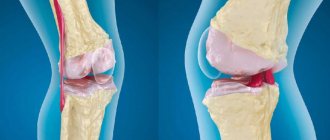
Synovitis of the knee joint is an inflammatory process limited to the joint membrane of the lower limb. A characteristic feature of the development of the pathological process is the accumulation of fluid in the joint, which significantly reduces the functionality of the knee.
Among the key reasons are previous injuries, as well as other joint pathologies and various metabolic disorders, including infectious lesions.
The main clinical manifestations are pain, the intensity of which increases when attempting to perform a movement, as well as swelling and an outwardly noticeable increase in the size of the localization site.
The diagnosis is made based on the patient’s existing complaints, visual examination, as well as the results of the study (laboratory/instrumental).
The treatment plan for each patient is determined individually, in accordance with the existing symptoms and his state of health.
Causes of synovitis of the knee joint
So, in most cases the cause of inflammation is:
- fur damage character that emerged as a result of traumatic experience. Pathologies cause destruction of the connective tissue of the joints;
- changes inside the joint cavity caused by loss of mobility and elasticity of tissues. In such situations, a slow infection develops and pus appears.
The traumatic type of synovitis is considered the most common. It has been studied almost completely and has a wide range of treatment variations.
Symptoms of the disease
Symptoms of synovitis are important for an accurate diagnosis. Among the signs of synovitis that indicate inflammation, there are several dominant ones that are inherent in all varieties of this disease:
- dull pain;
- the formation of exudate in a huge amount, which leads to an increase in the size of the joint;
- disruption of the normal functioning of the joint.
Knowing the symptoms will help you determine the nature of the injury in a short time. If the above signs of inflammation are detected, you should seek help from a specialist as soon as possible.
Diagnosis of synovitis
Diagnosis of pathology should be based on the patient’s complaints, as well as on the research performed. To make a correct diagnosis, instrumental research methods are usually used. To confirm synovitis, the following diagnostic methods are prescribed:
- radiography of the joint;
- Ultrasound of the joint;
- joint puncture;
- arthroscopy;
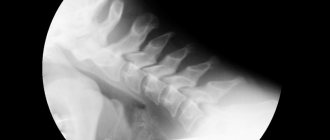
- CT;
- MRI.
Let's consider the main types of research.
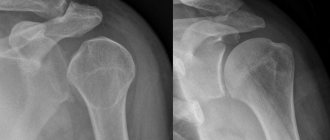
X-ray of the joint
Radiography is considered one of the simplest, inexpensive and fastest methods. An X-ray will help the doctor identify the inflammatory process in the synovium of the joint, based on a visual determination of the amount of fluid in the joint. X-rays also help determine the size of the joint space and the condition of the joint surfaces. Basically, doctors prescribe studies of both joints (healthy and diseased) in order to compare and identify the degree of inflammation.
Ultrasound examination of the joint
A joint ultrasound is a non-invasive test (does not damage tissue) that helps identify the cause and extent of joint damage. This diagnostic method also helps to find out the thickness of the synovial membrane, the volume of specific fluid that filled the joint, as well as determine the condition of the articular surfaces and tissues. It should be emphasized that ultrasound and x-rays, unlike puncture, can be used to diagnose synovitis in children.
Joint puncture
Joint puncture is considered the most effective diagnostic option, as it helps determine the type of fluid obtained through bacterial examination (microorganisms can be detected in the synovial fluid). Also, with the help of this study, you can detect bloody discharge, fibrin, pus and much more. In order to perform a puncture, the skin in the puncture area is thoroughly treated with a 5% iodine solution, and then wiped with 70% alcohol. This is due to the fact that iodine during puncture can enter the synovial membrane and cause chemical reactions. burn. It should be noted that the research method and the patient’s position during puncture of different joints are different. So, for example, puncture of the knee joint can be performed at one of four points.
How to treat rheumatoid and psoriatic synovitis
This synovitis develops against the background of rheumatoid arthritis. Therefore, in order to eliminate its symptoms, it is necessary to treat the underlying disease. Therapy should be carried out comprehensively and include the following elements:
- Chondroprotective agents are used to preserve the tissues of the knee joint. An effective and inexpensive drug in this group is Chondroitin.
