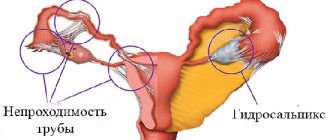
Fallopian tube adhesions are the most common complication of inflammatory gynecological diseases, in which partial or complete obliteration (fusion) of the lumen of the fallopian tube occurs with connective tissue.
Untreated adhesions (synechias) cause obstruction of the uterine (fallopian) tubes, which can lead to infertility, as well as a high risk of developing an ectopic pregnancy. According to medical statistics, every fourth case of female infertility is caused by adhesions of the fallopian tubes.
What are adhesions?
The organs of the abdominal cavity and small pelvis (uterus, fallopian tubes, ovaries, bladder, rectum) are externally covered with a thin shiny membrane - the peritoneum. The smoothness of the peritoneum, combined with a small amount of fluid in the abdominal cavity, ensures good displacement of the intestinal loops, uterus, and fallopian tubes. Therefore, normally, the functioning of the intestines does not interfere with the capture of the egg by the fallopian tube [1], and the growth of the uterus during pregnancy does not interfere with the normal functioning of the intestines and bladder.
Inflammation of the peritoneum - peritonitis - is a very dangerous disease. And the more dangerous it is, the more space it occupies in the abdominal cavity or small pelvis. But there is a mechanism in the body that limits the spread of peritonitis - the formation of adhesions.
With the development of the inflammatory process in the pelvis, the tissues at the site of inflammation become swollen, and the surface of the peritoneum is covered with a sticky coating containing fibrin (the protein that forms the basis of the blood clot). The fibrin film on the surface of the peritoneum at the site of inflammation glues adjacent surfaces to each other, resulting in a mechanical obstacle to the spread of the inflammatory process. After the end of the acute inflammatory process, adhesions in the form of transparent whitish films can form in places where internal organs stick together. These adhesions are called adhesions. The function of adhesions is to protect the body from the spread of a purulent-inflammatory process throughout the abdominal cavity.
The inflammatory process in the abdominal cavity does not always lead to the formation of adhesions. If treatment of adhesions
started on time and carried out correctly, the likelihood of adhesions is reduced. Adhesions form when an acute process becomes chronic and the healing process extends over time.
Adhesions can interfere with the normal functioning of internal organs. Impaired mobility of intestinal loops can lead to intestinal obstruction. Adhesions affecting the fallopian tubes, uterus, and ovaries disrupt the entry of the egg into the fallopian tube, the movement of sperm along the fallopian tube, the meeting of sperm and egg, and the advancement of the embryo after conception to the place of attachment in the uterine cavity. In gynecology, adhesions can cause infertility and pelvic pain.
Complications
The danger is not the spikes themselves, but their consequences. Replacement of functional epithelium with scar tissue is the main cause of infertility.
Depending on the location and organs affected, complications may vary:
- Adhesions between adjacent organs in the pelvis lead to deformation of the organs and loss of their function. There will be pain, discomfort, and difficulty during sexual intercourse. Possible development of infertility, amenorrhea, complications of infectious diseases due to stagnation of secretions.
- Adhesions on the ovaries and fallopian tubes can lead to the development of infertility due to ovulation disorders and amenorrhea. Often, adhesions on the ovaries remain after cyst rupture in the absence of necessary therapy.
- Adhesions in the uterus will lead to disruption of the endometrium during menstruation, recurrent miscarriage and infertility.
The degree of complexity of the situation will depend on the location of the adhesion. For example, if scar tissue is located near the cervical canal, it will make it difficult for blood to flow during menstruation, which can lead to pain and inflammation of the uterus. Seeing a doctor in a timely manner will help avoid possible complications.
Adhesions formed as a result of inflammation
The fallopian tubes, uterus and ovaries can be involved in the adhesive process that occurs during inflammation of neighboring organs (appendicitis - inflammation of the appendix), as well as with lesions of the small and large intestines. In this case, the genital organs themselves suffer little: the adhesive process almost does not disturb their internal structure. If inflammation occurs inside the genital organs, not only the formation of adhesions occurs, but also damage to the genital organs themselves.
