Arthrosis of the knee joint is a degenerative-dystrophic pathology that leads to deformation and destruction of articular cartilage. Gradually the limb loses mobility. According to statistics, almost every third person on the planet suffers from arthrosis, and this number is not decreasing. Elderly people, especially those who are overweight, are at risk. After 65 years, arthrosis is diagnosed in 70-85% of cases of treatment for knee pain.
A rheumatologist helps maintain a patient’s quality of life with joint pathology.
general information
The knee joint regularly experiences enormous stress. Walking, running, jumping, climbing stairs and simply standing - all this has an impact on the condition of cartilage. The processes of destruction and restoration are in constant balance, but if, under the influence of certain reasons, this balance is disturbed, the gradual development of arthrosis begins.
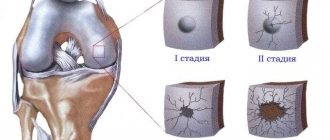
Initially, microcracks appear in the thickness of the cartilage, which help reduce its thickness in some areas. As a result, the load is redistributed on the contacting surfaces of the bones, which accelerates the pathological process. Gradually, a whole complex of changes occurs in the knee:
- thinning of cartilage until complete disappearance;
- changes in the composition and reduction in the amount of synovial fluid;
- damage to bones due to friction against each other;
- the appearance of bone protrusions (osteophytes) first along the edges of the joint, and then throughout its entire area;
- compaction of the joint capsule as a result of a chronic inflammatory process, which leads to joint stiffness;
- compensatory spasm of surrounding muscles.
Ultimately, the knee becomes significantly deformed and mobility is limited, leading to disability.
Depending on the location of the process, arthrosis of the knee joint can be unilateral and affect the right or left knee, or bilateral. In this case, both legs are affected.
Make an appointment
Frequently asked questions about the disease
Arthritis and arthrosis – what is the difference?
The difference is that arthritis is an inflammatory process in the joint, and arthrosis is degenerative-dystrophic (metabolic) with gradual “drying out” and cracking of cartilage, compensatory growth of bone tissue. Chronic arthritis gradually turns into arthrosis-arthritis and arthrosis.
Is it possible to warm joints in a sauna/bath if you have arthrosis?
It is possible and it will be beneficial. But arthrosis is often complicated by inflammation (arthritis), in which warming water procedures are contraindicated. Therefore, before you start treating arthrosis with water procedures, it is better to visit a doctor.
Do they take you into the army with arthrosis?
It depends on how pronounced it is. If the function of the joint is impaired, then no.
Is it possible to develop arthrosis after coronavirus infection? If not, why not?
It is unlikely that anyone will answer this question now, there is simply no data. The development of arthrosis is a slow process.
Which doctor should I contact for arthrosis?
To a therapist. He will conduct an examination, a preliminary examination and, depending on the type of arthrosis, will refer the patient to an orthopedic traumatologist or rheumatologist.
Does arthrosis occur in children?
It happens after injuries and joint diseases.
Arthrosis is not a death sentence. It cannot be completely cured, but it can and should be treated - this will save patients from suffering. Moscow medical specialists successfully cope with the treatment of arthrosis.
Literature:
- Karateev A.E., Barskova V.G. Criteria for choosing a non-steroidal anti-inflammatory drug. Handbook of a practical doctor, 2007.- T. 5.- No. 5.- P. 13-17.
- Povoroznyuk V.V. Osteoarthritis: modern principles of treatment // News of medicine and pharmacy. - 2004. - T. 144, No. 4. - P. 10-11.
- Raisz LG Prostaglandins and ione: physiology and pathophysiology. Osteoarthritis Cartilage, 1999.- V. 79.- P. 83-94.
- Peyron JC, Altman RD Osteoarthritis: diagnosis and medical surgical management. — 2nd ed. - Philadelfia, Pa: WBSauders Company, 1992. - P. 15-37.
