Intestinal adhesions are strands of connective tissue that, growing, connect the intestinal loops to each other and/or to other organs of the abdominal cavity and pelvis. Adhesions seriously impair intestinal function and can lead to volvulus, a decrease in the intestinal lumen and, as a result, intestinal obstruction.
Normally, when any damaged tissue is restored, fibrin threads are formed, but subsequently the resorption mechanism is activated. Adhesions in the intestines form when resorption does not occur or is incomplete. The threads become denser, grow further into organs and tissues, and limit the mobility of the intestinal tube.
Classification
Intestinal adhesions are classified according to the degree of strength and some morphological characteristics. The scale for assessing the severity of the adhesive process is as follows:
- 0 points - no adhesions;
- 1 point - single fusion, membranous structure, without narrowing of the intestinal lumen (divided in a blunt manner);
- 2 points - two adhesions of a loose structure without blood vessels. The intestinal tube is moderately deformed, the lumen is not narrowed (divided in a blunt way, in rare cases sharp);
- 3 points - more than two adhesions. Dense, can grow blood vessels. The intestine is deformed, the lumen is narrowed to 50% (divided only by acute means);
- 4 points - conglomerate of adhesions. They are dense, permeated with blood vessels. The deformation of the intestinal tube is extensive, the lumen is narrowed by more than 50% (they are separated only by an acute method, it is difficult to avoid trauma to the fused organ).
How are adhesions on the female genital organs and infertility related?
The female reproductive system ensures the processes of fertility. However, for conception to be unhindered, all parts of this complex system must function normally and have the correct anatomy.
To understand why adhesions in the fallopian tubes are so dangerous, let's look at the function of each organ of the female reproductive system.
- Ovaries. These organs contain follicles - “houses” in which eggs live. In each menstrual cycle, as a rule, 1 follicle reaches maturity, from which an egg is released in the middle of the cycle. This process is called ovulation. If the ovary is shrouded in adhesions, then rupture of the follicle and the approach of the fallopian tube to it becomes almost impossible. This is the prerequisite for the development of one of the forms of adhesive infertility.
- The fallopian tubes. Their role is to “catch” the egg released from the follicle. If in the middle of the cycle there is a meeting with a sperm, then fertilization occurs in the fallopian tube, from where the blastocyst descends into the uterine cavity. This is why fallopian tube adhesions and pregnancy are closely related to each other. If there are adhesions, then the transport of the fertilized egg into the uterine cavity is disrupted.
- Uterus. Hormonal fluctuations during the menstrual cycle lead to the fact that in the second phase the endometrium undergoes secretory transformation, necessary for successful implantation of the embryo. However, if a woman has had repeated curettage of the uterine cavity, inflammatory processes of the uterus, then normal physiological processes may be disrupted. On the one hand, the endometrium is not properly prepared for implantation, and on the other, synechiae create mechanical obstacles for the attachment of the blastocyst. This is a uterine form of infertility.
The main causes of intestinal adhesions
The most common cause is surgery with dissection of the peritoneum (with the laparoscopic method, complications in the form of adhesions are much lower than with open surgery).
The formation of adhesions is also promoted by:
- abdominal injuries;
- inflammatory processes in the abdominal and pelvic organs;
- infection after rupture of an inflamed organ and leakage of its contents into the abdominal cavity;
- radiation exposure in the treatment of oncology.
Burns (when using laser equipment) can provoke postoperative adhesive processes;
mechanical irritation from talc from surgical gloves or lint from gauze swabs; insufficient blood supply, drying out and overheating of internal tissues; long-term sedentary mode after surgery. Diabetes mellitus, bleeding disorders, infectious diseases, and frequent surgical interventions also increase the risk of adhesions.
Adhesive Disease Clinic
Adhesions formed in the abdominal cavity, regardless of the cause of their occurrence, cause a disorder of normal intestinal motility, which leads to difficulty in emptying the contents of the intestinal loops, causing pain in the abdomen and constipation. Bloating of the intestinal loops creates tension on the fixed omentum, which also gives rise to pain. When the adhesions are pulled, the nerves present in them can also contribute to increased pain. Sometimes adhesions create a constriction of the intestinal loop and cause acute intestinal failure. Due to the fact that the adhesive process can be located in different parts of the abdominal cavity, various organs can be involved in it.
