Gonarthrosis is one of the serious degenerative-dystrophic diseases of the knee joint. In terms of frequency of occurrence among all possible arthrosis in the musculoskeletal system, it occupies the first position. The common disease is characterized by the destruction of articular cartilage, as a result of which the bone joint of the knee is deformed and loses its mobility functions. Since this department accounts for a significant share of the load, the pathogenesis that arose in its structures is actively progressing. The patient’s quality of life suffers significantly, and often the destructive focus leads to disability.
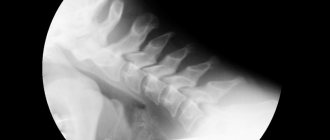
This is what the disease looks like on an x-ray. The arrows indicate the zone of destruction of cartilage tissue.
As you know, any disease has its own reasons, which provide fertile ground for its development. And gonarthrosis processes, as a rule, also do not develop out of the blue; they are almost always preceded by certain factors. However, this category does not include a very rare type of pathology - idiopathic gonarthrosis. What provoking factor “triggers” it still remains a mystery to science. Our article will be devoted to common causes, symptomatic signs and many other important aspects relating to gonarthrosis in general.
Signs and causes of the disease
Have you noticed any uncharacteristic sounds such as clicking, creaking or crunching in your knee when performing movements? Or maybe the leg in this section suddenly, after a simple walk or immediately after sleep, began to bother you with painful signs and/or stiffness? And after some time, did they go away on their own: in the first case - after rest, in the second - after 30-60 minutes, when the limbs had warmed up? But we ask all this for a reason, since these are the symptoms with a high degree of probability that can indicate gonarthrosis, at best stages 1-2.
The most important symptom of problems with the musculoskeletal system is pain. As long as it doesn't hurt, no one worries.
Important! If you do not pay attention to the problem in time, the pathological focus will reach an irreversible phase (stage 3-4), and conservative therapy will no longer be needed, you will have to undergo surgery. Often surgery is required already at stage 2, mainly for pathologies of rheumatoid origin.
So, if you have given an affirmative answer to at least one question, do not delay your visit to an orthopedic doctor and immediately undergo all the necessary examinations. After a thorough diagnosis, you will be individually prescribed the most effective treatment appropriate to the diagnosis. To make a diagnosis, it is usually sufficient to take an x-ray and test the biomechanical abilities of the knee area. Assessment of motor potential is carried out by performing certain movements of the limb with the help of a specialist and by the patient himself.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Diagnostics
If symptoms similar to manifestations of gonarthrosis occur, you should consult an orthopedic traumatologist. The doctor will interview the patient, find out his working conditions and lifestyle, clarify whether there have been knee injuries, etc. After this, the doctor will certainly perform an examination and evaluate the biomechanical abilities of the knee joint, asking the patient to make certain movements or independently conducting a series of tests. To finally confirm the diagnosis and clarify the stage of development of gonarthrosis, an X-ray or CT scan of the knee joint is prescribed.
But in the early stages of gonarthrosis development, X-ray examination does not provide a full range of data on the existing changes. In such situations, it is most advisable to perform arthroscopy, since this method allows one to accurately identify degenerative-dystrophic changes in the knee joint.
Arthroscopy is an invasive diagnostic procedure that involves the introduction of special endoscopic equipment into the joint through a microincision.
An MRI of the knee joint may also be prescribed. It is this method that allows us to detect changes in cartilaginous and soft tissue anatomical structures with 85% accuracy. Ultrasound does not have such capabilities.
Main symptoms
Let's return to the clinical symptoms. The older the disease, the more pronounced they will be. So, the disease manifests itself:
- crunching in the joint and other sounds (creaking, clicking, etc.) at the moment of making a certain movement (sounds are not typical for the last stage);
- painful syndrome of varying nature and color on the front and/or back side of the knee when moving;
- pain at rest , which indicates the neglect of the medical problem;
- muscle weakness, stiffness of the affected area, inability to move the joint correctly, limited range of motion;
- paresthesia in the form of numbness, tingling , etc. sensory disturbances;
- an increase in the size of the joint, which in severe pathogenesis can be seen visually; the affected knee is larger than the healthy one;
- periodic jamming (blockade) of the knee joint with a simultaneous feeling of sharp pain, which is explained by the entry of a necrotic fragment of cartilage into the space between the articular surfaces;
- instability of the leg (loss of support), and therefore the patient experiences frequent dislocations and subluxations.
