosis.
The morphological classification of nephrotic syndrome according to the ICD includes the following forms of kidney pathology:
- minor glomerular disorders;
- focal and segmental glomerular damage;
- membranous glomerulonephritis;
- mesangial proliferative glomerulonephritis;
- diffuse endocapillary proliferative glomerulonephritis;
- diffuse mesangiocapillary (membranoproliferative) glomerulonephritis;
- dense sediment disease;
- diffuse crescentic glomerulonephritis;
- Kidney amyloidosis.
According to the activity of the process, complete, partial remission and relapse are distinguished - newly emerging proteinuria after complete remission or an increase after partial remission.
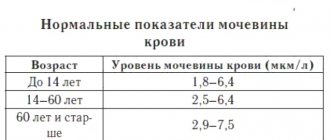
Determination of the state of kidney function in nephrotic syndrome is based on 2 indicators: glomerular filtration rate and signs of renal damage. Kidney damage is structural and functional changes in the kidneys that are detected by blood tests, urine tests, or imaging tests.
Sources
- Nephrotic syndrome /N. Jaipaul. – 2019
- Clinical guidelines for providing medical care to children with nephrotic syndrome /A. A. Baranov. – 2015.
- Nephrotic syndrome. Textbook / L.E. Rudakova, F.K. Rakhmatullov. Penza State University. – 2011.
- Proteinuria and nephrotic syndrome / Yu. S. Milovanov. – 2009.
- Differential diagnosis for nephrotic syndrome /Mironova N.A., Aleutskaya O.N., Kornilov L.Ya. – 2013.
- Nephrotic syndrome in children: definition and principles of therapy / S. V. Belmer, A. V. Malkoch. – 2004.
Causes
Some people substitute the concepts nephrotic and nephritic syndrome. In medicine, these concepts are divided. Thus, nephrotic syndrome is characterized by kidney damage. With nephritic syndrome, an inflammatory process and other associated symptoms develop.
The development of nephritic syndrome is associated with the penetration of antigens from the blood into the renal structures. After their penetration into the kidneys, immune mechanisms are activated, and an immune response to the foreign body occurs. Nephritic syndrome can develop due to the following reasons:
- viral or bacterial infection;
- autoimmune diseases;
- the effect of radiation;
- after administration of a vaccine or serum;
- tumor development;
- toxic effects after drinking alcohol or taking drugs;
- vascular damage due to diabetes;
- intoxication of the body with chemicals of various classes;
- chronic pathologies of the urinary tract;
- increased physical activity;
- sudden changes in air temperature.
Nephritic syndrome can develop both against the background of an inflammatory process and non-infectious disorders - depending on this, treatment tactics are developed.
The multidisciplinary Yusupov Hospital employs experienced specialists who accompany the patient during the treatment process. Thus, if this syndrome is of an autoimmune nature, consultation with a rheumatologist is necessary. Make an appointment
Prevention
The development of nephrotic syndrome can be predicted if relatives (parents) have already had a similar diagnosis. Also, pathology is inevitable if the patient suffers from systemic diseases, diseases of the urinary system, especially pyelonephritis, acute or chronic renal failure.
Therefore, nephrologists advise for prevention:
- Follow the recommendations of doctors when treating infectious and non-infectious diseases.
- Do not self-medicate, do not use antibiotics or hormonal drugs unnecessarily.
- Complete medical examinations and examinations on time.
The information is provided for informational purposes only! If you have questions, we recommend scheduling a consultation with a urologist.
Symptoms
With nephritic syndrome, patients with typical complaints come to the Yusupov Hospital. Signs of nephritic syndrome are:
- the appearance of blood in the urine;
- change in the color of urine - it becomes purple;
- the formation of edema, the most pronounced swelling of the face, eyelids, legs in the evening;
- feeling of thirst and slow urine production.
- A pathological process in the kidneys can cause the following symptoms in patients:
- weakness, nausea;
- pain in the lumbar region that appears at night;
- headaches that appear when the body weakens;
- signs of infectious respiratory diseases;
- Body temperature rises extremely rarely.
Acute nephritic syndrome develops 7-10 days after exposure to a provoking factor or infection. When the first signs of pathological kidney function appear, you should use the services of specialists from the Yusupov Hospital and visit the diagnostic class=”aligncenter” width=”1024″ height=”682″[/img]
Forms of nephrotic syndrome
It is also worth noting three forms of the syndrome, including:
- Relapsing syndrome. This form of the disease is characterized by frequent alternation between exacerbations of the syndrome and its remission. In this case, remission can be achieved through drug therapy, or it happens spontaneously. However, spontaneous remission is observed quite rarely and mainly in childhood. Recurrent nephrotic syndrome accounts for up to 20% of all cases of the disease. Remissions can be quite long in duration and sometimes reach 10 years.
