Liver failure is a complex of complex symptoms that is characterized by a violation of the vital functions of the liver, caused by acute or chronic damage to the organ tissue.
Any abnormal liver function requires immediate medical intervention. There are acute and chronic liver failure. Chronic liver failure develops over several months or years, but acute liver failure can develop within a few hours.
What functions does the liver perform?
The content of the article
The liver is a large organ located in the abdominal cavity. This important organ performs various functions and takes a significant part in regulating the homeostasis of the body.
The most important functions of the liver:
- metabolic function – processing of carbohydrates, proteins, fats;
- storage – including iron and vitamins;
- detoxification - the liver is involved in the removal of harmful substances in food, as well as medications;
- production of bile, which is especially important when digesting fats;
- immune function – some liver cells play an important role in immune reactions.
What are the causes of liver failure?
There are acute and chronic liver failure.
Chronic liver failure is most often caused by cirrhosis and infection with hepatitis viruses (hepatitis B and C), which ultimately also leads to cirrhosis.
Cirrhosis
Cirrhosis is a disease in which fibrous reconstruction of the liver occurs, as a result of which its function is impaired. The most common cause of liver cirrhosis is alcohol abuse. Other, rarer causes include:
- autoimmune hepatitis;
- primary biliary cirrhosis;
- metabolic diseases;
- chronic use of certain medications.
Infection with hepatotropic viruses is a chronic infection. The liver is usually affected by viruses type B and C. In addition to cirrhosis, chronic hepatitis may predispose to the formation of hepatocellular carcinoma.
Acute liver failure is a sudden and rapid deterioration of liver function that after a few weeks leads to encephalopathy, bleeding disorders and, if untreated, death.
Causes of acute liver failure:
- acute viral hepatitis, mainly types A and B;
- some medications - most often paracetamol, halothane, sulfonamides, statins;
- poisoning;
- severe systemic diseases - shock, sepsis, portal vein thrombosis, etc.
3. Treatment of the disease
If liver failure caused by acetaminophen overdose is diagnosed early enough, the disease can sometimes be cured completely and all negative effects eliminated. Similarly in the case of a virus, if liver failure occurs due to a virus, supportive care in a hospital will help avoid serious consequences until the virus passes. In these cases, the liver can recover on its own.
For liver failure, when severe liver damage has already occurred, the first goal of treatment may be to preserve the part of the liver that is still able to function. If this is not possible, then a liver transplant is not required. But even in cases where a liver transplant is necessary, this operation is usually successful.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms of liver failure
Symptoms of liver cirrhosis develop slowly and are not noticed by the patient for a long time. At first, patients usually complain of weakness, itchy skin and jaundice. As the disease progresses, muscle atrophy and ascites appear - the patient's abdominal circumference increases, with rather thin limbs.
Other symptoms of liver cirrhosis:
- low-grade fever;
- lack of appetite, weight loss;
- vascular bundles on the skin;
- palmar erythema (redness);
- excessive hair growth in women;
- dilated venous vessels of the abdominal wall (“head of the jellyfish”);
- symptoms of hemorrhagic diathesis due to a deficiency of coagulation factors;
- ascites and pleural fluid - caused by albumin deficiency and leakage of fluid from blood vessels.
Low-grade fever
Lack of appetite
Sexual dysfunction also appears. As a result of disturbances in the metabolism of sex hormones, men experience symptoms of feminization - hair loss on the chest and armpits and gynecomastia, as well as hypogonadism - loss of libido. Women are diagnosed with menstrual irregularities.
2. Symptoms of the disease
The initial symptoms of liver failure are often similar to those of other diseases, including the most common ones. Because of this, liver failure can be difficult to diagnose early in the disease. The first signs of liver failure may be:
- Nausea;
- Loss of appetite;
- Fatigue;
- Diarrhea.
As liver failure progresses, symptoms become more severe and require immediate medical attention:
- Jaundice;
- Minor bleeding;
- Constipation;
- Mental disorientation and confusion (hepatic encephalopathy);
- Drowsiness;
- Coma.