An interesting feature: while there is no pain, we do not pay attention to the steps. But when the pain comes, we realize that we overcome a huge number of steps every day.
The initial signs of gonarthrosis primarily include morning stiffness and mild pain, which disappear immediately after the person moves normally. Additionally, at an early stage, weakness in the legs and clicking in the knee may be observed.
Pain symptoms and movement disorders are not always alarming at the onset of the disease or are mild in nature, which often prevents a person from paying attention to the problem in time and coming to the hospital. As practice shows, often the case already has to deal with 2nd degree of severity and higher.
Content
- Definition of disease
- Development mechanisms
- Causes and risk factors
- Symptoms of the disease
- Signs of disease progression
- Types and forms of the disease
- Stages of the disease
- Expert opinion
- Diagnostic methods
- Which doctor should I contact?
- Conservative (non-surgical) methods
- Drug therapy
- Orthobiology methods
- Physiotherapy
- Prevention
- Surgical tactics
- Bibliography
- Our methods
- Prices for services
- Why do they contact us?
- Patient reviews
- Make an appointment
- Popular questions for doctors
Factors provoking pathology
If a person’s general health status is good, he leads a healthy lifestyle, usually his joints function well and are not bothered day after day with or without painful sensations, even in old age. Otherwise, degenerative changes may arise that will begin to aggressively destroy important articular components that provide motor, support and shock-absorbing functions of the lower extremities at any age.
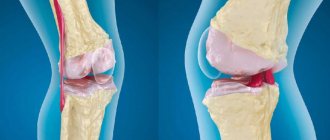
This is a real photo of the surface of the knee joint with gonarthrosis. Pay attention to damage that should not be there, the cartilage should be smooth as glass.
It is the progressive destructive processes in the knee joint that are commonly called gonarthrosis in medicine. It leads to the death of hyaline cartilage, which covers all surfaces of the articular bones, and as it becomes thinner and fibered, it leads to exposure and deformation of the latter and, as a consequence, to an extreme decrease in the quality of life.
An astroscope view of the destroyed cartilaginous surface in the joint cavity.
Arthrosis pathogenesis is often secondary, that is, when it becomes a consequence of certain pathologies, injuries, increased physical activity, etc. Anatomical and functional changes, as we have found out, mainly develop and become more complicated due to various negative factors. Among them, the most common ones are:
- congenital anomalies of the joints of the limbs (shortening of one of the legs, dysplasia, O-shaped and X-shaped deformities of the lower leg, etc.);
- post-traumatic consequences (complications of bruises, fractures, dislocations, sprains, etc.);
- joint hypermobility (JHM);
- rheumatoid arthritis, systemic lupus erythematosus, gout and pseudogout;
- local chronic infections and inflammations;
- obesity and metabolic diseases;
- endocrine diseases, especially diabetes and hypothyroidism;
- hormonal imbalances during menopause;
- excessive physical activity on the lower limbs;
- lack of physical activity, physical inactivity;
- constant overload of the legs associated with professional activities (sports, weight lifting, etc.);
- sitting for long periods of time in incorrect positions, for example, with your legs tucked under you;
- vascular pathologies of the extremities, hypothermia.
By the way, age-related physiological changes in bones, cartilage, and muscles occur in everyone as the body ages. These components wear out over time, becoming weaker, less flexible and elastic. This is not a paradox, but a natural phenomenon provided by nature, which begins approximately from the period when a person crossed the forty-year mark. Normally, it develops at a very slow pace, so nothing globally terrible happens to the joints. But there is one “but”. If the wear and tear of biological tissues significantly dominates the processes of metabolism and cellular nutrition, which is observed with the above factors, the joint begins to be progressively damaged.