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 04/22/2021 Date of update: 04/11/2021
Reader rating
Rating: 4.29 / 5 (7)
Causes
Arthrosis occurs against the background of its damage due to increased load, inflammation, or against the background of congenital pathologies of the articular apparatus. The list of the most common reasons includes:
- knee injuries: dislocations, damage to ligaments and menisci, severe bruises accompanied by hemorrhage into the joint cavity, intra-articular bone fractures;
- increased load on the joint: professional sports, lifting weights, working in a standing position, wearing the wrong shoes, excess body weight;
- connective tissue pathologies: systemic lupus erythematosus, rheumatoid arthritis;
- congenital and acquired weakness of ligaments and muscles, including those associated with low physical activity;
- diseases or injuries of the musculoskeletal system, accompanied by increased load on the knee (flat feet, arthrosis of the hip joint, etc.);
- hormonal disorders, especially diabetes;
- metabolic disorders accompanied by salt deposition (gout);
- inflammation of the joint (arthritis) regardless of the cause;
- knee surgery;
- heredity.
What is arthrosis
Arthrosis is a disease of the joints of a degenerative-dystrophic nature with the gradual destruction of cartilage and proliferation of bone tissue. The process is accompanied by deformation, impaired joint function and pain. Recently, the term osteoarthritis (OA osteoarthritis) is more often used - a group of diseases that are based not on purely dystrophic, but on dystrophic-inflammatory processes leading to gradual destruction of the joint. More and more experts believe that the causes of arthrosis and osteoarthrosis, the mechanisms of their development are the same, that is, in fact, they are the same disease.
According to statistics, from 10 to 20% of the population suffers from arthrosis in different countries. By the age of 80, almost everyone has age-related disorders in the musculoskeletal system. At the same time, patients do not always consult a doctor on time and take a long time to treat themselves, which leads to disability. Whereas the right treatment can relieve suffering and stop the progression of the disease. Arthrosis codes according to ICD 10: M15-M19.
Degrees
Depending on the extent of tissue damage, orthopedists distinguish 4 degrees (stages) of arthrosis of the knee joint, which determine its symptoms:
- grade 1: there are no symptoms, and minor abnormalities are found on x-rays;
- degree 2: the patient notes episodic pain during physical activity, when walking up stairs, squats, and standing for a long time; The images reveal a narrowing of the joint space and obvious foci of degeneration; initial manifestations of osteophytes or calcification of the lateral ligaments of the joint.
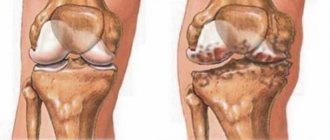
- degree 3: pain haunts the patient constantly, even at rest, walking without a cane is impossible; X-rays show a significant narrowing of the joint space, sometimes asymmetrical, due to damage to the menisci, signs of joint deformation, multiple, large osteophytes, bone growths;
- grade 4: movements in the joint are practically impossible, X-rays reveal complete destruction of cartilage and significant deformation of the articular surfaces of the bones, a large number of osteophytes; in severe cases, the bones fuse together.
Medicines for deforming arthrosis
Drug therapy for deforming arthrosis is effective at stages 1 and 2 of the disease, when destructive processes in cartilage and bone can be stopped while maintaining mobility in the joint.
Pharmacotherapy begins with the prescription of anti-inflammatory drugs, the secondary effect of which is to reduce pain. It is also important to relieve muscle spasms and improve blood circulation in the affected part of the body. Chondroprotectors are used to regenerate cartilage and prolong remission.
Anti-inflammatory
Anti-inflammatory drugs are steroidal and non-steroidal. Treatment of deforming arthrosis begins with non-steroidal drugs, which are prescribed in the form of tablets or administered intravenously or intramuscularly (to protect the gastric mucosa). To relieve symptoms and as an adjuvant, NSAIDs can be used externally - in the form of tablets, gels, creams, compresses.
