Is an allergy to cow's milk treated in a child, what to give to a bottle-fed allergic baby and what should a mother do if her breast milk causes an allergic reaction in the child - these and other popular questions from mothers are answered by Doctor of Medical Sciences, Professor of the Department of Pediatrics with a course Polyclinic Pediatrics named after. Academician G.N. Speransky Federal State Budgetary Educational Institution of Further Professional Education RMANPO of the Ministry of Health of Russia Irina Nikolaevna Kholodova.
— Irina Nikolaevna, how can you understand that a newborn or a 1.5-2 year old child has an allergy?
— I would like to draw the attention of parents to the fact that if there are people in the family who suffer from allergies, then, of course, the likelihood of allergies in the child will be quite high. For example, if only the mother suffers from it and all allergy sufferers are on the mother’s side, then the probability of an allergy is 40-50%, and if on both the mother’s and father’s side, then it is already 80%. That is, allergies are inherited
and in a child it can manifest itself from the first days of life. In young children, skin and gastrointestinal forms of allergies are most common.
Skin allergy
In young children, it is the cutaneous form that predominates (previously it was called exudative-catarrhal diathesis, now it is called atopic dermatitis) - an allergic rash appears on the child’s body. This can be a dry or wet rash, most often with itching.
Gastrointestinal form of allergy
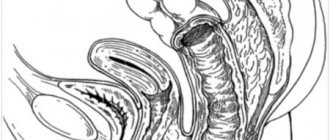
This form is more difficult to diagnose, and it can be very difficult to understand that it is an allergy. Such children may experience severe colic from the first days of life - food is poorly digested, under-oxidized products are formed that irritate the gastrointestinal mucosa and can cause inflammation. In addition, due to impaired fermentation of food, a large amount of gases is formed. Gases stretch the intestines and put pressure on nerves and blood vessels. All this causes spasm and pain.
Subsequently, changes in the character of the stool may appear - there are constipation, but most often diarrhea occurs. Moreover, stool is usually several times a day, and it can be irritating, with a lot of mucus and even streaks of blood. The child begins to eat poorly, there is poor weight gain, and subsequently there may be a slowdown in growth. In such a situation, it is necessary to hospitalize the child to determine the cause - it can be not only an allergy, but also other diseases.
Is milk not for everyone?
The main task of the immune system is to recognize “self” and “foreign” cells. It reacts mainly to substances of protein nature, forming either a “Friend” (so-called immunological tolerance) or “Enemy” (antigen) response. When the response is “Enemy,” specific substances (antibodies) are produced that are aimed at fighting it. But, as with any system, there are failures.
Allergy (atopy) is an example of one such failure, when even friends are blacklisted. The child’s immune system begins to react to BCM inappropriately and excessively, blacklisting it. Beneficial protein turns into an allergen. This reaction is called "hypersensitivity."
The reasons for the occurrence of such “problems” are not reliably known to anyone. Scientists only build hypotheses, accumulate and systematize knowledge. All experts agree that genetic predisposition plays an important role. The only way to break the vicious circle of allergies and help a person is to exclude the causally significant allergen from the diet (environment) of this person.
This is called elimination (and elimination measures).
Causes of lactose allergy
The causes of an allergy to lactose (milk sugar) may be as follows:
Genetic heredity means that a hypersensitive reaction is formed in the human body to the intake of substances into the body that serve as irritants.
Malfunctions of the immune system when specific immunoglobulin E is produced in large quantities.
If the enzyme that is responsible for processing the protein contained in milk is not present in the patient’s body or is present, but in too small an amount, then the human body will react to the proteins as a foreign substance and react accordingly.
Atopic diseases. How to suspect them?
Often people don’t even know about the diagnoses listed above because they don’t see a doctor.