It is enough to provoke the disease even by starting abruptly, without preparation, to engage in physical exercise, which you have never done before. Often, in pursuit of health, older people decide to radically change their lifestyle, for example, start running in the morning. Unprepared knee joints, which, as we noted, have some deviations due to age, are easily injured, and micro-tears appear in their structures and nearby areas. Such traumatization at the micro level, especially in people of retirement age, entails the development of gonarthrosis, not to mention more serious injuries.
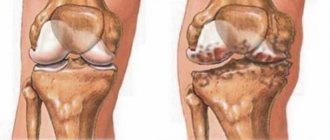
The knee and hip joints are most often affected. The picture shows the dynamics of destruction from left to right, from the complete absence of the disease to the last stage.
The disease can develop not only in the older generation (after 40 years or more), but also in young people 25-40 years old. Periods of mature and old age certainly provide more chances for complex pathology, because the natural elements of the joint are no longer as strong as they were before. In addition, women have a greater predisposition to pathomorphological phenomena in the joint, which is mainly explained by the hormonal characteristics of the female body.
Pathogenesis
The pathology develops over a fairly long period of time. The whole process can be defined in the following sequence:
- The emergence of causes of disruption of natural metabolic processes provokes the destruction of cartilage tissue.
- Destructive processes destroy the structure of the fibers responsible for the shock-absorbing effect. Not only the elasticity of the tissues gradually decreases, but also the stability of the joint.
- Due to the constant increased load on the joint membrane, an inflammatory process occurs, causing a decrease in mobility.
Principles of treatment
At the moment when the articular surfaces have not yet undergone fatal changes, but only minor degenerations, conservative treatment is applied. It is based on the following principles:
- physical therapy exercises without absolute vertical load - the doctor will prescribe the correct (!) set of trainings, which will improve metabolic processes in the joint and make it possible to stop pathological progression;
- losing weight through diet - losing weight is very important for overweight and obese people, because extra pounds put pressure on the joint, making it difficult to function normally;
- exclusion of physical activity , in which the bone joint functions in an enhanced impact mode (running, team sports, jumping, etc.);
- the use of non-steroidal anti-inflammatory drugs to relieve pain and swelling (Ibuprofen, Diclofenac, Voltaren, Indomethacin, etc.);
- the use of drugs to stimulate the production of synovial fluid and replenish osteochondral components with useful substances (chondroprotectors, hyaluronic acid);
- wearing special orthotic devices, orthopedic shoes;
- prescription of physiotherapeutic procedures (cryotherapy, ozokerite and paraffin applications, UHF, ultrasound, phonophoresis, etc.).
There are no statistics confirming that overweight people have more joint problems. But common sense has not been canceled, there is a big difference when you have 65 kg on your knees. or 110...
If the disease is characterized by a severe course or the conservative approach does not give positive dynamics, there is a need for surgery. Today, orthopedic surgeons carry out unique interventions (stage 2-4), in which the diseased knee joint or a separate part of it is replaced with an endoprosthesis, a biocompatible artificial analogue of a biological joint. We invite you to familiarize yourself with our videos and photos, which perfectly demonstrate the features of the procedure and its benefits.
Attention! It is impossible to cure this disease conservatively. Serious destruction cannot be corrected either by popular intra-articular injections or even by stem cell transplantation. Therefore, do not hope that newfangled minimally invasive and non-invasive techniques will magically help restore damaged hyaline cartilage, which, due to physiological characteristics, is not capable of regeneration. Alternative and official conservative medicine can only slow down unfavorable pathogenesis, and even then mainly only in the early phase of its development.
Endoprosthetics is the only orthopedic method that can relieve the patient from hellish pain and disability caused by gonarthrosis. There is currently no alternative to it! Replacement of the knee joint with a durable implant is carried out in the surgical department of orthopedics at a specialized clinic. Let us draw your attention: in order to achieve the most complete recovery after knee replacement, you should definitely undergo a special course of a rehabilitation treatment program.
With correctly performed implantation surgery and impeccable rehabilitation (it lasts on average 3-4 months), a person returns to a full life. Of course, he will need to follow simple rules so that the new knee joint can function without problems for at least 15 years. What is most remarkable is that 15 years is not the limit. Modern endoprosthetic knee designs, as shown by clinical observations of patients who have undergone this operation, in most cases last 20-25 years.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Prevention
Prevention of gonarthrosis of the knee joint comes down to the following measures:
- Elimination/minimization of severe physical overload of the knee joint (sports, household, professional).