In minimal “working” dosages for the treatment of deforming arthrosis the following is prescribed:
- artradol;
- ketoprofen,
- diclofenac (diclac);
- ibuprofen;
- meloxicam (movalis) or piroxicam;
- indomethacin
When taking NSAIDs in tablet form, it is recommended to take omeprazole in parallel to offset side effects. Self-medication with non-steroidal drugs is extremely undesirable: only a doctor can select the most gentle and at the same time effective drug in the right dosage, taking into account the stage, cause of deforming arthrosis and the patient’s health condition.
If NSAIDs are ineffective, to relieve exacerbations of arthrosis, the doctor may prescribe hormonal drugs - corticosteroids:
- diprospan;
- hydrocortisone;
- Kenalog (triamcinolone).
As a rule, these drugs are used in the form of intra-articular injections in short courses.
Chondroprotectors
To improve movement in the joint, chondroprotectors are prescribed - drugs that stimulate the production of joint fluid and trigger the processes of regeneration of articular cartilage. They must be taken in long courses over 3-6 months.
Chondroprotectors include preparations based on chondroitin sulfate, glucosamine sulfate, collagen and hyaluronic acid, which can be supplemented with vitamin C and other antioxidant components. For example:
- artracs;
- teraflex;
- ostenal;
- hyastat;
- alflutop.
Antispasmodics
Spasms cause the destruction of muscle tissue and accelerate its degeneration, reduce the range of voluntary movements in the joint, and negatively affect the psycho-emotional state of the patient. To prevent this in the treatment of deforming arthrosis, the following are used:
- mydocalm;
- spasmalgon;
- tolperisone;
- sirdalud;
- catadolon.
Angioprotectors
To improve metabolism and blood microcirculation in the periarticular tissues, angioprotectors and venotonics are used:
- Actovegin;
- repared;
- horse chestnut extract;
- a nicotinic acid;
- pentoxifylline;
- troxevasin.
Symptoms
Symptoms of knee arthrosis are typical of a degenerative lesion. A person faces the following problems:
- pain at the initial stage manifests itself in the form of mild discomfort after climbing stairs, and then gradually increases; with severe damage, it becomes permanent and torments the patient even at rest;
- morning stiffness: occurs already in the early stages of development, at first lasts only a few minutes, then up to half an hour;
- crunching: occurs with the second and further degrees of damage, differs from physiological sound in sharpness and special tonality, and is also accompanied by pain;
- limited mobility: associated with the proliferation of osteophytes and increased bone friction; bending and straightening the knee is difficult and often accompanied by pain; in the final stages, the joint may become completely blocked (ankylosis);
- knee deformation: occurs due to changes in the shape of the contacting bones, bone growths and involvement of muscles and ligaments in the pathological process; when inflammation occurs, swelling of the tissues around the joint occurs;
- lameness: as arthrosis progresses, a person lame more and more; in the later stages, he is forced to use a cane or walker.
Signs of disease progression
With the development of symptoms of gonarthrosis, the clinical picture becomes brighter: the knees begin to bother at rest and even at night, during movements associated with flexion or extension. Lameness appears, stiffness of movement increases, swelling of the soft tissues, inflammation of the synovial membrane occurs, effusion can accumulate in the joint cavity, externally the knee increases in volume, the contours are smoothed out.
The progression of DOA and a further increase in the degree of destruction are evidenced by the following changes:
- Curvature of the limb axis in the form of O-shaped legs (usually indicates the transition of defarthrosis to stage 3);
- Constant nature of pain, night pain and the manifestation of pain when the weather changes (meteosensitivity);
- Deterioration of motor functions, with the development of flexion contracture;
- Weakness and atrophy of the thigh muscles progresses.