The most unprotected in this regard is the fallopian tube - one of the most delicate and finely structured smooth muscle organs. It plays a key role in facilitating conception and supporting early pregnancy.
Sperm entering the vagina are filtered through the mucus of the cervix, pass through the uterine cavity and enter the fallopian tube. Peristalsis - the movement of the fallopian tube - helps sperm enter the outer third (ampull) of the fallopian tube, where the process of conception occurs. During ovulation—the release of an egg from the ovary—the fallopian tube “sucks in” the mature egg. If at the time the egg enters the fallopian tube there are sperm there, fertilization occurs, and the resulting embryo moves to the uterine cavity within a few days, where it is immersed in the uterine mucosa (implantation). Delivery of the embryo into the uterine cavity is ensured by the movements of the fallopian tube and the active work of the microcilia of the fallopian tube.
Thus, the fallopian tube not only ensures the transportation of germ cells and the embryo, but also creates an environment for fertilization and development of the embryo during the first 5-6 days of intrauterine development. A change in the composition of the fluid that is produced in the fallopian tube can destroy the embryo. Local immunity inside the fallopian tube is minimal, that is, there are almost no mechanisms that ensure the rejection of foreign substances, because the embryo is half foreign, the fallopian tube does not reject it, and excessive activity of the immune system is unfavorable for the development of pregnancy. This is why the fallopian tubes so easily become victims of the so-called ascending infection (coming from the vagina and uterine cavity). Surgical and diagnostic interventions in the uterine cavity (abortion, diagnostic curettage, hysteroscopy[2], echohysterosalpingography[3]) facilitate the entry of infection into the fallopian tubes.
Once in the fallopian tubes, the infection first affects the mucous membrane of the fallopian tube (endosalpinx), then the muscular layer (myosalpinx), and only at the last stage the outermost layer of the fallopian tube (perisalpinx) is involved in the inflammatory process and conditions arise for the formation of adhesions. If treatment of adhesions
belated or not effective enough, after recovery not only adhesions remain, but also irreversible damage to the mucous membrane of the tube and its muscle layer. The cilia disappear, and scar tissue forms in place of the smooth muscle fibers. The fallopian tube can turn into a connective tissue sac (sactosalpinx), i.e. it loses the ability to promote a fertilized egg. With such disorders, elimination of adhesions cannot restore the function of the fallopian tube, and the presence of a focus of the inflammatory process leads to a decrease in the likelihood of pregnancy even in the tube from the opposite side or with the help of in vitro fertilization. In such cases, to increase the chances of pregnancy using IVF, which can be performed after recovery, the entire tube has to be removed. As a result of inflammation, gluing and fusion of the walls of the fallopian tube can occur, which leads to obstruction of the tube for the egg and is also an indication for separation of adhesions or removal of the tube.
Adhesion formation after hysterectomy
The risk of adhesions forming after removal of the uterus is high. This problem occurs in almost every operated patient. But the negative consequences of adhesive disease manifest themselves individually. In severe cases, complications such as intestinal obstruction and dysfunction of nearby organs occur.
After removal of the uterus, physiological adhesions form in the form of scars. They do not harm organs if they stop growing and do not turn into fibrous cords. The latter are prone to sprouting into other organs, disrupting their blood circulation, and therefore their function. The only way to get rid of the strands is through repeated surgery.
Adhesion formation in the postoperative period occurs with symptoms, the first of which is nagging pain in the lower abdomen. They are most often periodic in nature, but are so intense that they force you to take painkillers. The patient may develop a high temperature (up to 40C). Painful palpation of the suture also indicates the onset of adhesive processes. There is difficulty urinating and constipation. But none of these symptoms can indicate with absolute certainty an adhesive disease. The final diagnosis is determined only after an instrumental examination and a series of tests.
The first 2-3 weeks of abdominal discomfort and fever may be due to physiological factors of the postoperative period. But if they do not go further, then you need to see a gynecologist.