Visit our Hepatology page
Complications of liver failure and cirrhosis
Cirrhosis leads to a serious complication – portal hypertension. This is an increase in blood pressure in the portal vein system, which, when transferred to subsequent vessels, causes collateral circulation in the form of, among other things, esophageal varices. This is a serious complication that can lead to massive gastrointestinal bleeding. This may be the first sign of cirrhosis.
Other complications of liver cirrhosis:
- Ascites is the accumulation of fluid in the abdominal cavity caused by a deficiency of albumin in the blood plasma;
- Spontaneous bacterial peritonitis caused by the penetration of bacteria from the intestinal lumen into the peritoneum. Pathogens cause infection of ascites fluid. In this case, the symptoms are rarely typical for peritonitis; fever, abdominal pain, and encephalopathy are usually observed;
- Hepatorenal syndrome, that is, deterioration of renal function in liver cirrhosis. The occurrence of this syndrome is an indicator of poor prognosis, as renal function may rapidly deteriorate, leading to end-stage renal disease with the need for dialysis in the short term;
- Hypersplenism is excessive splenic function that causes pancytopenia in some patients;
- Acute liver failure. This is a sudden and rapid impairment of liver function, which mainly manifests itself in the rapid development of encephalopathy and the appearance of plasma coagulation disorders.
- Hepatic encephalopathy is a collection of neurological and psychological symptoms resulting from impaired elimination of toxins from the body. They enter the central nervous system, causing disturbances in consciousness, dementia, behavioral disorders and brain damage.
Symptoms of acute liver failure are plasma ecchymotic coagulation disorders, bleeding, and in rare cases, overt bleeding, usually from the gastrointestinal tract.
Prognosis for acute liver failure
Acute liver failure before the use of modern therapy and liver transplantation led to death in 80% of patients. Currently, this figure has been reduced to 40%. The cause of the disease and the presence of complications are the main factors determining the prognosis.
Patients with acetaminophen-induced liver failure have a better prognosis than those in whom the cause of the disease is unknown. The presence of cerebral edema, renal failure, coagulopathy, or infectious complications worsens the prognosis. Severe hepatic encephalopathy grade 3-4 is also associated with a greater risk of death.
Diagnosis of liver failure
When diagnosing liver failure, the patient's medical history is key. The facts of alcohol abuse and the presence of situations that increase the risk of hepatotropic viral infection are mainly important. Signs of organ failure are identified, for example, the degree of blood clotting disorder is assessed.
During a physical examination, the gastroenterologist notes an enlargement of the liver - the organ is relatively noticeable when palpating the abdominal wall.
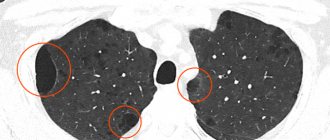
A useful tool in diagnosing liver failure is abdominal ultrasound. The examination helps to accurately assess the size of the liver, its structure, as well as the width of the portal vein (important in the case of portal hypertension) and possible complications, for example, the presence of fluid in the abdominal cavity.
Abdominal ultrasound
Additional tests are laboratory tests, mainly the determination of transaminases and bilirubin, which allow indirect assessment of liver function. These tests should be performed periodically, and the frequency of tests depends on the rate at which symptoms worsen.
Types of pathology
The pathogenesis of liver failure implies the following classification of the disease:
- Hepatocellular form. Involves damage to organ cells by toxins and other poisons. According to statistics, in most cases, toxic substances damage liver cells due to alcohol abuse. If healthy cells die slowly, organ damage develops gradually; if quickly, it develops rapidly.
- Portocaval form. Liver damage occurs due to disturbances in hepatic blood flow. When there are a large number of toxins and other poisons in the circulatory system, the blood does not pass through the liver, but goes directly into the general bloodstream. In this case, the liver cells suffer from a lack of oxygen.
- Mixed form. It is a combination of symptoms of cellular and portocaval forms. Toxic substances affect both liver cells and the bloodstream, so failure develops rapidly. The mixed form is considered the most dangerous.
According to the course of the disease, two types of deficiency are distinguished:
- Spicy. A condition that, if persisted for a long time, is dangerous to human life. Due to acute intoxication, rapid damage to the organ occurs. The duration of development of this type of disease ranges from several hours to several months.