Read more about what to do in case of exacerbation of arthrosis here>
Diagnostics
Diagnosis of arthrosis of the knee joint is carried out by an orthopedist-traumatologist. The following help to distinguish the disease from pathologies with a similar picture, as well as determine the degree of damage:
- interview and history taking: the doctor finds out the main complaints, the history of the development of the disease, learns about previous injuries, etc.;
- examination: the degree of knee mobility, tissue deformation, and pain syndrome characteristics are revealed;
- laboratory diagnostics: a general blood test reveals inflammation, a biochemical test reveals possible causes of problems;
- X-ray methods: X-ray and CT are the main diagnostic methods, allowing to detect typical signs of arthrosis: narrowing of the joint space, osteophytes, bone deformations;
- MRI: makes it possible to visualize soft tissues, assess the condition of muscles and ligaments;
- Ultrasound: assessment of the condition of muscles, tendons, joint capsule;
- joint puncture: allows you to take an analysis of the joint fluid, as well as insert a miniature camera to examine the cavity from the inside (arthroscopy).
If necessary, additional studies and consultations with specialists are prescribed.
Treatment of arthrosis of the knee joint
All treatment methods for arthrosis of the knee joint can be divided into three groups:
- medicinal;
- physiotherapy;
- surgical.
When a patient is diagnosed with stage 1-2 disease, a complex of medications and physical therapy is used, but if the lesion has become extensive, surgery remains the priority.
Drug treatment
Proper administration of medications can relieve pain, stop the inflammatory process if it exists, and also stop or at least slow down the destruction of cartilage tissue. The following groups of tools are used for this:
- anti-inflammatory (ibuprofen, ketoprofen, diclofenac, as well as their derivatives): relieve inflammation and relieve pain in the joint;
- hormonal (corticosteroids): prescribed when anti-inflammatory drugs are ineffective;
- antispasmodics (mydocalm and analogues): help get rid of muscle spasms and alleviate the patient’s condition;
- chondroprotectors (glucosamine, chondroitin and their combinations) stimulate the processes of regeneration of cartilage tissue;
- drugs to improve microcirculation (nicotinic acid, cinnarizine, pentoxifylline): improve the supply of oxygen and nutrients to the joint.
Depending on the situation, tablet, injection and local forms of drugs are used, intra-articular administration is allowed. Only a doctor is responsible for selecting medications, their dosage and frequency of administration. If used uncontrolled, many drugs can worsen the condition of the joint and also cause unpleasant side effects.
Physiotherapy
Physiotherapeutic techniques are used to improve blood circulation in the joint area, increase mobility, and also enhance the effect of medications. The doctor may prescribe:
- shock wave therapy: ultrasound of a special frequency, helps eliminate osteophytes;
- magnetotherapy: exposure to a magnetic field, stimulating metabolism and regeneration processes;
- laser therapy: deep heating of tissues with a laser beam;
- electrotherapy (myostimulation): exposure of muscles to a weak electric current;
- electro- or phonophoresis: administration of medications (chondroprotectors or analgesics) using electric current or ultrasound;
- ozone therapy: introduction of a mixture of gases into the joint cavity.
Physiotherapy exercises and massage are also prescribed according to individual indications.
Stages of the disease
Arthrosis of the joints develops gradually and in the process goes through three successive stages that determine the severity of the disease:
- Stage 1: the pathology is not detected on X-ray or ultrasound, but the destruction processes have already started; the composition of the joint fluid changes, as a result of which the tissues receive fewer nutrients and become more sensitive; increased stress on the affected area causes inflammation (arthritis) and pain;
- Stage 2 is characterized by active destruction of cartilage tissue, and bone spines and growths appear along the edges of the articular platform (the area of contact of surfaces); at this time, the pain becomes habitual, and the inflammatory processes become stronger and weaker; spasms of the muscles associated with the joint are periodically observed;
- Stage 3: areas of destruction affect almost the entire surface of the cartilage, the articular area is deformed, the affected limb deviates from its axis; range of motion decreases and ligaments weaken and become short.
Some experts also distinguish stage IV of the development of arthrosis. It is characterized by almost complete immobility of the joint.