Postoperative adhesions
During surgical interventions, adhesions are formed due to:
- tissue hypoxia or ischemia - insufficient supply of tissues with blood and oxygen;
- drying tissue during surgery;
- rough manipulation of fabric;
- presence of foreign bodies;
- presence of blood;
- separation of former adhesions.
Foreign bodies that cause adhesions often include talc particles from doctor's gloves, small cotton fibers from gauze or tampons, and suture material. Adhesions also form with endometriosis. During menstruation, a small amount of menstrual blood containing living cells from the lining of the uterus (endometrium) may enter the abdominal cavity through the fallopian tubes. Normally, these cells are removed by the body's own immune system, but if there are any problems, they take root and form functioning endometrial islands that menstruate into the abdominal cavity. Adhesions form around these foci.
Prevention of adhesions
For the prevention and treatment of adhesions, enzyme preparations based on hyaluronidase are used. Perhaps the most popular drug for the treatment of adhesions in gynecology is Longidaza suppositories.
Prevention is mostly aimed at preventing relapses of the disease or before an upcoming operation (since adhesions often appear after them).
Remember that the best prevention is regular visits to the doctor and timely diagnosis. Don’t delay until later and sign up for a pelvic ultrasound or a consultation with a gynecologist.
If you feel acute pain in the abdominal cavity or pelvic organs, do not delay visiting a doctor - prevent the development of the disease. Doctors at the Doctor A clinic will conduct an expert examination and prescribe competent treatment. Call or make an appointment online.
Diagnostics
The presence of adhesions in the abdominal cavity can be suspected in patients who have previously undergone pelvic inflammatory diseases, surgical operations on the pelvic and abdominal organs, and in women suffering from endometriosis. However, only in half of the patients with more than two risk factors for the development of adhesions in the anamnesis, adhesions are detected during laparoscopy (an operation during which small holes are made in the anterior abdominal wall through which an optical device is inserted to examine the cavity and special surgical instruments) .
A gynecological examination suggests the presence of adhesions in the abdominal cavity with a probability of 75%. Obstruction of the fallopian tubes according to hysterosalpingography (a contrast agent is injected into the uterus, X-ray images are taken) and ultrasound examination with a high degree of certainty indicate the presence of adhesions, but the patency of the fallopian tubes does not exclude the presence of adhesions that seriously impede pregnancy. Conventional ultrasound does not reliably detect the presence of pelvic adhesions. Today, the method of nuclear magnetic resonance (NMR, or magnetic resonance imaging, MRI) seems to be very promising in diagnosing the adhesive process. Using this method, images are obtained that reflect the “state of affairs” at different levels.
The main method for diagnosing adhesions is the laparoscopy method. It allows not only to detect the presence of adhesions and assess the severity of the adhesions, but also to treat adhesions
.
There are 3 stages of the adhesive process according to laparoscopy: Stage I: adhesions are located around the fallopian tube, ovary or in another area, but do not interfere with the capture of the egg; Stage II: adhesions are located between the fallopian tube and the ovary or between these organs and other structures and can interfere with the capture of the egg; Stage III: either torsion of the fallopian tube occurs, or it is blocked by adhesions, or a complete blockade of egg capture.
Adhesions in gynecology: symptoms
The adhesive process can be both acute and chronic, or have a periodic nature (with periodic exacerbation of symptoms). Often, women do not notice any symptoms of adhesions in the pelvis, and the disease is discovered only when examining the possible causes of infertility.
Signs of adhesions in the pelvic cavity:
- Painful sensations in the lower abdomen, lower back, above the pubis or in the sacral area;
- Discomfort during physical activity, before menstruation, after stressful situations;
- Pain during sexual intercourse or urination;
- Intestinal disorders: diarrhea, constipation, flatulence;
- Periodic attacks of nausea and vomiting.
Symptoms may worsen when consuming foods that increase gas formation.
Treatment of adhesions
The main method of treating adhesions is laparoscopy . Using special micromanipulators, adhesiolysis - cutting and removing adhesions. Techniques for separating adhesions include laser therapy (cutting adhesions with a laser), aquadissection (cutting adhesions with pressurized water), and electrosurgery (cutting adhesions with an electric knife).
