Causes
The pathological process most often develops due to the action of several factors. These include:
- Smoking;
- Occupational hazards;
- Unfavorable state of the environment;
- Anomalies in the structure of the upper or lower respiratory tract;
- Frequent colds1.
These factors lead to disruption of mucociliary clearance - a natural mechanism whose function is to cleanse the respiratory tract and bronchi from pathogenic microorganisms and their metabolic products. Exacerbation of chronic obstructive bronchitis can be caused by a viral and, less commonly, bacterial infection.
Basic ways to avoid bronchitis or quickly recover from illness
If you want to prevent the occurrence or development of bronchitis, you should be careful about your health. For example, smokers are advised to quit or reduce the number of cigarettes they smoke. This will reduce the rate of development of COPD and reduce the severity of cough. Playing sports or traveling, especially walking or cycling, will not interfere.
It is recommended to undergo annual vaccination to protect against influenza, as well as pneumonia, which is done once every five years.
How does the disease manifest itself?
Symptoms of obstructive bronchitis appear during its exacerbation. The main complaints include:
- Cough. Most often with the discharge of sputum, during an exacerbation its volume increases.
- Shortness of breath during exercise. The intensity of shortness of breath depends on the severity and level of compensation of the disease. Most often, breathing difficulties are observed during prolonged walking, heavy lifting and other types of activity.
- General weakness, increased fatigue. Typical for people who have been suffering from chronic obstructive bronchitis for a long time.
- Symptoms of hypoxia or lack of oxygen.
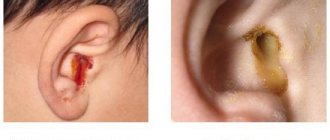
With bacterial inflammation, an increase in body temperature is more often observed, the sputum becomes purulent in nature, and the symptoms of intoxication intensify. Coughing attacks occur mainly at night, during physical activity or due to irritants. There is also acute obstructive bronchitis, which is more violent, but can result in complete recovery. This form is especially common in young children, but with proper treatment it does not leave behind negative consequences. In any case, in order to prevent the development of complications, therapy for obstructive bronchitis should be carried out under the supervision of a medical specialist.
Air barrier. How does obstructive bronchitis occur?
How does obstructive bronchitis occur?
The respiratory tract in childhood suffers most often compared to other organs. They are affected by various viruses and bacteria, resulting in bronchitis. If thick mucus accumulates in the bronchi and it becomes difficult to breathe, then obstruction develops. Neonatologist Ekaterina Sergeevna MOKEEVA (Nizhny Novgorod) told us about what obstructive bronchitis is and what the most effective methods of treating this disease exist.
The essence of obstruction
Bronchial obstruction is a sudden and severe spasm of the bronchi, which occurs under the influence of infectious or non-infectious factors.
The term “obstruction” means a blockage of the bronchi, which prevents air from entering the lungs freely. Anatomically, obstructive bronchitis differs from normal bronchitis in changes in the entire thickness of the bronchus, which leads to its narrowing, swelling and damage to the entire bronchial tree.
Most often, children under 5 years of age suffer from acute obstructive bronchitis, since their bronchopulmonary system is not yet sufficiently developed. The habit of children breathing through their mouth also plays a big role.
Parents should know that in the nasal passages there are special cilia that, like traps, capture the smallest particles of dust, virus and bacteria. Therefore, if the nasal passages are inoperative and the child’s nose does not breathe, then the risk of contracting bronchitis increases many times over.
Picture of the disease
Obstructive bronchitis begins as a common acute respiratory disease, no different from a cold. The child may develop a cough - in the first days of the illness it is not strong and unobtrusive, a runny nose and a sore throat.
As the cough worsens, there is an increase in body temperature, usually up to 38°C. The cough becomes painful, paroxysmal, does not bring relief (the mucus is very viscous and does not separate) and is most annoying at night. Moreover, a cough with obstructive bronchitis can be whistling, dry, or wet, but even in the latter case, sputum is difficult to clear.
By the patient's breathing, you can understand when bronchial spasm is severe: even without a phonendoscope, wheezing, whistling, shortness of breath, and noise can be heard.