Surgery
Surgical treatment of knee arthrosis is prescribed when other methods are ineffective. Doctors perform several types of operations:
- endoprosthetics: complete replacement of a damaged joint with a prosthesis;
- arthrodesis: fastening bones together to eliminate mobility (reduces pain and allows a person to lean on the leg);
- osteotomy: cutting one of the bones and placing it at the optimal angle to reduce the load on the joint.
Arthrodesis and osteotomy are used when it is impossible to perform endoprosthetics or it is necessary to postpone this operation for some time.
Make an appointment
Prevention
To keep your knees healthy, you must adhere to the following rules:
- lead an active lifestyle, engage in amateur sports, walk more and do exercises;
- avoid stress and overwork;
- minimize the risk of injury;
- maintain weight within normal limits;
- eat properly and balanced;
- wear high-quality orthopedic shoes;
- Avoid putting excessive stress on your knees (heavy lifting, professional sports, prolonged work on your feet).
The same rules are relevant for those who already suffer from arthrosis, because following them helps slow down the development of the disease.
Clinical recommendations for arthrosis
To get rid of pain and maintain normal condition of the musculoskeletal system, you need to:
- monitor your body weight – extra pounds significantly increase the risk of disease progression;
- get rid of heavy physical activity: heavy lifting, long walking, and especially long periods of standing;
- regularly perform physical therapy exercises;
- avoid injury; To do this, during training, gradually increase the load on the muscles, and also use special protective devices (knee pads, etc.);
- use special devices and techniques to restore impaired limb biomechanics (orthoses, taping);
- regularly visit your doctor and conduct courses of anti-relapse treatment.
Prognosis for arthrosis
With proper treatment of arthrosis and the patient following all the doctor’s recommendations, the progression of the disease and impairment of joint function can be stopped. It is also quite possible to completely relieve the patient of pain.
Prevention of arthrosis
To prevent arthrosis, you need to move more, avoid heavy physical activity and stick to a low-calorie diet so as not to gain weight.
Diet
The condition of cartilage largely depends on the quality of nutrition. If there are signs of arthrosis, it is recommended to exclude:
- carbonated drinks;
- alcohol;
- excessively fatty and spicy foods;
- canned food and semi-finished products;
- products with artificial colors, preservatives, flavors.
The diet should contain a sufficient amount of protein, fatty acids (especially omega-3), collagen (found in gelatin, agar-agar). It is necessary to structure the menu in such a way as to prevent weight gain.
Consequences and complications
Osteoarthritis of the knee joints develops very slowly, but if left untreated, this disease becomes the cause of serious and unpleasant complications:
- severe deformation of the joint and leg in general (associated with changes in the configuration of the knee, as well as restructuring of the muscle frame and curvature of the bones);
- shortening of the limb by grinding down the heads of the bones;
- ankylosis: complete lack of movement in the affected knee;
- damage to other parts of the musculoskeletal system due to improper load distribution (heel spur, arthrosis of the hip joint, pain in the spine).
To prevent these problems, it is important to undergo a timely examination by an orthopedist and follow his recommendations. Self-medication and addiction to folk remedies can cause a serious aggravation of the situation.
Localizations and clinical forms
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Arthrosis develops mainly in the most loaded joints – the knee and hip. But after an injury or against the background of arthritis, degradation-dystrophic processes can progress in any joint.
Classification of osteoarthritis
There are several classifications. The most famous are:
- Classification by etiology (reasons for development):
- primary – the causes of development have not been established;
- secondary – develop against the background of injuries and diseases.
- Classification by clinical forms:
- polyosteoarthrosis – multiple joint damage; divided into nodular (Heberden's and Bouchard's nodes) and nodular;
- oligoosteoarthrosis – the number of affected joints is no more than two;
- monoosteoarthrosis – damage to one joint;
- in combination with osteochondrosis or osteoarthritis of the spine.
- Classification by localization:
- interphalangeal;
- hip;
- knee;
- other.