- Persistent syndrome. This form of the disease is the most common and occurs in 50% of cases. The course of the syndrome is sluggish, slow, but constantly progressive. Stable remission cannot be achieved even with persistent therapy, and after about 8-10 years the patient develops renal failure.
- Progressive syndrome. This form of the disease is distinguished by the fact that nephrotic syndrome develops quickly and can lead to chronic renal failure within 1-3 years.
Diagnostics
During an outpatient examination of patients with nephrotic syndrome, doctors at the Yusupov Hospital carry out the following basic diagnostic measures:
- clinical blood test;
- general urine analysis;
- biochemical blood test (total protein, albumin, urea, creatinine, K, Na, Ca, glucose and cholesterol levels in blood serum);
- calculation of glomerular filtration rate using the Cockcroft-Gault formula;
- enzyme immunoassay for viral hepatitis B and C;
- blood test for HIV;
- Ultrasound examination of the kidneys and abdominal organs.
Additional diagnostic examinations that are carried out on an outpatient basis include daily proteinuria or protein/creatinine, albumin/creatinine ratios, immunological methods for studying blood serum, and determining the concentration of Cyclosporin-A in the blood serum.
If necessary, a computed tomography scan can be performed. Upon admission of a patient to the therapy clinic, nephrologists at the Yusupov Hospital prescribe the following mandatory diagnostic examinations:
- kidney biopsy;
- complete blood count (before and after kidney biopsy);
- general urinalysis (before and after kidney biopsy);
- daily proteinuria or protein/creatinine, albumin/creatinine ratios;
- ultrasound examination of the kidneys (after biopsy);
- coagulogram;
- morphological diagnosis of kidney tissue biopsy;
- immunohistochemistry.
Patients have the opportunity to undergo complex studies at partner clinics located in Moscow.
Additional diagnostic examinations that are carried out at the hospital level include electron microscopy of kidney tissue biopsy, determination of cryoglobulins in blood serum, electrophoresis of urine proteins, immunofixation of blood proteins for paraproteins, determination of the concentration of Cyclosporin-A in blood serum. If necessary, sternal puncture, fibroendogastroscopy, colonoscopy, and radiography of the flat bones of the skull can be performed. According to indications, computed tomography, Doppler ultrasound scanning of renal vessels is performed, and the level of tumor markers in biological fluids is determined. If a toxic origin of nephrotic syndrome is suspected, the presence and concentration of bismuth, lithium, paramethadone, and heroin in the blood are determined.
The patient is advised by specialized specialists depending on the suspected cause of nephrotic syndrome:
- oncologist - if paraneoplastic nephropathy is suspected;
- phthisiatrician – if a specific process is suspected;
- rheumatologist – if a systemic disease is suspected.
An ophthalmologist examines the fundus of the eye. The surgeon is invited for a consultation in case of nephrotic crises to exclude acute surgical pathology. A consultation with a neurologist is prescribed if neurolupus or systemic vasculitis is suspected. A hematologist examines patients with suspected multiple myeloma, a light chain disease. If a patient with nephrotic syndrome has a prolonged fever, he or she is consulted by an infectious disease specialist. Differential diagnosis of nephrotic syndrome is carried out with diseases that occur with severe edematous syndrome: liver cirrhosis, congestive chronic heart failure.
Pathogenesis
Hypoproteinemia (decreased blood protein levels) is the main cause of edema. It, in turn, develops due to the loss of proteins (primarily albumin) in the urine. This occurs due to increased permeability of the glomerular filter . Hypoproteinemia causes a decrease in plasma pressure, and the liquid part of it passes into the tissues and lingers in them, causing the development of edema. The condition of the lymphatic capillaries plays a role in the occurrence of edema. Increased filling of tissue with fluid causes a compensatory increase in lymphatic drainage, while tissue proteins are also removed with lymph. This reduces the pressure of the interstitial fluid. As plasma volume decreases, the renin-angiotensin-aldosterone system and antidiuretic hormone . As a result, sodium retention occurs in the renal tubules, which leads to the maintenance and further spread of edema.
The mechanism of toxic kidney damage is associated with the direct toxic effect of poisons on kidney tissue. Mostly the proximal parts of the nephron are affected, in which reabsorption of toxic substances occurs. Dystrophic and degenerative changes (even necrosis) develop in the tubular epithelium. In parallel, there is a disorder of renal hemodynamics in the kidneys - blood flow in the organ is significantly reduced, which causes a decrease in filtration and spasm of the arteries of the renal cortex.
Poor circulation leads to ischemia of the organ, and its consequence is damage to the tubules (up to necrosis) and destruction of the glomerular membrane. As a result of organ ischemia and tubular necrosis, swelling of the kidney tissue itself develops. Renal vascular spasm coagulopathy due to poisoning lead to the development of diffuse intravascular coagulation.