Due to allergization of the body by toxins released during the life of pathological bacteria, effusion occurs through the mucous membranes. The mucous membrane swells and thereby reduces the lumen of the bronchi. This gives a picture of obstruction - narrowing.
Next, an inflammatory process begins in the affected bronchi with the release of histamine. Copious, difficult to separate sputum appears. If this condition is not treated, the obstruction will soon become chronic.
A more complex picture emerges with the development of obstructive bronchitis in children against the background of an allergic reaction. The disease begins with a strong cough, accompanied by a characteristic whistle when inhaling. The child becomes lethargic and inactive, complains of weakness and headache. There may also be pain in the chest along the bronchial tree.
Typically, the hallmark of allergic obstructive bronchitis is the connection between the onset of the disease and any changes in the external environment. For example, you purchased a new carpet, furniture, or you got a pet.
The child may develop shortness of breath - rapid and difficult breathing during physical exertion, and in severe cases, at rest. But unlike cardiac dyspnea, the child does not tend to sleep while sitting or take a vertical position - on the contrary, such children sleep better on their stomach, sometimes hanging their head or placing it below body level - this is due to better discharge of sputum in this position.
Causes of the disease
Risk factors for obstructive bronchitis are:
- frequent acute respiratory viral infections;
- lack of outdoor sports activities;
- sedentary lifestyle;
- tendency to allergies;
- weakened immunity.
Infectious factors that can cause bronchial obstruction include rhinoviruses, adenoviruses, and mycoplasma.
Among non-infectious factors, allergies are the most common. Allergens are found in large quantities in sweets, canned foods, various processed foods and drinks. An allergic reaction can be caused by absolutely any drug or any dietary supplement. Allergies to house dust, animal hair, plant pollen, poplar fluff and much more often develop.
Many parents do not react in any way to the frequent skin rashes that appear in a child after eating new foods. They do not pay attention to the seasonal runny nose, motivating their superficial attitude to this problem by the fact that the symptoms of this condition are minimal, and therefore do not require treatment. This is wrong. In the chronic course of even a mild allergic process, there is a risk of increased sensitization (sensitivity) of the body.
Also, non-infectious factors that contribute to the occurrence of obstruction in a child include passive smoking. Parents should remember that tobacco smoke has an extremely negative effect on the child’s body.
Bronchoobstruction is caused by congenital malformations of the bronchi, impaired immunity due to the characteristics of pregnancy and childbirth of the mother (prematurity, fetal hypoxia, birth injuries and early infections).
We clarify the diagnosis
It is not difficult for an experienced pediatrician to identify obstructive bronchitis; just ask about the symptoms of the disease and listen to the baby’s breathing.
The radiograph sometimes (but not always) shows an increased pulmonary pattern. In a general blood test, ESR may be accelerated. If the cause of the disease was an allergy, the number of eosinophils in the child’s blood will be increased.
Effective treatment
For children under 2 years of age, it is advisable to undergo treatment in a hospital setting.
It is necessary to give a sick child a lot to drink (up to 2 - 3 liters of liquid per day). A hypoallergenic diet is required, and nutrition must be nutritious and age-appropriate.
Any store-bought sweets, sweet carbonated drinks, food products containing preservatives and dyes, including milk cheeses and fruit yoghurts, sausages, and citrus fruits should be completely excluded from your baby’s diet. Also, do not give your child smoked foods, limit the consumption of fatty and fried foods. Of the store-bought fruits, offer only green and yellow ones (red and orange are prohibited) that correspond to the area and time of year. Be careful when including honey and other bee products in your menu.
For obstructive bronchitis, the doctor usually prescribes antispasmodics (no-shpu, papaverine), bronchodilators (salbutamol, berodual), expectorants (lazolvan, ambrobene, acetylcysteine), antihistamines (zodak, zyrtek, tavegil).
If you have a nebulizer at home, you can remove mucus by inhalation using expectorant and bronchodilator solutions. In each specific case, the drugs are selected by the doctor.
Antipyretics should be given only when the body temperature exceeds 38.5°C. The optimal drug is paracetamol. Amidopyrine, antipyrine, phenacetin should not be given to children. It is not recommended to use aspirin and analgin - they can have negative side effects.
If the cough has become dry and occurs in attacks, it is possible to use drugs that affect the cough center, such as libexin. You just need to remember that in this case the sputum will be separated poorly and such drugs must be used in its absence.