Arthrosis of the lower extremities
Due to the high load, the legs suffer first of all:
- Arthrosis of the hip joint (coxarthrosis) is the most severe. The structural features of the hip joint (deep joint cavity, narrow joint space) contribute to the rapid development of degenerative disorders involving muscles and ligaments. If inflammation occurs, the effect of partial or complete immobility develops. Often develops against the background of congenital dysplasia, dislocations, subluxations of the hip, osteochondropathy (aseptic necrosis of the femoral head - Perthes disease). Symptoms of arthrosis: pain initially appears only towards the end of the day, but gradually increases, worries all day, radiates to the groin and buttock area. To reduce pain during coxarthrosis, the patient holds the leg in a forced position, which makes it seem shorter than the healthy one. The pain syndrome is very strong, so patients often agree to endoprosthetics.
- Arthrosis of the knee joint (gonarthrosis) - the most common. The knee withstands the highest loads and is injured, so gonarthrosis develops most often. Arthrosis of two joints is distinguished:
- patellofemoral - develops after injuries to the patellofemoral joint and is initially characterized by an inconspicuous course, since the joint has a lot of shock absorber cartilage that does not allow injury to the bone for a long time; but pain gradually appears after physical exertion, long walking or standing, when going up or down stairs; Over time, they become constant, dull, aching, and intensify when the weather changes; inflammation of the synovial membrane (synovitis) often develops, causing the pain to become acute;
- tibiofemoral arthrosis (femoral-tibial joint) - develops less frequently and is easier. The pain radiates down to the area of the lower leg and foot; Complete immobility with gonarthrosis rarely occurs. Prevention and timely treatment of arthrosis of the knee joint are very important - this will allow a person to live without pain. But even with an advanced disease, it is quite possible to relieve the patient from pain.
- Ankle – a large load also falls on the ankle, which is why arthrosis often develops in it. He is also often injured and the degenerative process is post-traumatic in nature. It is also affected in reactive arthritis. Symptoms: the disease is asymptomatic for a long time, but then pain appears. First, during physical activity, and then constant, aching pain. Stiffness of movement after a long rest is also characteristic, which goes away within half an hour. Complete immobility of the ankle is rare and only if the underlying cause of the disease is a long-term inflammatory process.
- Heel - arthrosis can develop in the area of the subtalar or talocalcaneal-navicular joints after injuries and diseases. They do not manifest themselves for a long time, then painful sensations in the heel begin to appear, gradually acquiring a constant painful character. Disability is rare.
Arthrosis of the upper extremities
Arthrosis in the joints of the hands develops less frequently. Main features of localizations in individual joints:
- Arthrosis of the shoulder joint. It usually develops after injuries and against the background of microtrauma in weightlifters, as well as in people engaged in heavy physical work. Acromial (acromio-clavicular) arthrosis is a consequence of trauma and inflammatory processes. At first it goes unnoticed, but then pain appears in the upper part of the shoulder, radiating to the elbow and neck, stiffness of movements and crunching when moving. The pain can be permanent and debilitating. Sometimes accompanied by inflammation, which contributes to the progression of the disease. If left untreated, partial ankylosis develops. Read more about shoulder arthrosis here.
- Elbow arthrosis - occurs rarely, mainly in miners, blacksmiths and workers of some other professions who deal with vibrating tools. Symptoms: pain in the elbow when bending and straightening the arm, stiffness after a long rest. If left untreated, there will be persistent dysfunction.
- Arthrosis of the joints of the hand. Most often, the degenerative process develops in the carpometacarpal joint of the first finger, since it is usually subject to trauma during household work. It manifests itself as a periodically appearing dull soreness in the outer side of the palm, radiating to the thumb.