- Anti-inflammatory treatment - if there is a good effect from NSAIDs, you can limit yourself to regular use of these drugs in combination with Omeprazole. If it is ineffective, the doctor prescribes hormones (Prednisolone, Hydrocortisone, etc.), calculating the dose individually.
- Reducing the load on the affected joint also reduces pain. The knee joint can be unloaded by recommending that the patient use a cane when walking.
- Physiotherapy is pain-relieving procedures aimed at the affected area. The use of any techniques is allowed: UHF therapy, photo and magnetic therapy, galvanization.
Treatment should be carried out by a rheumatologist. It is not recommended to independently treat this form of synovitis.
Types of synovitis
There are acute and chronic forms of the inflammatory process. Usually, after the first manifestation of synovitis, the patient experiences relapses in the future - the disease becomes chronic. Synovitis can affect any joint, so the following classification exists:
- Moderate inflammation of the elbow joint. The disease can manifest itself in severe form, but this happens infrequently. The disease is classified as an occupational disease of mechanics and people involved in sports. Patients experience serious discomfort up to intense pain, not only during the process of moving, but also in conditions of complete rest.
- Synovitis of the shoulder joint. Occurs due to carrying heavy objects and injury to the shoulder or forearm. Among the signs, only pain can be identified, since the swelling itself appears only during the acute course of the disease.
- Synovitis of the knee joint. One of the symptoms of the disease is joint instability. You can check everything in a couple of minutes - you need to straighten your knee in a sitting position and press on the kneecap, which should return to its place after displacement. Treatment of the acute phase is performed only in inpatient settings. Only in a hospital can you quickly restore the condition of the joint and avoid the acute phase.
- Inflammation of the hip joint is considered a rare pathology among adults. Typically, this form of the disease occurs in children between 4 and 8 years of age. It is worth highlighting that in childhood, synovitis can occur without an obvious reason. Sometimes, in addition to injury, the cause of the inflammatory process is a viral infection. Synovitis of the hip joint leads to pain when moving. The diseased joint swells, and there is also some stiffness in movement. Synovitis appears spontaneously, patients complain of pain in the legs. Further pain is localized near the hip joint. In childhood, this disease can lead to temporary lameness.
- Synovitis of the ankle joint is in many ways similar to other types of disease. The ankle swells, the skin over its surface becomes hot to the touch and becomes covered with red spots. Pain can occur not only when moving, but also at rest. This is due to the fact that the synovial membrane is considered sensitive. Also, with minimal load on the ankle, rapid fatigue occurs. Usually the cause of inflammation of the ankle joint is injury. A subluxation or direct blow to the ankle usually leads to microtrauma of the synovium and the development of synovitis.
- Synovitis of the foot joints. Basically, the inflammatory process of the synovial membrane begins in the metatarsophalangeal joint of the big toe (it is this joint that is most susceptible to deformation). Sometimes the inflammation also spreads to the long extensor tendon of the toes (tendinitis). Often this localization of synovitis indicates serious stress on the feet. Dancers, gymnasts and ballerinas are at risk. This type of synovitis is characterized by an increase in the size of the joint, redness of the skin around it, and pain when moving. If symptoms of the disease reappear, in some cases degenerative changes in the diseased joint (arthrosis) are possible. Most often, within three weeks the inflammation goes away, and the functionality of the joint is completely restored.
There is also villonodular and suprapatellar synovitis, but these types are rarely observed in patients, they do not have characteristic symptoms and can only be diagnosed by specialists. Diagnosis of any type of synovitis is carried out using a comprehensive examination.
Symptoms
The signs of the disease, regardless of its origin, are the same. True, they can appear at different time intervals. Symptoms characteristic of synovitis are:
- increased fatigue under loads that a person could previously easily cope with;
- feeling of discomfort in the problem area;
- pain localized in the ankle area, which can affect surrounding tissues with severe swelling;
- redness and swelling of the area involved in the pathological process;
- an increase in temperature and the appearance of symptoms of general intoxication (with an infectious form) are possible.