- Avoidance of knee joint injuries/permanent microtrauma.
- Body weight control and dietary nutrition in cases of exceeding the physiological norm.
- Physical stress on the joints that is adequate to the age/condition of the body.
- Wearing special shoes/low heels, to unload the joint - walking with a cane.
- Regular wearing (as prescribed by a doctor) of knee braces/orthoses.
ICD code
According to the international classification of diseases (ICD-10), a disease such as gonarthrosis is assigned a code from M17.0 to M17.9. What kind of regulatory framework is this and why is it needed? The ICD is one of the most important documents on a global scale, developed by the World Health Organization to address global aspects in the field of medicine. The document, which includes 3 volumes, contains all known diagnoses, each of which is listed under a specific ICD code.
Emblem of the World Health Organization.
The code consists of one letter (disease class) and three numbers (the first 2 numbers are a specific disease from the specified class, and after the dot there is another number indicating its specific type and characteristics of the disease). This ordered classifier, which includes more than 12 thousand ailments, is used by medical specialists from all countries, which allows them to focus on uniform standards when making a diagnosis, use officially introduced standards for providing medical care to a patient, maintain medical morbidity statistics, etc.
In general terms, we have figured out the code, but for some it may still be unclear why the number 10 comes after the abbreviation ICD. Let us explain that this value denotes the 10th revision of diseases, that is, the document is currently using the tenth version (1990) with the day of its first release (1983).
Now let’s decipher the ICD code directly related to our disease:
- the Latin letter “M” stands for diseases of the musculoskeletal system and connective tissue;
- number “17” – gonarthrosis, or arthrosis of the knee joint;
- the number following “17” is indicated from the numerical range 0-9, it means a secondary or primary type of pathology, bilateral or unilateral localization, post-traumatic nature of origin or not.
Typically, patients have a secondary type of disease (usually post-traumatic) with a unilateral lesion (the focus is concentrated on one knee). For such a diagnosis, the code will be M17.3. And, for example, for post-traumatic gonarthrosis with bilateral localization (2 knees), the disease is recorded as M17.2. Primary arthrosis of the knee joint is M17.0 and M17.1. Let’s just say that there is no need to study ICD codes, unless the doctor “encoded” the diagnosis in the medical record in this way, and you really want to get to the bottom of the truth and find out the interpretation of the mysterious designations.
The medical classification of diseases was primarily created for medical and healthcare workers for diagnostic and therapeutic purposes, maintaining statistical records and using codes in official documentation (in disability certificates, benefit certificates, etc.).
Medicines for deforming arthrosis of the knee
Drug treatment of deforming arthrosis of the knee joint allows you to quickly relieve acute pain, reduce inflammation and swelling, and improve nutrition of the joint. Therefore, medications are used at all stages of the disease and help restore mobility to the knee.
Chondroprotectors
Chondroprotectors in the form of tablets, capsules, sachets and injections are used for the regeneration and maintenance of synovial cartilage.
The most effective chondroprotectors include artracam, dona, teraflex, structum, movex, artron, alflutop.
Anti-inflammatory
Steroid and non-steroidal anti-inflammatory drugs are used to treat deforming arthrosis of the knee joint. They are prescribed in the form of tablets, injections, sachets, creams, ointments and other products for external and internal use.
Nonsteroidal drugs (NSAIDs) include: artradoldiclofenac, nimesulide, paracetamol, meloxicam, indomethacin, ketorolac, ibuprofen, piroxicam and others.
Steroids: hydrocortisone, prednisolone, dexamethasone, kenalog, flosterone, methylprednisolone.
Anti-inflammatory drugs can be used in conjunction with anesthetics (novocaine, lidocaine, trimecaine), which are injected into the joint cavity as a blockade.
Antispasmodics
Relieving spasm is necessary for the patient to return to normal activity and the normal flow of nutrients into the tissues. For this purpose, buscopan, pentalgin, papaverine, drotaverine (no-shpa), spasmalgon, halidor, novigan and others are used.