To prevent the formation of new postoperative adhesions during laparoscopy, the following methods can be used:
- introduction into the spaces between anatomical structures of various barrier liquids (dextran, povidin, mineral oils, etc.);
- wrapping the fallopian tubes and ovaries with special polymer absorbable films.
In addition, after laparoscopy, control diagnostic laparoscopy several months after the first laparoscopy has become increasingly common in recent years.
How osteopathy affects adhesions
An osteopathic doctor is able to feel with his hands where the adhesions are located and where they lead, where they are attached and what they are pinching. He is also able to loosen their tension in a few sessions, and can restore, balance and balance damaged organs, and therefore restore their function to the fullest possible extent.
An osteopathic doctor is also able to interrupt the chains of damage and pain in parts of the body that seem to be unrelated to the operated area. After all, our body is an integral system where everything is interconnected. The osteopath acts on the adhesions directly, without violating the integrity of the body tissues, and therefore without an additional factor stimulating the formation of connective tissue. By restoring and harmonizing the function of the suffering organ, the body releases energy to initiate complete recovery in possible individual conditions for the entire organism.
Any surgical intervention, no matter how minimally gentle it may be, leaves behind a lot of negative changes, injuries and stress, which the body is forced to fight alone. What the body will do to heal itself, what it will sacrifice, how it will limit itself is always individual. But within the framework of self-preservation, this is always expressed in loss of function to one degree or another, and therefore subsequent suffering of the entire organism with loss of compensation and the expenditure of much greater effort on normal functioning throughout life.
Therefore, if you have had surgical interventions on the abdominal organs in your life, consult an osteopathic doctor. It does not matter whether the operation was conventional or performed using a gentle laparoscopic method. Any discomfort has a reason, which means there is an opportunity to solve it.
An osteopathic doctor can use pulse diagnostics to determine the significance of adhesions or scars on the body. This means that if, when pressing on a postoperative scar, the properties of your pulse change, then this zone is important and significant for the whole organism, and this adhesion or scar must be worked with.
Adhesions and scars have the following significance and prevalence of influence:
- local (the effect is limited to the area where the scar or adhesions are located);
- regional (the effect extends to the entire thoracic or abdominal region where the commissure is located);
- global (affects the entire body, even to the point of disturbing its position in space).
How long does osteopathic treatment last?
If the patient has undergone surgery, then the osteopathic doctor will tactically act as follows. 10 days after the operation, when the stitches are removed, the doctor will work with the scar itself layer by layer, work with the tissues directly around the scar itself and restore that independent mobility of the organ, which does not depend on the movement of the diaphragm. This period of work ranges from 10 days to 3 months after the operation.
If the duration after surgery is 3 or more months, then the doctor will pay attention to all surrounding organs and tissues in the operation area, influence the mobility of all internal organs in general and directly to the localization of the adhesions themselves.
The information was prepared by the leading specialist of the osteopathy and family medicine clinic Osteo Poly Clinic Gulyants Maria Alexandrovna, osteopathic doctor, chiropractor, endoscopist surgeon.
Prevention
The cellular and molecular mechanisms of adhesion formation are now quite well understood. Therefore, the process of adhesions after surgical operations, including after laparoscopy, can be sharply slowed down using so-called adjuvant (auxiliary) therapy. This therapy should begin as early as possible after the operation (in the first days and hours) and continue for several weeks. Treatment is aimed at suppressing the inflammatory reaction, suppressing fibrin deposition in the abdominal cavity, and activating fibrin dissolution.
Adjuvant therapy includes the use of the following drugs:
- Fibrinolytic agents are substances that dissolve fibrin, around which adhesions are formed: FIBRINOLYSIN, STREPTOKINASE, UROCINASE, HYALURONIDASE, CHEMOTRYPSIN, TRYPSIN, TISSUE ACTIVATORS OF PLASMINOGEN.
- Anticoagulants - drugs that prevent blood clotting: drugs HEPARIN, OXALATES, CITRATES.