The following symptoms should alert you:
- seasonal nasal congestion or runny nose with copious mucus production
- occasional lacrimation
- bouts of coughing and sneezing
- prolonged dry cough
- bouts of difficulty breathing
- wheezing
- rashes, redness and itching of the skin
- skin prone to dryness and flaking (periods or after contact with something)
- redness and/or other skin reaction to sun or cold exposure
- skin irritation after contact with something
- reactions to insect bites
- reactions to drugs
If the above symptoms occur, then there is a high probability of atopy. In this case, it is better to seek advice from a specialist. If you have allergies, be sure to tell your pediatrician about it and monitor your child’s diet.
Diagnosis of milk allergy
Today, pharmaceutical companies actively advertise anti-allergy products, which is why the vast majority of people choose not to visit a doctor. Such negligence causes addiction to medications, and often provokes complications. The symptoms of the pathology are so extensive that it is almost impossible to diagnose the disease without the participation of an experienced doctor. Some people don't even realize they may have a milk allergy, so they mistake the signs of an allergic reaction for a cold or an upset stomach.
Diagnosis of the disease is carried out by an allergist, an allergist-immunologist, and in children - by a pediatrician. Milk allergy is determined by clinical manifestations, data regarding the patient's diet and laboratory results. The doctor interviews the patient, studies his outpatient card and conducts an examination. To determine the type of allergic reaction and prescribe the correct treatment, the doctor performs laboratory diagnostics. Research is aimed at identifying the allergen. There are two main methods used for this:
- skin allergy tests;
- immunogram.
Skin tests are prescribed for adults and children over 3 years old, subject to a mild allergic reaction. The allergen is injected with a needle under the skin or applied to the wrist. The result is assessed within 24 hours. If after a specified period of time the skin turns red or becomes covered with a rash, the patient is diagnosed with a milk allergy.
An immunogram involves taking the patient’s venous blood and then sending the sample to the laboratory. Under artificial conditions, the suspected allergen is injected into a test tube with blood. Monitoring of processes occurring at the cellular level is carried out using reagents and a microscope.
False allergy or lactose allergy is diagnosed in a slightly different way. Since it is not associated with the production of histamine, skin tests and immunograms are ineffective in this case. A patient with signs of lactose intolerance is advised to consult an allergist or gastroenterologist. After the examination, the doctor will prescribe the following procedures to the patient:
- coprogram (stool analysis) for the presence of lactic acid;
- urine and blood tests to determine galactose levels;
- genetic blood test;
- endoscopy.
Is it possible to prevent the development of ABCM?
Yes.
During pregnancy, the process of “friend/foe” recognition begins. The future mother’s nutrition plays a significant role in this. Products containing choline, methionine, zinc, folic acid, vitamins B6 and B12 can regulate gene function and contribute to the formation of tolerance (body resistance) to CMP.
During breastfeeding, you can limit the consumption of dairy products and other obligate allergens. This will reduce the burden on the child’s body and will also contribute to the formation of an adequate response of the immune system to BCM.
Obligate allergens are foods that often cause allergic reactions: eggs, fish, seafood, legumes: peas, beans, soy, peanuts; nuts, honey, strawberries, pomegranate, kiwi, melon, black currant, mushrooms.
If supplementary feeding is needed?
In the first three months, all children, regardless of the degree of risk of developing CM, are recommended to use only mixtures with specially prepared protein. Their degree of allergenicity is significantly reduced, which is why they are called hypoallergenic. The NutrilakPremium Hypoallergenic mixture is additionally enriched with probiotics and food substrate for their growth and development (prebiotics). The NutrilakPremium Hypoallergenic fat component in combination with lutein best provides all the needs for the development of the child’s brain, vision and motor skills.
Allergy to milk in a child
When a child has a milk allergy, the disease process is accompanied by the same symptoms as in adults. If a child is allergic to milk protein, which is found in dairy products such as milk (breast milk), cottage cheese, cheese, yogurt, kefir, etc., then he may be more capricious, and may also be delayed in growth and development ( This is due to the fact that he does not receive the necessary amount of nutrients for this). In addition, he may have loose stools or burp after feeding. It is much easier to understand that milk is the cause of an allergic disease when the sick person is a child. Because unlike an adult, whose diet should still be checked for the presence of possible irritants, a child may develop a milk allergy immediately during breastfeeding. It is worth adding that over time in young children, milk allergy goes away, remaining in adulthood in only 1% of those affected.