Taking into account the complaints of patients, two clinical forms of adhesive disease can be distinguished:
- Adhesive disease with pain in the abdominal cavity.
- Adhesive disease with periodically recurring attacks of OKN.
Painful sensations during adhesive disease depend, on the one hand, on the irritation of the nervous apparatus of the intestinal loops, and on the other hand, on the irritation of the nervous elements. With adhesive disease, patients may experience pain in various parts of the abdomen, depending on the location of the adhesions, but the patient’s main complaint will be abdominal pain. In this group you can find patients with a relatively calm course of this disease - they have a history of 1-2 laparotomies.
Many patients begin to aggravate due to addiction to narcotic drugs. Abdominal pain can be small, aching in nature, in most cases it is constant pain, sometimes periodically intensifying. The pain often intensifies with physical stress or with errors in diet.
Increased pain forces patients to resort to using heating pads, after which the pain decreases and disappears completely. Along with abdominal pain, patients experience dyspeptic symptoms: nausea, constipation, bloating, etc. Patients of this type do not lose their ability to work, but constant aching pain forces them to often go to the clinic. Prescribing physiotherapeutic procedures in the form of diathermy and iontophoresis improves the condition and reduces pain. Patients can use HBOT, sulfur mud baths, which brings relief for some time.
A number of patients, against the background of constant abdominal pain, periodically experience severe painful attacks that require the administration of drugs. During such attacks, patients are admitted to hospitals, where they undergo a new laparotomy. The appearance of severe pain attacks is associated with great physical stress of the patient or with the consumption of large amounts of food, after nervous disorders.
Patients with frequently recurring attacks of pain become irritated, they develop psychasthenia, lose weight, decrease appetite, and often become drug addicts. Often these patients are harsh, rude, and their ability to work is usually reduced. Contact with such a patient is quite difficult. An objective examination reveals several postoperative scars; upon palpation outside of an attack, the abdomen is soft, usually painless; During a painful attack, a sharp pain is detected in certain parts of the abdomen, and there may be muscle tension. Various painkillers and physiotherapy provide only temporary relief.
The omentum sometimes adheres to the postoperative scar on the anterior abdominal wall and this often leads to pain. The tension of the omentum attached to the scar significantly increases pain when extending the body backwards. If the patient is asked to bend forward, the pain decreases. If there are positive symptoms of omental tension, patients are subject to surgical intervention, the purpose of which is to cut off the greater omentum and its resection.
In adhesive disease with periodically recurring attacks of OKN, along with abdominal pain and constipation, attacks of acute intestinal obstruction with typical clinical symptoms are observed: cramping abdominal pain, vomiting, impaired passage of gases, bloating, postoperative scars on the abdominal wall, palpation reveals some tension in the abdominal muscles, pain in the areas of bloating (P.N. Napalkov said: “the intestines stand like a stake”). Patients in these conditions are excited, Valya's symptom is determined, with a slight shock a splashing noise is detected - Sklyarov's symptom.
Due to the presence of scars on the abdominal wall, intestinal peristalsis is usually not observed. Hepatic dullness may be pushed aside by distended intestinal loops. Auscultation reveals bowel sounds of varying intonation. When examining the rectum, there may not be anything typical: sometimes the ampulla can be swollen, sometimes collapsed (the Obukhov hospital symptom appears quite late).
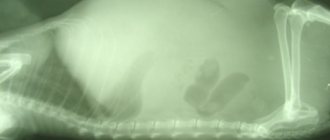
An X-ray examination reveals Kloiber's cups; with a pronounced adhesive process, Kloiber's cups do not move in different positions - a symptom of fixation. In this kind of patients, quite often the symptoms of obstruction are relieved after using the usual measures: a heating pad, a cleansing enema, but if we cannot completely exclude OKN, we need to observe the patient over time - radiologically trace the passage of barium suspension through the gastrointestinal tract. Usually, when a patient is admitted with an unclear clinical picture of OKN, the patient undergoes a survey X-ray of the abdominal cavity and after that they drink about 200 ml of barium suspension and, at an interval of 3 hours, the patient undergoes an X-ray of the abdominal cavity. To speed up the movement of barium, sometimes the suspension is made in very cold water (since cold water enhances peristalsis).
