Causes of the condition
Problems with the sense of smell are usually associated with pathologies of the nose. Due to swelling of the mucous membrane, congestion occurs, less air passes in and comes into contact with the taste buds. As a result, a person does not smell.
In some diseases, the bulbs themselves that capture odors are affected. They do not send signals to the brain, and the person does not feel anything.
More serious pathologies directly affect the nerve fibers that transmit the signal. The receptors pick up the smell, but the information does not enter the brain. For a person, the result is the same - lack of feelings.
The most terrible diseases are associated with the parahippocampal zone of the brain. They damage the area responsible for analyzing information about odors. The brain is not able to recognize them, so a person does not feel them.
Each mechanism is responsible for its own group of diseases. It is important to correctly identify the pathology in order to prescribe adequate treatment and the smell will return.
What diseases does it occur in?
Often, loss of smell accompanies the course of acute respiratory viral infections and acute respiratory infections. At the same time, the nasal mucosa swells, making it difficult for patients to breathe. If you remove the congestion, sensitivity will be restored. The same mechanism of loss of smell is characteristic of allergic rhinitis and sinusitis.
Much more people are concerned about why the nose breathes and odors are not felt. This happens when nerve fibers or receptors are damaged. The symptom occurs with chronic atrophic rhinitis, uncontrolled use of vasoconstrictor drops for the common cold, taking ACE inhibitors or estrogens, as well as heavy metal poisoning. This is also observed with influenza and coronavirus infection.
Damage to the areas of the brain responsible for smell is quite rare. This happens with degenerative pathologies of the nervous system (Alzheimer’s disease, multiple sclerosis), head injuries, and also against the background of complications after brain surgery.
Prospects for restoring the sense of smell in case of its permanent loss
Scientific research data have shown that regeneration of the olfactory epithelium after viral infections occurs through neural stem cells, from which both the olfactory epithelium and the cells supporting olfactory neurons are regenerated. With a chronic inflammatory process in the nasal cavity, this regenerative process is disrupted. Perhaps in the future, drugs will be developed to stimulate the regenerative process or protocols will be created for transplanting stem cells responsible for the regeneration of olfactory neurons into a special area in the nasal cavity. One way or another, we can only believe that these studies will be initiated by analogy with stem cell transplantation for other pathologies in the human body.
Diagnostic measures
When contacting a doctor, attention is paid to complaints and epidemiological history. If the patient has been in contact with a sick person, and also has nasal congestion and a high temperature, ARVI and acute respiratory infections can be assumed. A person is recommended to undergo a general blood test to accurately determine the nature of the disease: bacterial or viral.
A sudden loss of smell and taste is a sign of coronavirus infection. The patient is advised to undergo tests for the pathogen in the form of a nasal swab.
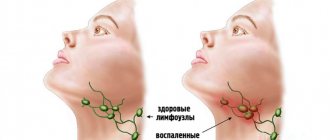
Allergic rhinitis is diagnosed by a characteristic clinical picture. A smear from the nasopharynx reveals neutrophils and elevated IgE in the blood.
Atrophic rhinitis is diagnosed by an otolaryngologist after an in-person examination. Sometimes an x-ray is recommended. The same diagnostic method is used for sinusitis.
Treatment Options
What to do if your sense of smell is lost depends on the cause of the condition. Therapy is selected by the doctor individually, taking into account age and concomitant diseases.
Treatment regimens:
- Antibiotics - for moderate to severe acute respiratory infections, sinusitis.
- Bed rest and drinking plenty of fluids is for uncomplicated ARVI.
- Tamiflu, Oseltamivir - for influenza.
- Corticosteroids locally in the form of a spray - in case of abuse of vasoconstrictor drops.
- Antihistamines - for allergic rhinitis.
For atrophic rhinitis, coronavirus infection and all types of brain damage, a treatment regimen is developed by a specialist taking into account clinical recommendations and the patient’s condition.
The sense of smell returns after recovery and recovery period. It lasts from 2 weeks to 3 months. If there is no improvement, it is worth undergoing a re-examination to assess the condition of the receptors and nerve endings.
Read also: Dry paroxysmal cough
Dear patients! Remember that only a qualified doctor can make an accurate diagnosis, determine the causes and nature of the disease, and prescribe effective treatment. You can make an appointment with our specialists or call a doctor at home by calling 8-(4822)-33-00-33
Be healthy and happy!