If a child exhibits the above symptoms, he should be immediately taken to a specialist. In order to find out whether there is an allergy specifically to milk, and, as a possible consequence, to dairy products, the following procedures can be carried out: skin allergy tests are performed to check the blood for the content of immunoglobulins; To check the blood for antibodies, it is analyzed.
The presence of such an allergic disease creates a lot of inconvenience for the patient, especially if it is a small child. They are recommended to eat milk substitutes that are designed specifically for allergy sufferers. This milk contains milk of plant origin and goat's milk, which is completely harmless for your baby, because intolerance to goat's milk is extremely rare. Its important advantage is the fact that its composition is close to that of women. For adults, it is recommended to consume types of milk such as oat, rice, soy and almond. Moreover, for approximately a quarter of people who are allergic to milk protein, soy is also an allergen, so they cannot change milk to soy in their diet. Rice milk does not contain such protein, but its disadvantage is the low level of nutritional and beneficial properties compared to their level in other types of milk.
It is also recommended to replace butter with a product such as margarine. It is worth paying attention to the fact that dairy products contain a large amount of vitamin B. In this regard, if a person excludes dairy products from the list of foods he eats, he must compensate for this. Large amounts of calcium are found in fish, nuts and vegetables. It is strongly recommended that a person who is allergic to milk increase the amount of these products in their diet.
How does an allergy to BCM manifest in a baby?
Symptoms of ABCM can be very different.
With skin lesions:
- the appearance of dry skin, sometimes in the form of plaques
- redness of certain areas of the skin (around the mouth, arms and legs, cheeks, chest and abdomen)
- the appearance of weeping spots and crusts with severe itching
- long lasting diaper rash
Involving the gastrointestinal tract:
- private regurgitation
- colic
- constipation
- diarrhea
- mucus in stool
- blood-streaked stool
- poor appetite and slow weight gain
The mucous membranes of the eyes, nose and respiratory tract may be involved with the following symptoms:
- lacrimation
- prolonged runny nose
- distant wheezes
- paroxysmal cough
All this can also affect the baby’s behavior in the form of:
- irritability
- sleep disorder
- bouts of crying and anxiety
It is important!
If symptoms persist after eliminating the causative allergen from the diet, it may not be a food allergy.
Contact your pediatrician immediately. In this case, a nursing woman needs to return to a balanced diet that includes all foods acceptable in the diet of nursing women (to prevent nutritional deficiencies in both her and the child).
If the baby is on mixed or artificial feeding, then together with the pediatrician it is necessary to decide on the correct selection of nutrition for him.
If the baby is already familiar with complementary feeding products, then together with the doctor, review the menu again. Make changes if necessary. Products containing BCM should be excluded. Keeping a food diary for mother and baby will greatly facilitate the process of finding the allergen and taking measures to eliminate it.
How to confirm the diagnosis of ABCM?
There are not many tests in a doctor's arsenal for this, and there are no gold standards. There is no analysis that can confirm the diagnosis with 100% certainty.
The immunological tests performed can be divided into:
- nonspecific, confirming the allergic nature of inflammation
- specific, indicating the degree of significance of the influence of a particular allergen
Difficulties in diagnosing ACM It is extremely rare that only one allergen (CAM) is the cause, the trigger that triggers inflammation
- Most often these are several allergens at once (polyvalent allergy)
- There is cross-reaction between different groups of products
- If the child is breastfed, immunological tests are difficult to interpret (due to the presence of maternal antibodies in his blood)
Ways to select nutrition for ABCM
It all depends on the severity of the allergic process, existing symptoms, the age of the child and the type of feeding.
Breastfed
It is enough to organize the mother's nutrition.
With mixed feeding
If supplementary feeding is necessary, experts recommend using a mixture with split protein hydrolyzate. Of these, you can consider the Nutrilak Premium Hypoallergenic mixture.