- Chronic. Signs of the disease appear gradually - from several months to several years. Typically, this form of liver failure develops against the background of exacerbation of other chronic liver diseases.
Sometimes renal-liver failure occurs - a serious condition that has a fulminant (rapid) development, has an acute form, and often leads to death.
There are also several degrees of deficiency: initial, moderate, severe. In each case, the intensity of symptom progression is individual, so the duration of each stage is different.
Treatment of liver failure
Treatment of liver failure should be symptomatic. However, cirrhosis detected at an early stage of development can be reversible if the pathogen or cause can be destroyed.
The gastroenterologist selects drugs that support liver function, containing, among other things, phospholipids. Phospholipids are components of the cell membrane of hepatocytes; they stabilize and support membrane regeneration, inhibit collagen synthesis, slowing down the breakdown of the organ.
A proper diet supports the treatment of liver failure. The gastroenterologist prescribes an easily digestible diet with limited fatty foods. The following should be excluded from the diet:
- fried food;
- hot spices;
- animal fats – lard, fatty fish;
- foods that cause bloating - beans, peas;
- alcohol is an absolutely important condition.
In the case of viral hepatitis, treatment directed by a gastroenterologist should be carried out by an infectious disease specialist.
For acute deficiency, symptomatic treatment should be used to reduce cerebral edema, prevent encephalopathy, and support the coagulation system. At the same time, the only effective treatment for liver failure that completely eliminates the problem is a liver transplant.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Sources
- Acute Liver Failure. Mescape. Updated: Jun 13 2021 — https://emedicine.medscape.com/article/177354-overview
- Pediatric Liver Transplantation. Medscape. Updated: March 17 2019 —https://emedicine.medscape.com/article/1012910-overview
- Liver Transplants. Medscape. Updated: December 31, 2021 — https://emedicine.medscape.com/article/776313-overview
- Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Pubmed - https://www.ncbi.nlm.nih.gov/pubmed/19524577
- Fulminant Hepatitis. Family Practice —https://www.fpnotebook.com/GI/Lvr/FlmntHpts.htm#fpnContent-panel-id_2
- Acute Liver Failure in Children. Medscape - https://www.medscape.com/viewarticle/584466_1
- The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. PubMed —https://www.ncbi.nlm.nih.gov/pubmed/16879891
- Cirrhosis. Medscape. Updated: 30 July 2017 —https://emedicine.medscape.com/article/185856-overview
- MELD Score for End-Stage Liver Disease (NOT appropriate for patients under the age of 12). Medscape —https://reference.medscape.com/calculator/meld-score-end-stage-liver-disease
- Acute liver failure. PostgradMed —https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1743234/pdf/v081p00148.pdf
- Modern prognostic models of survival of patients with terminal stage diseases. Journal of Clinical and Experimental Surgery - https://www.cesurg.ru/ru/jarticlescesurg/60.html?SSr=40013379b601ffffffff27c_07df070a01282f-690 12.Overview of the Indications and Contraindications for Liver Transplantation. PMC _ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996378/
- Liver transplantation for acute hepatic failure. PMC—https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2131363/
- Indications and Contraindications for Liver Transplantation. International Journal of Gepatology - https://www.hindawi.com/journals/ijh/2011/121862/
- Liver transplantation for chronic liver disease: advances and controversies in an era of organ shortages. Postgraduate Medical Journal - https://pmj.bmj.com/content/78/917/135
- Extracorporeal liver support. Organogenesis —https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3082035/
- Lifestyle Changes to Manage Cirrhosis. Winchester Hospital —https://www.winchesterhospital.org/health-library/article?id=19276
- What Are the Treatments for Cirrhosis?. WebMd —https://www.webmd.com/digestive-disorders/tc/cirrhosis-home-treatment#2
- Cirrhosis and Chronic Liver Failure: Part II. Complications and Treatment. American Family Physician - https://www.aafp.org/afp/2006/0901/p767.html https://www.aafp.org/afp/2006/0901/p767.html
- The use of extracorporeal methods for the treatment of liver failure. Kutepov Dmitry Evgenievich - https://cyberleninka.ru/article/n/ispolzovanie-ekstrakorporalnyh-metodov-lecheniya-pechyonochnoy-nedostatochnosti