Vibration (drainage massage) facilitates the discharge of sputum and can be performed by both the nurse and the parents. In this case, the collar area, back, then the chest, respiratory muscles (sternocleidomastoid, intercostal muscles, abdominal muscles) are massaged.
Antibiotics are prescribed in case of secondary bacterial infection. The following symptoms may indicate this: body temperature is above 39°C, lethargy and loss of appetite are observed, weakness and headaches are expressed, in the general blood test the ESR is accelerated and the content of leukocytes is increased.
It is imperative to rinse the nasopharynx with saline solution, Borjomi, preparations based on sea water and products containing silver.
To restore nasal breathing, vasoconstrictor drugs (tizine, oxymetazoline, etc.) are used. Nasal drops cannot be used for a long time - this can lead to atrophy or hypertrophy of the nasal membrane.
Prevention of exacerbations
The most important thing is to understand the cause of the obstruction and try to eliminate it.
If the disease was caused by a viral infection, then you need to strengthen your immune system and take antiviral drugs prescribed by an immunologist during the cold season.
If the culprit of obstructive bronchitis is an allergy, it is necessary to create hypoallergenic living conditions and, if possible, conduct allergy tests.
Protect a child prone to bronchial obstruction from passive smoking and irritating environmental factors (sudden temperature changes, polluted air, dust and mold in the apartment).
And, of course, the baby needs to be hardened in all available ways: a contrast shower, sufficient time in the fresh air, physical education, swimming in the pool are useful.
Ekaterina QUEEN.
Diagnostics
The beginning of diagnosis consists of a thorough collection of complaints and medical history. An informative method is to listen to breathing in the lungs using a phonendoscope. Obstruction is characterized by the presence of scattered dry or moist rales. In addition to the examination, if necessary, the doctor may prescribe additional tests:
- X-ray of the OGK;
- Spirometry;
- General blood analysis;
- Blood biochemistry (to determine markers of inflammation);
- Bacteriological examination of sputum and culture for sensitivity to antibiotics;
- CT or MRI of the lungs to assess the presence and nature of changes in them3.
After making a diagnosis, the doctor should talk about the prevention of exacerbations of obstructive bronchitis and prescribe a course of treatment.
Basic means of diagnosing obstructive bronchitis
To obtain the most accurate diagnosis, it is very important to conduct high-quality diagnostics.
- Computed tomography allows you to immediately exclude diseases that have similar symptoms, such as lung cancer, pneumonia or bronchiectasis;
- Spirometry or FVD is a breathing test that makes it possible to exclude bronchial asthma from a possible list of diseases. With its help, COPD is detected;
- Thanks to blood tests, doctors can detect the presence of an inflammatory process occurring in the body. The degree of activity of microorganisms and viruses that cause inflammation will be determined immediately;
- Using sputum cultures, it is possible to identify bacteria that provoke inflammatory processes in the bronchi.
Treatment
Therapy for obstructive bronchitis should be comprehensive. To reduce obstruction syndrome, bronchodilators are used - drugs that relieve spasm and expand the lumen of the bronchi. This makes breathing easier and eliminates shortness of breath. Medicines that thin mucus and relieve cough are also prescribed. If a bacterial cause of bronchitis is confirmed, a course of antibiotics is necessary to prevent the infection from developing into pneumonia. Antihistamines (antiallergic) drugs are used if the obstruction is caused by an allergic component.
The most effective methods of treating chronic obstructive bronchitis
For treatment, first of all, contact a pulmonologist who will prescribe examination and treatment. At the Integramed respiratory medicine clinic, appointments are conducted by pulmonologists with 20 years of experience. Applicable:
- Therapy carried out with specially developed drugs. First of all, these will be medications that make it possible to dilate the bronchi - bronchodilators. They are used as inhalations. As a result of the effect of the medicine, the bronchi expand, which improves breathing and mucus removal;
- Antibiotics are used that successfully destroy bacteria and viruses that provoke inflammatory processes. Their dosage is prescribed only by a pulmonologist or therapist;
- It is possible to prescribe an oxygen inhalation procedure;
- A vibration massage of the chest will also not be amiss, as it allows for a better effect on the lungs and speeds up the removal of phlegm.