The severity of symptoms depends on the stage of the disease. The first alarm bell is always pain, which initially appears only when performing rotational movements. Gradually, the pain increases so much that it accompanies the patient even at rest, disrupting sleep and normal functioning in general.
Treatment of synovitis of the knee joint
Let's consider two main types of treatment for the disease. Conservative therapy. Treatment of aseptic type synovitis in most cases is outpatient, includes puncture with fluid evacuation and immobilization of the limb with a plaster splint, knee brace or tight bandage. Immobilization can last a maximum of 7 days, since prolonged absence of walking can cause the development of joint stiffness. Patients are prescribed exercise therapy, microwave therapy, electromagnetic treatment, electrophoresis with dimethyl sulfoxide or hydrocortisone and ultrasound with anti-inflammatory drugs. After eliminating the acute phase, paraffin, ozokerite, mud treatment, and balneotherapy are recommended.
For reactive synovitis, treatment is prescribed with glucocorticoids, calf cartilage extracts, heparin, ibuprofen and indomethacin. During an exacerbation, from the third or fourth day, patients are sent to physical therapy: phonophoresis with corticosteroid medications, UHF, magnetotherapy, electrophoresis with aprotinin, ketoprofen and heparin. Please note that heparin should not be taken immediately after injury or surgery, or if you have clotting problems. If you need help, please contact us. Our clinic employs only qualified specialists; they conduct individual exercise classes, massage, etc.
For chronic synovitis with obvious infiltration of the synovial membrane, inhibitors of proteolytic enzymes are prescribed, aprotinin and corticosteroids are injected into the joint.
Surgery
Pathogenetic therapy of traumatic synovitis involves restoration of anatomical features in the joint. The treatment regimen in each individual case is determined individually, taking into account the scale of changes, the severity of general disorders, the prospects and risks of the need for surgery and other points. In the postoperative period, drug correction of local metabolic disorders is prescribed and rehabilitation is carried out.
If irreversible changes in the synovial membrane develop during the chronic course of the disease, surgery is performed - partial, subtotal or total synovectomy. In the postoperative period, immobilization is performed, antibiotics, painkillers, exercise therapy and physiotherapy are prescribed.
Signs
The disease can occur in acute or chronic form. In the acute form, pain, swelling, and redness of the skin occur in the joint area. Movements are limited due to pain. In the chronic form, the same symptoms are present, but they are less pronounced. They then subside, then a new exacerbation develops. Inflammation of the articular membrane when an infection is attached can turn into a purulent form. The joint swells even more, severe pain occurs, and pus accumulates under the skin. The general condition of the patient is disturbed, body temperature rises.
At CELT you can get a consultation with a traumatologist-orthopedic specialist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Prevention of synovitis
To prevent a relapse, you must not forget about preventive measures. Prevention is a set of rules and measures that will help maintain the health of your lower extremities.
When playing sports, do not forget to be careful, this will help protect your knee from injury. Also, special attention should be paid to the choice of shoes, not only those in which you train, but also everyday ones. Having the right shoe collection will protect you from future injuries. Professional athletes should fix the articular surfaces with special pads or bandages. Contact us if you have severe or moderate synovitis, we will help. We employ qualified specialists. Prices can be found in the price list on the website or by calling +7,).
Exercise therapy
After arthroscopy, joint surgery or conservative treatment, it is recommended to perform a set of exercises to quickly restore the functions of the limb (start exercises within the time frame indicated by the doctor):
- Lie on your back, then perform partial flexion and extension of the knee (10 times).
- While lying down, squeeze any flat object up to 10 cm thick under the knee (10 times).
- In any position, strain the muscles of the thigh and lower leg (5-6 times).
- Lie on your back, slowly lift your straight leg 40 cm from the floor and lower it (10 times).
- Lie on the side opposite the side of the affected leg, then move the affected leg up (5 times).
- Sit on a chair and slightly lift the sore leg above the floor surface with a 1-kilogram load attached (5 times).
- Standing on the affected leg, half-squat and perform rotational movements with the other leg (1 minute).
After stabilizing the condition, it is recommended to walk for a distance of up to 500-600 m several times a week at a slow speed, as well as exercise on an exercise bike.