- Arthrosis of the finger joints. Develops when performing small tasks (knitting, embroidery, sewing). In the distal (uppermost) interphalangeal joints, the pathological process manifests itself in the form of growths of bone tissue - Heberden's nodes; joint pain usually does not occur or they appear only occasionally, for example, when the weather changes. In the proximal interphalangeal joints, the disease manifests itself in the form of the same bone growths on the joints of the fingers located below - Bouchard's nodes.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Arthrosis of the spine (vertebral)
In different parts of the spinal column, arthrosis manifests itself in the form of different symptoms:
- Cervical uncovertebral arthrosis (cervical facet spondyloarthrosis) . Degenerative-dystrophic changes in small facet joints of the cervical vertebrae. Arthrosis of the joints of the cervical spine develops mainly in the second half of life in people who work for a long time in a stationary state with their heads bowed. It can also develop after injuries and against the background of chronic arthritis. It manifests itself in the form of headaches, dizziness, pain in the neck, radiating to the shoulder and crunching when moving. Decreased vision, hearing, and the appearance of high blood pressure (BP) are also possible. Since overgrown bone tissue can compress the vessels supplying the brain, the disease sometimes threatens the patient’s life. Requires long-term rehabilitation treatment.
- Thoracic spondyloarthrosis (arthrosis of the joints of the thoracic spine). It is much less common than the cervical one. First, moderate and then quite severe pain in the spine appears, intensifying with coughing, sneezing and deep breathing. Sometimes the symptoms are similar to manifestations of diseases of the cardiovascular and respiratory systems. To correctly establish the diagnosis, additional examination is required. In the thoracic region there are also costovertebral joints, 2 of them on each rib (rib head and costotransverse). They can also develop degenerative-dystrophic processes, mainly in older women. The disease manifests itself as pain in the chest. If it lasts for a long time, it can cause severe complications from the cardiovascular and respiratory systems.
- Lumbar spondyloarthrosis. It is a consequence of heavy physical labor and spinal injuries. Arthrosis of the joints of the lumbar spine manifests itself in the form of aching pain, aggravated by bending the body. Characterized by stiffness of movement after a long rest, a crunch in the back when bending over.
- Sacrococcygeal spondyloarthrosis. Most often develops after injuries, for example, after a fall and injury to the tailbone. It manifests itself as pain, aggravated by sitting and prolonged walking. Requires long-term rehabilitation treatment.
Tissue changes in spondyloarthrosis
Arthrosis of the temporomandibular joint (TMJ)
The disease develops with chronic arthritis of the TMJ, malocclusion, absence of lateral teeth, and problems with prosthetics. There is a violation of blood circulation and metabolism in the TMJ area with the development of degenerative-dystrophic processes in it. Symptoms of arthrosis of this joint: aching pain in the lower jaw, stiffness and crunching when opening the mouth and chewing. The pain increases with changes in weather, as well as with the development of synovitis. The long course of the disease leads to the appearance of asymmetry: displacement of the jaw tissue to the affected side.
Read more about the disease here.
Treatment at the Energy of Health clinic
If your knee begins to crackle or ache suspiciously after physical activity, you should immediately make an appointment with an orthopedist. The Health Energy Clinic offers its patients the most popular and effective methods for treating the early stages of arthrosis:
- modern drug regimens for cartilage restoration and pain reduction;
- intra-articular administration of drugs for rapid pain relief;
- physiotherapeutic techniques;
- physical therapy under the supervision of an experienced instructor;
- professional massage;
- PRP therapy;
- injection of artificial synovial fluid to facilitate movement.
All methods of treatment and prevention are selected individually depending on the results of the examination.
Advantages of the clinic
The Energy of Health clinic has modern equipment for diagnosing and treating a wide variety of diseases. We offer each client:
- comprehensive screening programs to identify various diseases;
- effective methods of laboratory and instrumental diagnostics;
- modern approaches to the treatment of diseases, including not only medications, but also physiotherapy, exercise therapy, massage and diet according to indications;
- consultations of highly qualified specialists;
- flawless performance of medical procedures;
- comfortable conditions and maximum comfort within the walls of the clinic;
- reasonable prices for all services.
Health is the greatest value. We will help restore and strengthen it. Take the first step towards excellent health, sign up for an examination at Health Energy!