- Antibiotics : TETRACYCLINES, CEPHALOSPORINS, SULPHANAMIDES.
- Anti-inflammatory drugs : corticosteroids, antihistamines, non-steroidal anti-inflammatory drugs, progesterone, calcium channel blockers.
The choice of drugs and treatment regimens depends on each specific case and can only be made by the attending physician.
How to treat adhesions in the pelvis
What to do if adhesions are found in the pelvis? Depending on the severity of the adhesive process, the doctor will select the appropriate treatment for you.
To treat single thin adhesions in the pelvis in women, drug therapy is used. What is usually prescribed:
- Antibiotics and antimicrobial agents (to relieve inflammation);
- Non-steroidal anti-inflammatory drugs (as a pain reliever);
- Fibrinolytic agents (for resorption of adhesions);
- Vitamins and immune system regulators (to restore immune balance);
- Hormonal drugs (in cases where adhesions are caused by endometriosis).
Additionally, physiotherapy, balneotherapy and mud therapy may be prescribed as auxiliary measures.
In more severe forms of adhesive disease, a surgical method is used to treat adhesions in the pelvis, i.e. their dissection. The most gentle surgical procedure is manipulative laparoscopy. To prevent re-formation of adhesions, hyaluronic acid is injected into the surgical area.
If treatment for adhesions does not help
Unfortunately, laparoscopy cannot solve all problems associated with adhesions. It is possible to free the internal genital organs from adhesions, but it is impossible to restore the structure and function of the fallopian tubes. Therefore, if pregnancy does not occur within several months after laparoscopy, you should consider switching to more radical methods of treating infertility. In vitro fertilization[4]
(IVF) is one of the most famous methods of in vitro fertilization.
To increase the effectiveness of in vitro fertilization (IVF), the following is taken into account: 1. The presence of sactosalpinxes (limited accumulation of fluid in the fallopian tube) sharply reduces the effectiveness of the IVF method. Sactosalpinxes are removed using laparoscopy. 2. Before the in vitro fertilization (IVF) procedure, it is advisable to undergo a special immunological examination to increase the chances of embryo engraftment.
[1]
The fallopian tube is a thin, hollow tube that extends from the uterus, connecting the uterine cavity to the abdominal cavity. After the egg is released from the ovary into the abdominal cavity, it travels through the fallopian tube into the uterine cavity. [2] Hysteroscopy is the insertion of a special optical device into the uterus, which allows you to examine the uterus from the inside. [3] Hysterosalpingography – injection of an X-ray contrast agent into the uterus and taking a series of X-rays. [4] In vitro fertilization (IVF) is a relatively new method of treating infertility. It was first used in England in 1978. The essence of in vitro fertilization is that the egg is fertilized and develops outside the uterus, and an embryo (sometimes consisting of only a few cells) is transferred into it to bear a child. Tags: infertility
The occurrence of synechiae inside the uterine cavity
Intrauterine adhesions occur mainly due to injury to the mucous membrane during abortion, miscarriage, complicated childbirth, and infectious inflammation. This pathology in gynecology is called Asherman's Syndrome. This disease is characterized by a decrease in the internal volume of the uterus and a deterioration in the quality of endothermy. Asherman's syndrome reduces the ability to conceive and bear a child. The functions of the uterus in this case are hampered by adhesions. With the syndrome, the amount of menstrual flow decreases significantly and may disappear.
The presence of adhesions in the uterine cavity is detected using ultrasound, as well as hysteroscopy. Diagnostic hysteroscopy is considered the most effective, allowing to determine the type of adhesions, their development, and also examine the endometrium. Based on the diagnostic results, the doctor selects treatment methods, taking into account the individual characteristics of each patient.
For Asherman's Syndrome, therapeutic hysteroscopy with excision of synechiae and the prescription of hormonal treatment gives good results. As a result of this operation, the uterus is restored, the endometrium improves to a normal state. The success of treatment largely depends on the degree of endometrial damage. A woman’s chances of becoming pregnant naturally or with the help of assisted reproductive technologies can be assessed already at the diagnostic stage.