Angioprotectors
For deforming arthrosis of the knee joint, troxevasin and troxerutin, pentoxifylline, drugs based on horse chestnut, detralex, trental, cinnarizine and others are used.
Warming agents
Among the warming agents, it is worth highlighting preparations based on natural ingredients: snake and bee venom, hot pepper, mustard. For example, capsicam, viprosal, apizartron.
Voltaren, Dolobene, Fastum, Finalgon and Nicoflex are also used. All these drugs improve blood supply to tissues and distract from pain.
Stages of bilateral damage
As we have already found out, pathological resorption of tissues of the knee joint can occur either exclusively in one lower limb or simultaneously in both legs. Simultaneous damage to the right and left joints is usually called bilateral deforming arthrosis. It is not difficult to understand that when both joints are affected by the disease, the pathology is more complicated and more difficult to tolerate, and it threatens the loss of locomotor-support functions of two limbs at once
Both knee joints are destroyed almost symmetrically.
Such pathogenesis sometimes belongs to the idiopathic or primary form of gonarthrosis. In other words, the disease appeared for no apparent reason, which does not happen very often. Often it has a post-traumatic nature of origin. This suggests that the degenerative-dystrophic process is caused by previously suffered knee injuries, which at one time were treated incorrectly, incompletely or not treated at all. No less often, it is facilitated by congenital pathologies of the musculoskeletal system (curvature of skeletal components, genetic defects of muscle-ligamentous elements, congenital inferiority of the joint, etc.). Another common consequence of disorders are certain diseases, especially rheumatoid arthritis and diabetes.
Good to know! Knee arthrosis requires competent differential diagnosis. To prescribe therapeutic measures that will help improve the quality of life, it is necessary to correctly diagnose and accurately determine the root cause of the pathology. And this is strictly within the competence of the orthopedist-traumatologist. It is impossible to find out on your own whether the problem really lies in gonarthrosis. In addition, there are a lot of movement disorders, for example, Parkinson's disease, which can easily be mistaken for arthrosis. Thus, you can make a mistake and trigger a very dangerous neurodegenerative brain disease. Therefore, if you have not done so already, undergo a high-quality diagnosis, and never prescribe treatment on your own!
Stages of gonarthrosis of the knee joint, from complete absence to complete destruction.
Like left- or right-sided osteoarthritis, bilateral disease occurs in several stages, and the clinical picture is not always equally expressed on the right and left limbs. Simply put, one of the joints suffers from irreversible changes to a greater extent than the other. Let's look at what happens to a large and complex joint at each stage, and how it affects a person. Note that the characteristics presented below are universal, therefore they are also applicable for left- and right-sided types, and not just bilateral arthrosis. The article will highlight the European classification of stages according to Kelgren.
Initial stage (1st stage)
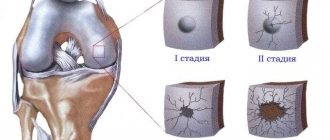
The painful syndrome is not very pronounced or absent. I may experience mild signs of impaired mobility, mostly in the morning and after prolonged physical activity. At the edges of the articular surfaces, X-rays reveal small osteophytes (bone growths), in the peripheral part of the articular bones - cysts of insignificant size and mild osteosclerosis. The gap between the articular surfaces has a slight narrowing or is not changed. At this stage, conservative methods promise a favorable prognosis for preventing the progression of the disease.
Second degree
At the second stage, the radiographic signs listed above become more distinct, namely: rough marginal spines and cystic formations are well visualized, osteosclerosis is sharply expressed, the radiograph clearly shows that the gap between the bone units has been significantly reduced, and the congruence of the joint is distorted. Painful sensations in the 2nd phase can no longer be confused with simple fatigue; they occur much more often and are more intense. A person notices a tendency for their appearance: pain is associated in particular with walking, going up and down stairs, and forced long-term standing. The flexion function is most impaired, the person begins to limp. To help the patient, specialists already at this stage often resort to surgical intervention methods, since non-surgical tactics sometimes refuse to “work”, and the disease progresses.