“Even people smell bad.” How to live with parosmia after Covid
Tatyana lives in the Moscow region. When she was expecting her third child, five months pregnant, she fell ill with coronavirus. She lost her sense of smell. “At first this made me happy, because I was too sensitive to smells, for example, I couldn’t travel on public transport,” recalls Tatyana. “But, of course, it was hard in everyday life: I almost fed the children rotten soup.” A month after giving birth, the situation changed, the smells began to return to me. But they were not the same as before: everything smelled of something chemical, rotten meat and some odors that did not even exist in nature. I remember the moment where it all started. At night I smelled a strong smell of rubber. At first I thought that he appeared because of a children's cheesecake, which they use to ride down the slide; it was standing in our hallway. We took the cheesecake out onto the balcony, but the smell did not disappear. And no one felt it except me. Then an unpleasant, sickly-sweet smell began to emanate from my hair. I put them in a bun, but it didn't help. Then I began to smell the same smell from the products. As a result, I stopped cooking and eating normally for a while. She saved herself by delivering ready-made food for her family, and for a month and a half she ate oatmeal and honey cake, took vitamins to smooth out the imbalance of nutrients, but her skin still broke out in acne. In the end, I began to smell an unpleasant odor even from people, and tried not to let anyone into my room. When I got hysterical because of this, I started googling what it even was. My husband believed that parosmia exists only when I sent him an article about it.”
Tatyana went to the doctor, but he did not solve the problem. However, she is now making progress for the better. “The doctors didn’t really help me: someone didn’t understand my problem, one doctor recommended a drug to improve cerebral circulation, but it didn’t help me. Now I’m seeing slight progress for the better - I’ve started eating potatoes,” shares Tatyana.
Collage: Anna Sbitneva
“Among the smell disorders with Covid-19 in clinical practice, we most often encounter anosmia (complete absence of smell) and hyposmia (its significant decrease), explains Alexey Yakovlev, Candidate of Medical Sciences, Director of the Association for the Development of Rehabilitation, Physiotherapy and Habilitation. — Parosmia — distortion of odors — is somewhat less common with Covid-19. Like other smell disorders, parosmia develops due to the ability of a virus to penetrate nerve cells and cause so-called “neuroinflammation” - this is called neurotropism of the virus. As a rule, smell disturbances with Covid-19 are short-lived and do not require the use of any specific additional therapy. On average, smell disturbances develop on days 3–5 of the disease and persist during the first 8–14 days of the disease. Most patients note complete restoration of olfactory function by the time the virus is eliminated from the body. However, if olfactory dysfunction persists after the patient receives the first negative PCR smears, this is always a reason to contact specialists - a neurologist and an otorhinolaryngologist.” Yakovlev says that disturbances in the sense of smell are not always related to how seriously ill a person was. However, “it is known that vaccinated patients, in case of illness, suffer from Covid-19 in a milder form, i.e., any manifestations of the disease are less pronounced, the same applies to dysfunction of the olfactory analyzer.”
Alexey Yakovlev. Collage: Anna Sbitneva
“The duration of the violation depends on the severity of the damage. Within 6 months, 95% of patients regain their sense of smell. The taste usually returns to normal much sooner. Doctors have encountered post-viral anosmia before (with rhinovirus, adenovirus infections, parainfluenza), but much less frequently, says otolaryngologist, Ph.D. Anastasia Varvyanskaya. - There is no method that would instantly cure. You should consult a doctor if your sense of smell persists for a month or if you are bothered by a runny nose, nasal congestion, or pain. The doctor conducts an endoscopic examination of the nasal cavity, assesses olfactory and gustatory function. Depending on the situation, he may prescribe additional examination and treatment.”
Anastasia Varvyanskaya. Collage: Anna Sbitneva
“To date, there are no approved treatment regimens for persistent impairment of smell in patients who are convalescents of the new coronavirus infection Covid-19; treatment is always symptomatic and strictly personalized. But smell disorders can be a consequence of other diseases and pathologies, some of which are very serious. Among the neurological diseases in which a violation of the sense of smell may be one of the first symptoms, Parkinson's disease, Alzheimer's disease, dementia with Lewy bodies, and brain tumors should be highlighted. All these pathologies require quite serious professional diagnostics,” Yakovlev points out.
“I got sick in July - I was very weak, I couldn’t get up, I was practically crawling around the apartment, and I had a severe headache,” says Anna, another person who recovered from coronavirus. — When everything passed, there were signs of disturbances in the sense of smell and taste when I ate eggs, but then the smell was even more or less normal. And just three weeks ago, active manifestations began: the smells of meat, onions and eggs changed. From these products I smell a pungent smell of rotten meat, which is generally intolerable. While I have not tried treatment, I hope that it will somehow go away on its own. At first I endured it, ate these foods through force, I just couldn’t believe that I would never be able to feel their previous taste and that it would now be so unpleasant. Then I realized that this couldn’t continue like this and I just had to eliminate these foods from my diet. Although these foods are my favorites, I used to simply not do without them, I ate them every day. Now you have to change your menu. I haven’t felt any better yet, but that’s because the problem with me is recent. I wasn’t particularly afraid of the manifestations of parosmia - it’s unpleasant, of course, that there is such a side effect. I had already heard about this problem, but I didn’t think that I would have it. I tried to “mask” the smell with spices, but I can still smell it all. The smell of the oatmeal has also changed, but for the better - for some reason it has a sweet smell, like it smells like caramel. I used to not like the smell of oatmeal, but now I like it.”