Video on the topic
Methods for eliminating synechiae
Medication
It is most often used if a woman does not have severe inflammation and is not planning a pregnancy in the near future. Antibiotics are traditionally used to prevent inflammatory processes. Enzyme preparations, biogenic stimulants and drugs containing placenta can be used to separate and resolve adhesions. To restore and regulate the immune system, patients may be prescribed immunogenesis stimulants.
Expert opinion
Doctors warn: do not self-medicate under any circumstances, it is dangerous to your health! The process of removing adhesions is individual; after a thorough diagnosis, your doctor will select the appropriate medications for you.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Physiotherapy
Physiotherapeutic procedures are especially effective in combination with the drug treatment described above.
The most well-known non-surgical techniques include mud therapy, electrophoresis, and magnetic therapy. Gynecological massage is considered quite effective, stimulating blood flow and destruction of connective tissue in the fallopian tubes.
Physiotherapy has a number of contraindications and can only be prescribed after a detailed examination of the body, so be sure to consult with a physiotherapist before signing up for procedures.
Laparoscopy
Laparoscopy is the most radical method of combating adhesions in the pelvis. It refers to minimally invasive surgical operations. To eliminate synechiae, the surgeon makes several small (up to 1 cm) incisions through which he performs the necessary manipulations.
Due to the slight loss of blood after such an operation and minor surgical trauma, the female reproductive system recovers in approximately 3-7 days.
You should know that there are absolute and relative contraindications to laparoscopy.
Folk remedies
Being one of the key causes of female infertility, synechiae have been known to women for quite a long time. In addition to traditional methods of getting rid of adhesions, there are many folk remedies. Doctors warn that such therapy cannot be the main method of treatment. Of course, the use of one or another folk method requires the approval of a doctor.
Among the medicinal plants, boron uterus, milk thistle, cinquefoil, St. John's wort, sweet clover, centaury and coltsfoot are especially popular.
In various combinations, these plants are infused for oral administration. You can also prepare compresses from flax seeds and herbal decoctions. There is a statement that to get rid of adhesions at the initial stage, a course of 8 procedures is enough for them to all resolve.
Of course, many drugs are produced based on medicinal plants, but talking about their absolute effectiveness is debatable - it all depends on the individual condition of the patient, the quality of the herbs, etc. When treating with folk remedies, it is important to constantly maintain contact with the doctor to prevent complications.
Adhesive disease: when to suspect?
Abdominal adhesions can cause trouble for people who have had abdominal surgery or inflammatory diseases of the abdominal organs.
Manifestations range from minor, rare pain to surgical emergencies. The expert of the Sibmeda portal is Gennady Nikolaevich Tolstykh, Ph.D., Honored Doctor of the Russian Federation, Head of the Department of Surgery of the State Regional Clinical Clinical Hospital. Why do adhesions form?
In surgical practice, adhesive disease of the abdominal cavity refers to a condition when between the internal organs located in the abdominal cavity, jumpers or cords of connective tissue of different types and structures are formed, which are called adhesions.
Initially, this is a protective process, because through the formation of adhesions the body seeks to limit the pathological focus, blocking it. During the normal course of the disease, after a certain time, adhesions disappear, and if they remain, they do not make themselves felt, and patients may not be aware of their existence. But in some cases, the process of adhesion formation becomes redundant. The resulting adhesions of connective tissue begin to affect the function of the organs with which they come into contact, and symptoms of the disease appear. If the adhesive process affects one or another part of the intestine, there will be symptoms of disruption of its functioning, sometimes even to the point of obstruction. Localization of the adhesive process in the pelvis in women can cause deformation and obstruction of the fallopian tubes with infertility.
Causes of adhesive disease
Adhesive disease can develop at any age. Actually, adhesions in the abdominal cavity after surgical interventions develop in 20-80% of patients. Of these, in 2-8% of cases, adhesive disease with characteristic symptoms subsequently develops. It is more common in women - the ratio is 2:1 in relation to men. However, depending on the causative pathology, the ratio changes. For example, adhesive disease after removal of the appendix occurs more often in women - 3:1.