Third stage
The pain becomes persistent and almost constant, lameness progresses, and the muscles are seriously atrophied. The patient is no longer able to cope without the use of supporting devices. The third degree of severity provokes curvature of the legs, more often varus deformity, when the limbs acquire an O-shape, as they say simply, “legs like a wheel.” At the same time, the interarticular space is critically narrowed, there are practically no “living” zones of cartilage, and osteophytes are of massive size. The exposed articular surfaces of the bones are in contact with each other, each movement is accompanied by strong friction. Often non-viable tissues and pathological bone formations break off and fall into the joint cavity, which causes terrible pain and joint blockages. At this stage, knee replacement surgery is inevitably needed. Otherwise - lifelong disability with excruciating physical suffering.
Fourth stage
This is the end point, which is characterized by the final loss of the joint - the complete death of all its functional structures. That is, the hyaline cartilage is erased, there is no joint space, and the bony epiphyses are terribly deformed. This stage can be characterized in two words - hellish pain, which even powerful painkillers cannot extinguish. Regarding the motor potential of the problematic limb, we can say the following: there is a persistent flexion-extension contracture, the maximum possible loss of support, coordination and the ability to move. The patient is mostly confined to a wheelchair; at best, he moves with the help of a walker or crutches.
4th degree of gonarthrosis is the last one on the right. A pronounced deformation of the joint and the axis of the tibia is noticeable.
I would like to note that advanced pathology also negatively affects the spinal system and the musculoskeletal framework as a whole. Therefore, it is not surprising when a patient complains that, in addition to unbearable pain in his legs, he has pain in his lower back or another part of the spine. At the final stage of degenerative processes, since the pronounced pain syndrome “does not go away” either day or night, total bilateral endoprosthetics is indicated as an emergency.
The diagnosis is based on an assessment of the patient’s complaints, his individual data (professional activity, concomitant and past diseases, level of daily physical activity, etc.), as well as on the information that the orthopedic doctor receives during examination, after instrumental and laboratory diagnostics.
Diet
Diet for gonarthrosis of the knee joint
- Efficacy: healing effect
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
One of the most important factors slowing down the development of degenerative-dystrophic processes in the cartilaginous tissue of the joints is therapeutic nutrition, which, in combination with drug treatment, physiotherapy, exercise therapy, orthopedic regimen, therapeutic massage and spa treatment, can improve the patient’s quality of life. The diet for gonarthrosis is aimed primarily at correcting metabolic processes, regulating body weight/fighting obesity , preventing pathological changes in the hyaline cartilage of the knee joints, stopping the inflammatory process and normalizing articular connective tissue structures. Medical nutrition is based on the following principles:
- Physiological completeness and balance of the diet with a high content of minerals/vitamins. For patients with normal body weight, the energy value of the diet should not exceed the average daily energy expenditure.
- Any fish/meat broths containing extractives, refractory fats, fatty meats, smoked meats (ham/bacon), semi-finished meat/fish products or canned food containing various kinds of food additives in the form of preservatives, flavor enhancers and dyes should be excluded from the diet. , salo.
- Limit to 5-8 g/day salt and salty foods.
- Introduction of 1-2 fasting days/week in the form of a curd fasting day (350-400 g of cottage cheese and 500 grams of milk for 3-4 doses); fruit and vegetable fasting day (1.5 kg of fruits/vegetables with rosehip decoction); kefir fasting day (1.5-2 liters of kefir).
The basis of nutrition for gonarthrosis should be a diet enriched with vitamins/microelements - low-fat varieties of sea/river fish, seafood, dietary meat, low-fat cottage cheese, offal, chicken eggs, butter, cereals, vegetables/fruits, unsalted cheese, whole grain varieties bread, nuts, low-fat dairy products, virgin vegetable oils.
To maintain the cartilage tissue of the joints, it is necessary to include in the diet foods containing mucopolysaccharides, which are by their nature natural chondroprotectors (red fish, cartilage, chicken/pork legs, chicken meat, hard cheeses, gelatin) from which it is recommended to prepare jellied fish, jellies, fruit jellies/jelly. These products, when taken frequently/long-term, normalize the structure of cartilage tissue, help accelerate the processes of its synthesis, slow down degenerative processes and normalize joint function.