In this type of patient, it is often possible to stop the obstruction and they are discharged, and after a few days they can be admitted again. Such obstruction is often interpreted as dynamic intestinal obstruction of a spastic nature. The use of sedatives eliminates intestinal spasm, thereby restoring its patency. According to many authors, conservative treatment in this group of patients eliminates the symptoms of obstruction in 75% of cases. Surgical intervention for this type of obstruction without the use of conservative measures will be a surgeon’s mistake. At the same time, the surgeon faces a difficult task: is there a mechanical obstruction in this case that cannot be eliminated by conservative measures? A barium test helps here.
To eliminate mechanical obstruction, surgical intervention is necessary. The earlier the intervention is applied, the better the prognosis. We must always remember about the possibility of developing mechanical intestinal obstruction during adhesive disease. To eliminate mechanical intestinal obstruction, emergency surgical intervention is used, the volume of which varies (depending on the amount of intestinal necrosis).
Differential diagnosis of mechanical and dynamic intestinal obstruction is possible with the mandatory use of x-ray examination.
Clinic of adhesive disease in tuberculous peritonitis: as a rule, young people suffer; patients can palpate intestinal conglomerates; during an attack, loud peristalsis can be heard; the onset of pain is often preceded by an abdominal injury or sudden muscle tension. The clinical picture during an attack resembles acute intestinal obstruction with characteristic cramping pain and other symptoms. Some discrepancy between the existing phenomena of obstruction with a clearly expressed dysfunction, and the absence of peristalsis can help in diagnosis. The presence of a tumor formation with a smooth surface and fibrous encysted chronic peritonitis in the abdomen provides significant assistance for recognition - but this does not always happen.
Laboratory data do not provide anything pathognomonic for adhesive disease: ESR may be accelerated, leukocytosis may appear when a painful attack occurs, and the same can be observed with the development of acute intestinal obstruction. To establish a diagnosis of adhesive disease, it is necessary to conduct an X-ray examination of the gastrointestinal tract, since the presence of laparotomies in the anamnesis does not indicate the presence of adhesions in the abdominal cavity. Until recently, laparoscopy was contraindicated, as there is a high risk of damage, but modern endoscopists use laparoscopy for adhesive disease.
X-ray diagnostics is based on the detection in a polypositional study of various types of deformations, unusual fixation, adhesions with the abdominal wall; they study the state of the relief of the mucous membrane, the elasticity of the intestinal walls, especially in the deformation zone: the folds of the mucous membrane, although deformed, do not break off, unlike the tumor process. The adhesive process is not characterized by rigidity of the intestinal wall, which is characteristic of a malignant tumor.
Conservative treatment of adhesive disease: usually adhesive disease has a chronic course, only periodically giving attacks - exacerbation of pain. Therefore, conservative treatment in remission is modified when a painful attack occurs. A painful attack with some gas retention can be stopped with a cleansing enema, heat on the stomach, and antispasmodics. In a hospital setting, epidural blockade of trimecaines has a positive effect. Previously, lumbar blockades according to Vishnevsky were widely used, however
If you have constipation, it is recommended to eat foods that enhance intestinal motility, but not too much. If constipation continues, mild laxatives should be used and regular meals are necessary. You should not eat food that can cause severe bloating - soy food, large amounts of cabbage, milk, etc. Physiotherapeutic procedures should be periodically applied - solar plexus diathermy, paraffin or ozokerite applications on the stomach, iontophoresis, mud therapy can be recommended. Physiotherapeutic procedures must be combined with a diet. If the diet is not followed, physiotherapeutic procedures are ineffective. Heavy physical work should be avoided; muscle tension increases pain. By following a diet, monitoring regular bowel movements, and periodically applying physiotherapeutic procedures, patients with adhesive disease can live tolerably for a long time. But a violation of this lifestyle immediately leads to an exacerbation of adhesive disease.