Treatment
Treatment of nephritic syndrome has the following goals:
- achieving weakening or disappearance of signs of the disease;
- elimination of extrarenal symptoms (arterial hypertension, edema) and complications (electrolyte disturbances, infection, nephrotic crisis);
- slowing the progression of chronic kidney disease and delaying its terminal stage with the help of dialysis and kidney transplantation.
The patient, depending on the severity of nephrotic syndrome, is recommended free or bed rest (if the patient’s condition is serious and there are complications). Dosed physical activity – 30 minutes 5 times a week. Doctors recommend that patients stop smoking and drinking alcohol. The diet is balanced, with an adequate amount of protein (1.5-2g/kg), caloric intake according to age. In the presence of arterial hypertension and edema, limit the use of table salt (less than 1-2g per day).
Pathogenetic therapy after establishing a morphological diagnosis begins in the therapy clinic and continues on an outpatient basis. Significant edema is treated with diuretics. Diuretics are not prescribed for diarrhea, vomiting, or hypovolemia. For long-term edema, furosemide is prescribed intravenously as a single bolus or torasemide orally. To treat patients with refractory edema, a combination of loop and thiazide-like or potassium-sparing diuretics is used. If there is a high risk of developing nephrotic crisis, a combination of albumin and diuretics is used.
If the patient experiences resistant edema in combination with renal failure in the acute period of nephrotic syndrome, hemodialysis with ultrafiltration is performed until the critical state of renal failure is eliminated and diuresis appears.
Cardiologists at the Yusupov Hospital take a differentiated approach to the choice of treatment method for patients with nephritic syndrome. In the absence of symptoms of acute kidney injury, ACE inhibitors or angiotensin AT1 receptor blockers are prescribed for antihypertensive purposes, but not in combination. If high blood pressure persists, calcium channel blockers are used. If the patient has a rapid pulse or there are signs of chronic heart failure, beta blockers are additionally prescribed.
Pathogenetic therapy of nephritic syndrome depends on the morphological variant. It is prescribed only after a kidney biopsy and clarification of the morphological diagnosis.
When treating the disease, the disease that caused the nephrotic syndrome is also treated. If parasites or helminths are detected, antiparasitic (anthelminthic) drugs are prescribed. Patients with neoplasms undergo chemotherapy, radiation treatment, and surgery. For diabetic nephropathy, endocrinologists treat diabetes mellitus, nephrologists prescribe drugs that have a nephroprotective effect.
At the onset of nephrotic syndrome, patients are prescribed methylprednisolone or prednisolone. Upon achieving complete or partial remission, the dose of prednisolone is gradually reduced.
Patients who do not achieve complete or partial remission after taking a full dose of prednisolone for 16 weeks are defined as steroid-resistant. They are treated with combination therapy with cyclosporine-A and a minimal dose of prednisolone.
50-75% of patients with nephrotic syndrome who respond to steroid therapy experience relapses. If nephrotic syndrome reoccurs, prednisolone is prescribed. If relapses occur three or more times within one year or there is a steroid-dependent form, combination therapy with low doses of prednisolone in combination with one of the following groups of drugs is used:
- alkylating agents;
- calcineurin inhibitors;
- antimetabolites.
Patients with nephrotic syndrome and chronic kidney disease are prescribed statins. For resistant nephrotic syndrome, rituximab is used. Treatment of nephrotic syndrome in systemic lupus erythematosus is carried out depending on the class of lupus nephritis.
The pathogenetic treatment started in the therapy clinic is continued in the patient’s outpatient and home settings under monthly monitoring of the results of laboratory data (clinical blood test, general urine test, biochemical blood test). Proteinuria levels are monitored using test strips once every 1-2 weeks, and patients regularly measure blood pressure. If the amount of proteins in the urine increases, the protein/creatinine ratio is determined and immunosuppressive therapy is adjusted. If the patient does not respond to immunosuppressive therapy, a repeat kidney biopsy is performed in a therapy clinic.
If the cause of nephrotic syndrome is infectious diseases, antibiotic therapy is administered. Drugs are selected for each patient individually depending on the type of infectious agent. At a high risk of arterial and venous thrombosis, low molecular weight heparins are administered subcutaneously for a long time.
Diet
Patients are advised to limit salt for edema and high blood pressure. Animal products (meat and fish) also contain sodium chloride , so in the acute period they are excluded from the diet, but it must be borne in mind that long-term protein restriction is also bad. The optimal protein intake is 1 g per kg of weight. During the period of exacerbation Diet No. 7 , and in the remission stage, nutrition can correspond to Table No. 5 .