- In some cases, folk remedies can also help. But only in consultation with your doctor and in the indicated doses.
Prevention
To prevent exacerbations of chronic bronchitis, a person must first give up smoking and work in conditions of increased air pollution. An adequate response of local immunity to viruses and bacteria is also very important. If there is no such response, activation of local immunity is required, since the body’s protective factors can eliminate most of the pathogens that lead to bronchitis.
IRS®19 is a drug with an immunomodulatory local effect, which includes a mixture of 18 bacterial lysates. It comes in the form of a nasal spray and acts directly on the nasal mucosa, which is considered the entry point for viruses and bacteria into the respiratory tract4.
IRS®19 activates immune cells of the nasal mucosa and begins to act immediately upon contact with the mucous membrane5. When added to standard symptomatic therapy, IRS®19 reduces the duration of symptoms by 2 times5. The drug is used for the treatment and prevention of respiratory diseases in children and adults from three months.
Causes of bronchitis
Primary obstructive bronchitis in children is often caused by viruses. The following pathogens affect the bronchial tree:
- parainfluenza virus type 3;
- respiratory syncytial virus;
- enterovirus;
- influenza viruses;
- adenoviruses;
- rhinovirus.
Often the manifestation of obstructive bronchitis in a child is preceded by a cold. The disease is repeatedly caused by other pathogens of persistent infections, which include:
- chlamydia;
- mycoplasma;
- herpesvirus;
- pathogens of whooping cough, parawhooping cough;
- cytomegalovirus;
- mold fungi.
Often, with repeated cases, the opportunistic microflora of the respiratory tract is activated. Allergic reactions play a significant role in the development of bronchial inflammation in children. Relapses of obstructive bronchitis are facilitated by infection with worms and foci of chronic infection (sinusitis, tonsillitis, caries). Factors that provoke the development of exacerbations include:
- physical fatigue;
- hypothermia;
- neuropsychic stress;
- congenital failure of protective barriers;
- unfavorable climate;
- poor environmental stop;
- decreased immunity;
- lack of vitamins.
Passive smoking, as well as irritation of the ciliary epithelium by dust particles and chemicals, play an important role in the development of obstructive bronchial inflammation in children.
Pathogenesis of obstructive bronchitis in children
The pathogenesis of the disease has a complex structure. When a virus invades, inflammatory infiltration of the mucous membrane lining the bronchi occurs. Various groups of leukocytes migrate in large numbers in its tissue. Inflammatory mediators are released - histamine, prostaglandin, cytokines. Edema of the bronchial wall develops.
Then the smooth muscle fibers in the wall of the bronchi contract, causing bronchospasm to develop. Goblet cells activate the secretion of bronchial secretions. Mucus has increased viscosity. A disorder of the ciliated epithelium occurs. Mucociliary insufficiency develops. The process of coughing up mucus is disrupted.
The lumen of the respiratory tract is blocked by bronchial secretions. This creates ideal conditions for the proliferation of the bronchitis pathogen. The submucosal and muscular layer of the bronchi is exposed to inflammation. Peribronchial interstitial tissue is included in the process. Lung tissue is not involved in inflammation.
Causes of COPD
COPD can be caused by heavy smoking , occupational hazards, and exposure to unfavorable environmental conditions with increased air pollution.
The appearance of the disease can also be influenced by:
- heredity,
- pathogenic microorganisms,
- complications after infectious diseases and bronchial asthma,
- cold and wet climate,
- elderly age.
Symptoms of bronchitis
The first sign of pathology is a runny nose. After a couple of days, a cough develops. It remains dry for some period. At the same time, the temperature rises and weakness appears. Later the cough becomes wet and phlegm appears. Typically, these symptoms appear within 4-5 days. With timely treatment, you can completely get rid of the pathology in 7-8 days. But it should still be remembered that the lack of treatment can lead to the formation of a chronic form of bronchitis, and it will be much more difficult to cure.
Treatment of cough in COPD
The development of COPD can be prevented by limiting the influence of negative factors, but it cannot be cured. Treatment only slows down the progression of the disease, but does not contribute to a full recovery.