Make an appointment
Diagnostics
Adhesive processes can be asymptomatic. The doctor should be alerted by complaints of problems with stool (constipation or diarrhea), bloating, belching, early satiety, pain in the intestines, painful bowel movements, infertility in women, a history of abdominal surgery, umbilical hernia.
There are no laboratory tests to determine adhesions. To establish a diagnosis, clinical studies are carried out:
- X-ray with contrast agent;
- ultrasonography;
- CT scan;
- colonoscopy;
- laparoscopy.
Pain with intestinal adhesions and other signs
There are several signs that may indicate the development of the pathological process in question:
- periodic vomiting that occurs regardless of food intake;
- pain in the abdomen or chest cavity;
- chronic constipation;
- violation of the passage of gases.
These are characteristic signs of the adhesive process. Pain from intestinal adhesions may not depend on food intake and increases over time. Symptoms of diaphragmatic adhesions are manifested by pain at the border between the chest and abdominal cavities, impaired excursion (movement) of the diaphragm and difficulty breathing. Clinical symptoms of adhesions in the pelvis may be absent.
Adhesive disease lasts a long time: abdominal pain occurs frequently, then becomes constant, its intensity increases.
Treatment options
The main vector of action in the treatment of intestinal adhesions is the return of the normal location and functionality of intestinal loops by separating adhesions and removing severely affected areas.
It is performed surgically - open or laparoscopic methods. Loose adhesions are separated bluntly, while denser and vascularized adhesions are separated using instruments followed by suturing. If an area of the intestine is irreversibly damaged by adhesions, this conglomerate is completely removed, and the wall is sutured with maximum preservation of the anatomical shape. Areas of affected damaged organs may also be excised.
The use of a nasointestinal tube is indispensable in the treatment of intestinal adhesions. The main objective of using this method is to straighten, eliminate obstruction, and restore normal blood circulation in the intestinal wall. The use of a probe accelerates the healing process, stimulates the return of motility and other functional abilities to the affected intestine. The probe is inserted during the operation jointly by the surgeon and the anesthesiologist through the nasopharynx, esophagus, into the stomach cavity, duodenum and directly into the intestine. It causes some discomfort to the patient, but speeds up recovery. Usually placed for 3-5 days. Maximum 7. The decision to withdraw is made by the attending physician based on observation and the results of clinical studies.
Sources
- Abdominal Adhesions What are abdominal adhesions?, NIH - [https://www.niddk.nih.gov/health-information/digestive-diseases/abdominal-adhesions] (https://www.niddk.nih.gov/health- information/digestive-diseases/abdominal-adhesions)
- Abdominal Adhesions, Medicine Central - [https://im.unboundmedicine.com/medicine/view/5-Minute-Clinical-Consult/117470/all/Abdominal_Adhesions] (https://im.unboundmedicine.com/medicine/view/ 5-Minute-Clinical-Consult/117470/all/Abdominal_Adhesions)
- Alisher Zh. Dairbekov, Zhandos T. Tileuberdi, Nurbolat E. Kuanyshbaev. Prediction and prevention of adhesion formation of the abdominal cavity [Electronic resource] // International Student's Journal of Medicine, 2015.
- Korell M. Methoden der Adhäsionsprophylaxe [Electronic resource] // J GYNÄKOL ENDOKRINOL - 2010.
- Boychuk AV, Kurylo OU, Tolokova TI Prevention Of Adhesions In The Preservation Of Reproductive Health [Electronic resource] // Research Journal of Pharmaceutical, Biological and Chemical Sciences, 2021.
- C. Brochhausen, V. H. Schmitt. Intraperitoneale Adhäsionen [Electronic resource] // BIOmaterialien, 2009.
Consequences of the adhesive process
After treatment, you must monitor your health and follow the doctor’s recommendations. Adhesive processes can recur, therefore, the sooner the patient pays attention to health problems, the greater the chance of eliminating the pathology at an early stage.