Compared to whole molecules of cow's milk proteins, the allergenicity of its split protein is reduced by 100,000 times. Nutrilak Premium Hypoallergenic is suitable for the prevention of allergies in children at risk and the treatment of mild skin manifestations.
Types of proteins in milk
In general, we can say that milk contains different types of proteins, which determine the nature of a person’s allergic disease.
Casein is a component of all types of milk, as mentioned above. And this means that it is not possible to replace drinking one milk with another if you are allergic to milk.
Whey proteins. Such proteins are sensitive to increased temperature. Accordingly, when milk is boiled, the process of destruction of such proteins occurs. That is why, if it is impossible to consume raw milk, you can safely consume milk that has been boiled.
It is important!
Nutrilak Premium Hypoallergenic contains lactobacilli L.rhamnosus LGG® - this is the most effective and safe probiotic for children from birth, used for the treatment and prevention of atopic dermatitis and eczema.
With artificial feeding
If the baby has pronounced skin manifestations, there are crusts and areas with weeping, or there is persistent heavy regurgitation, streaks of blood in the stool, then only deep hydrolysates (for example, Nutrilak PEPTIDE MCT) or amino acid mixtures can be used from mixtures.
Children over 6 months have a wider choice of food: there is more possibility of using complementary foods and soy mixtures (for example, NutrilakPremium Soya).
Is it possible to outgrow ABCM?
No!
If tolerance has not been formed and hypersensitivity to CMP remains, then the allergic inflammatory process occurs in the background. It may not be as pronounced, but it continues! Gradually, the foundation is laid for the development of chronic pathological diseases, turning into a time bomb.
What else is useful to know?
In the process of forming a reaction to an allergen, not only the response of the immune system is important, but also the background against which it unfolds.
It is known that products such as chocolate, cheese, citrus fruits, vinegar, nuts, marinades, etc. are a source of special substances (histamine liberators). They help maintain allergic inflammation by adding fuel to this fire. Limiting their intake or completely eliminating them will reduce the manifestations of atopy and help alleviate the child’s condition.
The smallest friends are microorganisms. Most of them live in the large intestine. They are our great helpers. Their contribution to curbing allergic reactions and forming the correct response to food is difficult to overestimate. More and more studies are confirming this. And if your own intestinal inhabitants can’t cope with this, then trusted friends – probiotics – can come to the rescue. All over the world, only two microorganisms have the largest evidence base on the antiallergic effect - LGG and BB-12 from Chr. Hansen. One of them even has its own website (https://www.lgg.com/).
Dysbacteriosis
Intestinal dysbiosis does not act as an independent form of the disease. But this clinical concept exists and is currently considered from the standpoint of a syndrome that accompanies many conditions and diseases.
Intestinal dysbiosis is a clinical and laboratory syndrome that occurs in a number of diseases and clinical situations. It is characterized by changes in the qualitative and/or quantitative composition of the microbiota, metabolic and other disorders, accompanied in some people by clinical symptoms of intestinal damage.
There is a concept of “transient dysbiosis” in a newborn. It provides for cases when in the first days of life the child has not yet acquired a sufficient number of intestinal microorganisms in their normal composition. After all, some bacteria are colonized only after two weeks or more, which is reflected in the baby’s stool. In the first 2-3 days after birth, the stool is thick and green, with an unpleasant odor. This is meconium, which contains particles of epidermis, amniotic fluid that the baby swallowed while in the womb. Manifestations of such changes in the nature of stool are transient dysbiosis, that is, a normal phenomenon in the first weeks after birth. Later this will be a pathological process that will bring discomfort to the child.
Symptoms of dysbiosis are constantly associated with the basic functions of intestinal microorganisms. And, of course, the main function is the regulation of intestinal motility. Under the influence of microflora, a large number of prostaglandins are synthesized - bradykinins, which affect the contraction of the intestinal wall. Therefore, when this function is disrupted, children first experience abdominal problems in the form of cramps. This leads to the child becoming restless, whiny, and inactive.