Unfortunately, adhesive disease often accompanies surgical treatment methods, since every operation is a trauma. A doctor, saving a patient from one fatal disease, unwittingly contributes to the emergence of a new disease. Hope in this regard comes from the development of laparoscopic and transluminal surgery. The main causative factor in the formation of adhesions is one or another effect on the peritoneum - the integument lining the abdominal cavity and covering the organs.
Gennady Tolstykh
said:
“Rather, we should talk not about operations, but about diseases that more often lead to adhesive disease of the abdominal cavity. The main causes are injuries to the abdominal cavity when blood enters it. Then come diseases of the abdominal cavity, accompanied by inflammation of the peritoneum, that is, peritonitis. Often these are gynecological inflammatory diseases. Autoimmune diseases also contribute to the appearance of abdominal adhesions. Suppuration of a postoperative wound also sharply increases the risk of developing adhesive disease. If we talk about the consequences of operations on the abdominal cavity, then more often adhesive disease occurs after extensive interventions, as well as after repeated operations. Previously, the percentage method was used, according to which, after the second surgical intervention, the risk of adhesive disease is approximately 20%, after three operations - 30%, after five - already 50%. The main reason is the body’s reaction to traumatic factors, blood in the abdominal cavity, etc.
Of course, careful treatment of tissues during the operation, as little trauma as possible, and careful stoppage of even the slightest bleeding also play a role. Factors such as the presence of intestinal paresis in the postoperative period or a significant increase in intra-abdominal pressure also influence. It is very difficult to predict the appearance of adhesive disease in a particular patient.” Any intervention in the abdominal cavity, accompanied by its opening, to one degree or another leads to injury to the peritoneum. Technical techniques during a surgical operation, especially those performed roughly, can become a trigger for adhesions. When the presence of infection, the presence, especially long-term, of blood in the abdominal cavity, and exposure to air on the peritoneum are added to the mechanical traumatic effect, the risk of adhesions increases significantly. The infectious factor plays a big role, especially unfavorably if the peritoneum becomes infected from the intestinal lumen, for example, during its perforation.
Blood that enters the abdominal cavity during operations, injuries, and is not collected in time, coagulates, blood clots are formed, which subsequently become denser, become organized and cause the appearance of adhesions. If certain foreign bodies enter the abdominal cavity, for example, during surgery or trauma, they provoke inflammation with the formation of granulomas and adhesive connective tissue adhesions.
Adhesions as a result of inflammation
The adhesive process can develop as a result of acute or chronic inflammatory diseases of certain abdominal organs. This process of inflammatory origin is called perivisceritis. The infectious factor and inadequate treatment, including irrational antibiotic therapy, play a role in its development.
For example, with chronic inflammation of the gallbladder, the process can spread to the bladder itself and the duodenum, deforming them and causing dysfunction, bile stagnation, and chronic duodenal obstruction.
The adhesive process in the pelvic area often occurs in connection with chronic inflammatory diseases of the internal genital organs in women. This is the result of the transition of acute inflammation to chronic, which happens in 17–20% of cases. According to the international classification of diseases, adhesive disease in the pelvic area in women is included in a separate section, which indicates the significance of the problem.
There is an increased tendency to adhesions in some patients. The reason is seen in the presence of an autoimmune component during inflammation of the peritoneum. In conditions of damage to the peritoneum by one or another factor in combination with an autoimmune or allergic component, inflammation lasts longer than usual, deeper degenerative changes occur, the balance of the enzyme systems of the peritoneal epithelium is disturbed, which slows down the process of disorganization of adhesions that have begun to form. They continue to develop, become denser, and occupy a larger area. If a person has a tendency to form keloid scars on the skin after some kind of surgery or injury, the likelihood of excessive adhesions increases.
Manifestations of adhesive disease
Adhesive disease can manifest itself with various symptoms: from moderate periodic abdominal pain to acute intestinal obstruction at different levels, when the patient’s life is threatened.
Gennady Tolstykh
clarified:
“With regard to the timing of appearance, adhesive disease is divided into early, if adhesions and the corresponding clinic appear on the 3-7th day after surgery, and late, if more than a month has passed.