Violation of the diet prescribed by the doctor, a sedentary lifestyle, uncontrolled use of medications - all this can provoke new pathological foci.
Symptoms of tubal obstruction
Clinical signs (symptoms) of adhesions in the fallopian tubes are usually absent. It is possible to identify only indirect manifestations, which may indicate an increased risk of adhesions. If a couple fails to become pregnant within 1 year of regular sexual activity, and there are indications of the situations presented below, then an assessment of the patency of the fallopian tubes is mandatory:
- pain in the lower abdomen, especially if they were combined with an increase in body temperature;
- the presence of discharge from the genital tract with an unpleasant odor, which recurs repeatedly;
- pain when examined on a gynecological chair;
- history of surgical interventions on the pelvic organs.
Ultrasound signs of tubal adhesion may include detection of hydrosalpinx, a collection of fluid in the fallopian tubes. This is regarded as a sign of a chronic inflammatory process. There are no other specific manifestations. Normally, the fallopian tubes are not visualized during ultrasound examinations. However, if they are not visible, this does not mean that the organ is functionally complete. Synechiae can develop in the tubes, which almost completely clog their lumen. To objectively assess cross-country ability, special methods are used, which will be discussed below.
Why is it important to see a doctor at the first symptoms?
Adhesive disease is dangerous and often goes unnoticed until it develops into a pathology that is difficult to reverse.
If you have a history of surgeries, abdominal injuries, congenital intestinal abnormalities, or an umbilical hernia, then you should not be ashamed of constipation, bloating and other delicate signs of the disease. You shouldn’t rely on folk remedies either - in the case of adhesions, they will only relieve the symptoms for a short time and give time for the strands to grow even deeper. The Yusupov Hospital provides a full range of medical services, including inpatient treatment, examination, surgery and rehabilitation. Diagnostic procedures of any level of complexity are provided. An individual approach is provided to each patient, which guarantees positive dynamics in treatment.
To make an initial appointment with a specialist, call the numbers listed on the website or fill out a standard online form, leaving contact information for feedback.
What causes adhesions to form in the pelvis
Inflammation of the pelvic organs. The disease is diagnosed in women who have suffered acute inflammation or suffer from chronic:
- colpitis;
- endometritis;
- andexite;
- parametritis and other diseases.
Operations. Adhesive disease appears in 16% of those operated for the first time and in 96% of women after the third operation. The percentage is high for laparotomy operations:
- appendectomy;
- C-section;
- removal of appendages;
- hysterectomy;
- supravaginal amputation.
Pelvic hemorrhages. The trigger is ovarian apoplexy, bleeding due to a ruptured tube during an ectopic pregnancy.
Endometriosis. The formation of fibrinous ties is provoked by endometrioid growths, which spread to the organs and peritoneum of the pelvis.
Pelvic injuries. Open and closed damage after accidents, falls from a height received at work are one of the reasons for the appearance of adhesions.
Predisposing factors. The occurrence and development of the disease is influenced by:
- invasive gynecological interventions;
- promiscuous sex life;
- late visit to the clinic.
How to reduce the risk of formation of adhesions on the fallopian tubes?
The main preventive measures are as follows:
- Prevention of inflammatory processes in the genital organs. To do this, it is recommended to avoid casual sex, use barrier methods of contraception (condom), monitor intimate hygiene and regularly visit a gynecologist for preventive examinations, because Many infections can remain asymptomatic for a long time.
- Reliable contraception to prevent unplanned pregnancy and associated abortions. Today, the most effective and recommended is hormonal protection. A gynecologist will help you choose the most optimal drug.
- If possible, conservative rather than surgical treatment of gynecological diseases. Any operation, even the most gentle laparoscopic one, leaves its mark. Taking into account the individual characteristics of collagen formation, there are categories of women who are distinguished by a pronounced adhesive process that developed after surgery.
For all questions of reproductive health, please contact the SM-Clinic clinic. Our staff includes qualified gynecologists, reproductive specialists and doctors of related specialties who work as a team to help you realize your dream of motherhood. The SM Clinic has introduced advanced diagnostic and treatment methods, incl. use of assisted reproduction methods.