In case of obesity/body weight exceeding the norm, the calorie content of the diet should be reduced within 500-600 kcal and not exceed an average of 1800-2000 kcal/day, which allows for a gradual reduction in body weight. First of all, simple carbohydrates up to 250-300 g and refractory animal fats up to 60 g are subject to restrictions, and the protein content must correspond to the physiological norm.
Limit the consumption of white bread, pastries, sugar, confectionery, sweets, cream-containing products, honey, chocolate, fast food, fatty meats, mayonnaise, high-fat dairy products (cream/sour cream), duck/goose meat, smoked meats, animals/ cooking fats. It is prohibited to consume salty foods (canned food, pickles, preserves), starchy foods, cocoa, strong black tea, coffee, seasonings/spices that increase appetite - ketchup, vinegar, garlic, ground black pepper, horseradish, mustard, onions. All fried foods are also excluded. Meals are fractional. Sweet carbonated/alcohol-containing drinks are subject to restrictions.
Consequences of not treating the disease
The consequences of the disease can be the most tragic. And we are talking here not just about those standard violations (destruction and deformation of the knee) that arise at each stage. With them, we think, everything is clear: if competent therapy is not started in a timely manner, a disappointing outcome is predetermined - the patient’s disability, which can occur quite quickly. But we would like to say a few words about the potential danger of the disease for other segments of the musculoskeletal system, in particular for the spinal column and other joints.
As we said above, the trouble with problems with joints is that if the work of one department is disrupted, then other areas, primarily the spine, are immediately involved in destructive processes.
Gonarthrosis, in 75% of cases it affects the medial (inner) part of the knee, is also a real aggressor for your spine - one of the most important and significant segments in the body. The disease creates additional stress on the vertebral elements, since it does not allow normal movement without adaptive postures. Thus, with advanced forms, the following serious problems may most likely be added to it:
- radiculitis;
- curvature of the vertebral axis;
- intervertebral canal stenosis;
- intervertebral hernia;
- osteochondrosis;
- vertebral instability.
Moreover, the listed ailments can provoke negative consequences in the future. And it is likely that, along with knee replacement, you will also be prescribed (before or after the main operation) another surgical intervention, but on the spine. We are sure that everyone has understood the essence of the problem. By the way, the same applies to other joints, most often the limbs. Due to the incapacity of the knee, they act as compensators for its functions, taking on too high loads, which is fraught with their rapid wear and, as a consequence, the same arthrosis in the near future.
Fortunately, synovitis can be successfully treated, unlike gonarthrosis.
It is impossible not to mention at the same time that sometimes synovitis appears against the background of gonarthrosis - an inflammatory process that affects the synovial membrane of the knee joint. As a result of synovitis, large volumes of joint fluid (synovium) accumulate in the articular cavity, which stagnates and literally puts pressure on the joint, pushing it out from all sides, which is why the knee area swells noticeably, local hyperemia and hyperthermia of the skin may appear, rise general body temperature. In addition, excess fluid can leak into the popliteal region, resulting in a popliteal hernia (Baker's cyst).
Thus, the main pathology plus its complications in the form of these diseases in combination will extremely aggravate the already unsatisfactory clinical picture. We have given only a few examples of consequences from a large list. We won’t scare you with other complications; you yourself must understand the seriousness of your problem and treat it with all the responsibility. In the end, what is at stake is your physical viability, which is the most valuable thing in life.
Study as much information as possible and visit only competent specialists.
Remember, restoring the biomechanics of the legs is not an easy process, often requiring high-tech surgery and then 3-4 months of rehabilitation. Therefore, seek medical help from professional specialists in a timely manner; only they will be able to diagnose any forms of the underlying pathology and associated complications, and then develop the most effective algorithm for treatment measures.
Forecast
In gonarthrosis, the prognosis is determined by the stage of the pathological process and the adequacy/timeliness of the therapy. With grade 1 gonarthrosis, if you follow the doctor’s recommendations, the pathological process can be slowed down and the prognosis is generally favorable. While with pronounced destructive changes, conservative treatment is ineffective and the third stage of gonarthrosis is the cause of loss of ability to work/disability. Such patients are indicated for surgical treatment, including knee replacement.