Early is acute adhesive intestinal obstruction, which requires emergency measures.” Often the leading complaint is a variety of abdominal pain. The pain can be constant or paroxysmal, cramping, often without a specific localization. The pain is caused by the presence of nerve elements in the adhesions themselves, as well as by stretching of the hollow organs.
If the passage of the small or large intestine is impaired, a feeling of gastrointestinal discomfort is felt, bloating, rumbling, then nausea and vomiting appear. The passage of gases and stools is delayed. Adhesive disease of the abdominal cavity is characterized by repeated attacks of partial or complete intestinal obstruction, followed by periods of normalization of the condition (remission).
Periods of well-being can vary in duration, sometimes months, and sometimes years, if there are no provoking factors, the patient follows the recommendations. Adhesive obstruction can be provoked by unfavorable factors, especially their combination: significant physical effort, dietary errors (significant overeating, consumption of prohibited foods), intestinal infections, for example, gastroenteritis.
With a long and severe course of adhesive disease, somatogenic neuroses may occur, which further aggravate the course of the disease and cause irritability and imbalance. Disorders of the motor-evacuation function of the gastrointestinal tract deepen, which leads to painful symptoms that force such patients to limit themselves in food.
There is a significant loss of body weight, sometimes even exhaustion. Functional disorders of the nervous and cardiovascular systems may be detected. Metabolic parameters change: the amount of albumin and total protein in the blood decreases, which indicates their deficiency, and mineral metabolism worsens.
Diagnosis: by exclusion
To diagnose adhesive disease, the doctor must collect information about previous operations, diseases of the abdominal organs, and find out whether there were postoperative complications or not.
“The main method for diagnosing adhesive disease is the exclusion method.
A number of examinations are carried out to exclude pathological conditions and diseases similar to adhesive disease of the abdominal cavity. First of all, this includes diseases that give a similar pain syndrome in the abdominal cavity - pathology of the gallbladder, kidneys, gynecological diseases, chronic diseases of the small and large intestines, etc. To do this, a set of examinations is performed: ultrasound of the abdominal organs, kidneys, pelvic organs, colonoscopy, examination by a gynecologist, and, if necessary, other related specialists, etc. For more than 100 years, the most reliable method for confirming adhesive disease has been an X-ray examination of the intestine with the passage of a barium suspension through it. Determine the speed of passage (slow, normal, accelerated), places of delay, etc. Treatment of adhesive disease is conservative: physiotherapy, primarily electrophoresis, mud therapy, as well as massage of the anterior abdominal wall, stool regulation, treatment of intestinal dysbiosis.
The operation is performed only after long-term unsuccessful conservative treatment when the fact of severe long-term suffering of the patient has been established ,” the expert said.
Prevention of adhesions and relapses of adhesions
Prevention of adhesions should be carried out by doctors during and after surgery. But to a certain extent, the patient himself can help prevent the formation of adhesions. To do this, it is necessary to follow the doctor’s prescriptions, which may include physiotherapeutic treatment. Abdominal massage and physical therapy are important to strengthen the muscles of the abdominal wall and improve the excursions of the diaphragm. Below are exercises with simple self-massage techniques:
1. Lying on your back with your hands on your stomach, perform abdominal-diaphragmatic breathing: when inhaling, strongly protrude your stomach, when exhaling, pull it in, pressing it from above with your hands.
2. In a sitting position with a straight back, perform abdominal-diaphragmatic breathing: when inhaling, protrude the stomach, when exhaling, retract it, making massaging movements with your hands from right to left along the large intestine.
People with existing problems should strictly follow dietary instructions. Eat in small portions, fractionally, do not eat food that causes gas formation in the intestines. It is useful to periodically carry out courses of physiotherapeutic procedures. They must be combined with a diet, otherwise the effect will be far from obvious. Heavy physical work should be avoided. The use of laxatives is prohibited. Failure to follow the recommendations is fraught with the development of adhesive intestinal obstruction with serious consequences.