First of all, smokers should completely stop using tobacco products, and passive smokers should try to distance themselves from the source of tobacco smoke. The attending physician may prescribe medications from various groups that can alleviate symptoms:
- Inhaled bronchodilators that dilate the bronchi;
- Mucolytic drugs to reduce the viscosity of sputum and expectoration;
- Antibiotics for identified infection;
- Anti-inflammatory drugs;
- Anticholinergics to suppress the reaction of the bronchi to irritating agents.
Often, an exacerbation of COPD requires emergency hospitalization.
Classification and stages of development of obstructive bronchitis in children
There are three forms of obstructive bronchitis - bronchiolitis, acute and recurrent. Bronchiolitis often affects children under 2 years of age. This is how their body responds to the introduction of rhinovirus or respiratory syncytial infection. It is preceded by a mild ARVI. As the condition worsens, respiratory and heart failure develops. With this form, characteristic moist, fine-bubble wheezing appears on inhalation and exhalation.
Acute bronchial obstruction most often occurs in children aged three to five years. It is caused by parainfluenza and influenza viruses, adenovirus. First, the temperature rises to high numbers. Other symptoms of ARVI appear. Then manifestations of respiratory failure increase. The child has difficulty breathing. The muscles of the neck and shoulders are involved in the breathing process. Whistling sounds occur when exhaling. Exhalation becomes difficult and lengthens.
Recurrent obstructive bronchitis occurs at any age. It is caused by: mycoplasma, cytomegalovirus, herpes virus, Epstein-Barr virus. Bronchial obstruction increases gradually. This occurs at normal or low-grade fever. Nasal congestion, runny nose and infrequent coughing are noted. Shortness of breath is moderate. The general condition is almost unaffected. According to the course of the disease, the following forms are distinguished: acute, protracted, recurrent and continuously relapsing.
How does an obstruction form?
The wall of the bronchi consists of cartilaginous tissue, which changes its structure and becomes thinner as it moves away from the trachea. The volume of smooth muscle cells increases as their caliber decreases, and their sensitivity to carbon dioxide (the more of it, the wider the diameter) increases.
The decrease in bronchial lumen is caused by three mechanisms:
- swelling of their mucous membrane, resulting from the ingress of allergens or microbial antigens;
- accumulation of viscous thick sputum in the lumen;
- contraction of small-caliber smooth muscles of the bronchi.
These are three links of one process that potentiate each other.
Treatment of obstructive bronchitis in children
Children with bronchitis are often treated on an outpatient basis. Indications for hospitalization include age up to one year, the child’s serious condition, and the presence of concomitant pathologies. The main treatment is etiotropic therapy. It includes antiviral or antibacterial drugs.
Pathogenetic therapy includes selective bronchodilators or inhaled glucocorticosteroids. They are inhaled through a compressor nebulizer. The following drugs are prescribed as symptomatic therapy:
- diluting sputum - they facilitate its evacuation;
- expectorants - activate the movements of the cilia and promote coughing;
- antipyretics;
- non-steroidal anti-inflammatory drugs;
- restoratives (vitamins, immunomodulators).
During the recovery period, physiotherapy, massage and breathing exercises are prescribed.
Symptoms of obstructive bronchitis in children
At the onset of the disease, the clinical picture is dominated by manifestations of ARVI. Dyspeptic symptoms are possible in small children. Bronchial obstruction often occurs on the first day of illness. Bronchitis is manifested by the following symptoms:
- increase in respiratory rate (up to 60 per minute);
- prolongation of exhalation;
- dyspnea;
- breathing is noisy, wheezing;
- auxiliary muscles are involved in the act of breathing;
- the anteroposterior size of the chest increases;
- flaring wings of the nose;
- cough with scant sputum, paroxysmal in nature;
- sputum discharge is difficult;
- pale skin;
- cyanosis of the lips;
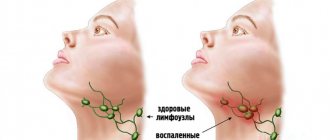
- cervical lymphadenitis.
Bronchial obstruction persists for up to a week. Then its manifestations gradually subside as inflammation in the bronchi subsides. Children under six months of age develop acute bronchiolitis. Inflammation in the bronchi is accompanied by severe respiratory failure.