Gonarthrosis and the army
Many young male patients wonder: are they drafted into the army with such a complex pathology? To clarify, we suggest you read the information that we have specially prepared for you. So, first of all, your military suitability will be assessed:
- severity of clinical symptoms of the disease;
- degree of deformation;
- the presence of concomitant pathologies (systemic pathologies, congenital anomalies of the musculoskeletal system, flat feet, kyphosis and scoliosis of the spine, etc.).
Suitability to become a recruit is determined by a military medical commission on an individual basis based on x-rays of the joint, personal medical history and laboratory test results. It is impossible to say unequivocally whether you will be released from service or not without seeing your examination results. However, you can use information from regulatory documents, which contain diagnoses and their criteria for which exemption or deferment from military service is allowed. Arthrosis of the knee is regulated by Art. 65, which lists possible options that allow exemption from the army:
- Stage 2 , in which there are osteophytes larger than 1 mm, the joint space is narrowed 2 or more times from normal values, there is impaired joint congruence and subchondral osteosclerosis. The young man most likely will not serve, even though he is marked “fit” in the relevant document.
- 3-4 degrees allow you to fully count on exemption from military service. This diagnosis is accompanied by severe pain, while X-rays clearly show large spiky growths, significant osteochondral deformations, and a complete or almost complete absence of joint space. In fact, a disabled person, it’s hard to even say where one can work with such a sentence, let alone the army. Therefore, category “D” is assigned with the note “unfit”.
Regarding stage 1 of the disease, we note that it does not provide grounds for exemption from the army; the conscript is only given privileges to mitigate the conditions of service.
Classification
Based on the ways the disease appears, there are:
- primary gonarthrosis - occurs on its own, often in the nature of bilateral gonarthrosis;
- secondary gonarthrosis of the knee - develops against the background of injuries or other pathologies of the knee joint, there are two types: right-sided gonarthrosis on the right leg and left-sided gonarthrosis on the left leg.
The severity of symptoms depends on the degree of gonarthrosis:
- Stage 1 – dull pain, slight swelling of the joint, no deformation;
- Stage 2 – increased symptoms and pain, the presence of a crunch, moderate limitation of movement and mild deformity;
- Stage 3 – maximum clinical symptoms, gait disturbance and severe constant pain, limited mobility and visible deformation of the joint.
What is the difference between gonarthrosis and arthrosis?
It might be worth starting the article with an interpretation of these medical terms. But if you read it carefully, you probably guessed that there is no fundamental difference in the concepts of these two names, except in pronunciation and spelling. Gonarthrosis is also no different from osteoarthritis of the knee joint. The essence, features of the initial manifestation and later periods of development, prevention and therapeutic measures of all these pathologies are equivalent. All of them indicate the same direction of degenerative-dystrophic pathogenesis, however, with only one difference: the diagnosis “gonarthrosis” cannot be used in relation to other bone joints. Why?
Gonarthrosis, which means degeneration and dystrophy of the articular cartilage of the knee joint (translation from the Greek knee + arthrosis), provides information about the specific localization of deforming arthrosis (osteoarthrosis), namely in the knee. But, for example, the term “coxarthrosis,” which you also repeatedly came across when reading medical Internet sources, also means deforming arthrosis, but of the hip joint (hip + arthrosis). Arthrosis and osteoarthritis are general concepts that are simultaneously suitable for any joint.
Anatomy of the knee joint
The knee joint consists of two surfaces, which are formed by the tibia and femur. The front of the knee joint is protected by the patella, which moves between the condyles of the femur. The fibula does not participate in the formation of the knee joint and essentially does not bear any functional load, due to which it is often used for the reconstruction of other bone elements in the body.
All articular surfaces: the tibia, femur and the inner surface of the patella are lined with hyaline cartilage, which is very smooth in texture, has a high degree of strength and elasticity, the thickness of this dense and elastic structure reaches 5-6 mm. Cartilage absorbs shock during physical activity, prevents friction and softens impacts.