Anna. Collage: Anna Sbitneva
“Food does not become harmful because the brain does not perceive the smell correctly. The main thing is that it is not rotten,” explains the gastroenterologist, Ph.D. Roman Karas. — There is also usually no gastroenterological reason for such symptoms. Because smells are the brain and the nose. But with prolonged parosmia, you limit yourself in the intake of important nutrients, which, of course, will affect your health. Try eating food that smells like rotten fish or feces. Will it work? No. All that remains is to choose products that smell tolerable and avoid parosmia provocateurs. Pleasant taste and smell improve mood, improve appetite and bring joy. With parosmia, the opposite is true: sadness, melancholy, sadness and even weight loss. If you perceive odors incorrectly, you can miss a fire, harmful fumes/gases, a spoiled product, and even lose your job if you are a cook, perfumer, or firefighter. Hygiene difficulties arise."
Roman Karas. Collage: Anna Sbitneva
“Self-medication, which is based on recommendations from the Internet, is a very risky way to restore the sense of smell,” Yakovlev points out. “There are opinions from practicing specialists that neuroprotective therapy and vitamin therapy can speed up the process of restoring the sense of smell, but treatment should always be individual and a treatment plan should be drawn up only with face-to-face interaction between the patient and the doctor.”
Success in treating parosmia also depends on the psychological state of the person. Anxiety, sleep disorders, depression and hypochondriacal disorders can aggravate the symptoms. “The work of the olfactory analyzer is closely related to the work of the centers of the autonomic nervous system, so any psycho-emotional dysfunction that the patient has can contribute to a more pronounced disruption of the olfactory tract, including as part of the development of a syndrome complex of post-Covid disorders (the so-called Long Covid),” says Yakovlev .
“An important role for patients with olfactory impairment is the understanding and support of loved ones, the opportunity to discuss their problem with someone who is in a similar situation, and access to competent sources of information on this problem,” says Varvyanskaya. She also points out that each case of parosmia is individual, and to make a diagnosis you need to consult a doctor: “You need to start with an ENT specialist. The sense of smell can be impaired for various reasons: nasal/sinus disease, acute respiratory viral infections, trauma, neurodegenerative disorders.”
Collage: Anna Sbitneva
Denis, who had coronavirus, had to fight parosmia for about seven months. He was ill in December, and the disturbance in his sense of smell appeared in March. “I noticed the problem by chance when I was eating meat,” says Denis. “I thought it was just spoiled.” But the completely different meat smelled exactly the same the next day. And I realized that there was some problem with me, and not with food. My first thought was that there was something wrong with my nerves or something wrong with my head. I started searching on the Internet to see what it could be, and came across a group on the social network VKontakte where they discussed that distortions in smells appear after the coronavirus. And so everything fell into place in my head, I realized that all this was because of “corona.” There was no misunderstanding on the part of loved ones. At first they looked at me as if I was a little crazy, but when I explained the situation, everyone took it as normal. No one ever said that I imagined or invented something for myself. The biggest problem for me was the unpredictability of grocery shopping: I didn't know what I could eat and what I couldn't. At first it seemed that everything was simple: I can’t eat dairy, meat, onions, so these foods need to be excluded, everything else should be eaten. But sometimes some foods began to smell unpleasant, from which I did not expect this at all, for example, some vegetable. And it turns out that you simply throw away half of the food at home because you can’t eat it. All purchases were a lottery.” Denis did not go to the clinic because he was not sure that his attending physician could help in this matter.
“This problem itself lasted about seven months, the worst were the first two, when everything really stinks, from milk to soy meat, everything that contains protein, lactose,” recalls Denis. “Then the range of products expanded. Somewhere in the middle of summer I started drinking milk, it no longer had a strong smell. And gradually, over two months, the [unpleasant] smell disappeared completely. It’s the same story with meat: at first I only ate fish and sausage, and then I started eating pork, although chicken and beef still smelled bad. I started eating chicken normally in September. The recovery was not abrupt - it took me about four months. If there was no information about parosmia (and when I started, there was little information), then it would be absolutely terrible to walk around and think that there is something wrong with your head. And just not knowing what to do, whether the distortion of smells will ever go away, it would be very psychologically difficult. And when I found information, read the stories of people who had experienced this, it was somehow easier to accept.”
Illustrations: Anna Sbitneva