Environmental deterioration, unhealthy diet, and unhealthy lifestyle of parents are some of the most common reasons that negatively affect the condition of children’s visual organs. And if false strabismus in newborns goes away with age, then true strabismus needs early diagnosis and correction. How to recognize where the true strabismus is and where the false one is?
Parents of newborns are often concerned about the asymmetrical gaze of the baby, but receive “evidence” in the form of stories of friends with a successful outcome, whose children also had strabismus, but it went away on its own. Yes, sometimes this happens - as the baby grows, the structures of his eyes become stronger, and the squint disappears.
Typically, by five months of the first year of life, strabismus, associated with the infant's inability to control the eye muscles, disappears.
But it also happens differently: parents wait for everything to get better without the participation of doctors and lose precious time because the child develops true strabismus. Therefore, understanding the features of determining such a pathology in children as strabismus, it is worth understanding the importance of early diagnosis.
Strabismus in children - when should you worry?
If you go to see a specialist in a timely manner for a complete diagnosis, you won’t have to worry, because the clarity of the diagnosis makes the treatment process easier. Pediatricians usually notice strabismus during the first examinations of a newborn. Infants are often diagnosed with strabismus - due to weak muscles, it is difficult for the eyes to move in a coordinated manner, focusing correctly on an object.
Most often, newborns' eyes squint from time to time, and not constantly. If parents notice that the visual axes of one or even two of the child’s eyes are shifted to the bridge of the nose or are shifted not to it, but in the opposite direction - to the temples, and constantly, then it is necessary to go to the doctor for examination and advice.
Prevention of strabismus at an early age:
- routine examinations with an ophthalmologist;
- timely treatment of concomitant eye pathologies - for example, childhood farsightedness;
- control of visual load - it is necessary to ensure a good level of lighting in the playroom, offer the baby large toys;
- responsible attitude towards the hardware treatment prescribed by the ophthalmologist, attendance at all sessions of magnetic and laser stimulation.
If the physiological strabismus of infants goes away by six months, then the diagnosis of true strabismus in older children, with the right approach, adequate therapy and prevention, can be removed after two to three years of treatment.
Recommendations for parents
In order to prevent strabismus and visual impairment in children, it is necessary to control the time they watch TV shows and spend time at the computer. The child should have a properly equipped and well-lit place where he could draw, look at pictures and books.
You should not read while lying down, placing the book too close to your eyes or to the side. You should not buy glasses using the “selection” method without having your vision checked by a specialist. If you have any visual impairment, you should immediately consult a doctor.
What types of strabismus are there?
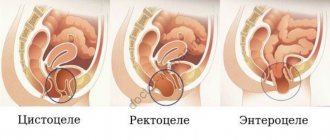
Normally, the axes of both eyes of a person should be parallel. If the baby has an asymmetrical gaze, we can talk about strabismus, which, in turn, is divided into types. It can be horizontal, vertical and combined.
Types of strabismus:
- horizontal strabismus - the eyes can converge towards the bridge of the nose or, conversely, diverge, gravitating towards the temporal zone;
- vertical strabismus - the eye muscle in this case cannot hold the eye and it deviates up or down;
- combined is a vertical-horizontal lesion of the oculomotor system;
- paralytic and concomitant - with a paralytic disease, paralysis of one or more motor muscles of the eye is noted, and with a concomitant disease, the eyeballs retain their mobility without paralysis or paresis - this is treated by wearing glasses and hardware therapy sessions.
Hyperfunction of the inferior oblique muscle of the eye is the main reason why upward deviations are observed in concomitant strabismus of the convergent type. Vertical deviation is difficult to treat and usually requires surgical intervention. With congenital strabismus, it is diagnosed in 90% of cases.
Among the causes of occurrence, the predominant ones are: previous infectious diseases, paresis of the ocular motor muscle, head injuries. With farsightedness, convergent strabismus is most often observed, and with myopia, divergent strabismus.
In addition to horizontal, vertical and combined strabismus, there are also monocular or alternating strabismus.
With alternating strabismus, both eyes squint periodically. With monocular - one eye. If the disease is not diagnosed and treated in a timely manner, amblyopia may develop - “lazy eye” syndrome, when information from the squinting eye is ignored by the brain.
When corrected with glasses, the healthy eye must be closed so that the amblyopic eye becomes fixative. To get him back into work, the strabismus is corrected with glasses; in some cases, surgery is recommended for the little patient.
Pleoptics
Like optics, the pleoptics method is one of the options for correcting childhood strabismus without surgery. The essence of the therapy is to completely cover the healthy eye with an overlay. This method is called occlusion. Having lost the ability to receive an image from a healthy organ of vision, the brain connects the eye with pathology to work.
Another option for the same therapy is the use of the drug atropine. The product is instilled into the healthy eye and temporarily relaxes its accommodation. This is the ability of the eye to see equally well at both close and far distances. Thus, the drug forces the eye to work abnormally. The bandage is not used in this case.
Strabismus in children: where is false and where is true?
A specialized specialist must diagnose the type of strabismus and choose a treatment method. He also prescribes therapeutic measures if necessary. It is impossible to independently determine whether strabismus is false or true, since the effect of asymmetry of a newborn’s eyes is enhanced by the anatomical features of the facial part of the skull, for example, the wide bridge of the nose.
During the examination, the doctor pays attention to the presence or absence of certain oculomotor disorders. If there are no oculomotor disorders, then we can talk about false strabismus, which will soon not be noticeable.
What should parents be wary of?
- If a child turns his head at an unusual angle in order to better see an object of interest to him.
- If the baby often bumps into objects located on the side of the squinting eye.
- Children older than one year may complain of headaches.
Tests help determine imaginary or true strabismus. There is a test in which the optometrist projects a light source onto the two eyes and compares the location of the corneal light reflex in each eye. In the absence of pathologies, the light reflection is symmetrical, but with strabismus it will be shifted from the center. This test does not detect small angle deviations.
Also, to diagnose visual pathologies in infants, a test with a bright toy is used, which should completely take over the baby’s visual attention. While the child is interested in looking at the toy, the doctor will conduct a test with alternate closing of the eyes. If there is an abnormality, the eye will make a rapid adjustment movement as soon as the other eye is closed. The test is performed with fixation on close and distant objects.
What is called strabismus?
This is a pathology in which there is an asymmetrical arrangement of the eye pupils in a person looking forward. Normally, both eyeballs should move in the same direction when examining an object. In this case, a three-dimensional “binocular” image is obtained, since the gaze of both eyes is focused simultaneously. With strabismus, when one eye looks directly at an object and the other at a certain angle, the brain perceives a distorted picture, which leads to a gradually worsening visual disorder.
Strabismus (strabismus) can be congenital or acquired in a child. Many children mow down before 6 months, and this is not a pathology. Even before 1 year of age, there is hope that the defect will disappear on its own as soon as the muscles responsible for the movement of the eyeballs become stronger.
Sometimes strabismus occurs in children aged 1-3 years, but it can occur later. This is no longer normal and indicates the presence of some kind of eye or neurological disease in the child.
Addition: It is interesting that with true strabismus, only one eye squints. There is such a thing as “imaginary strabismus”. It seems as if both eyes are looking in different directions. However, squint has nothing to do with it. The defect is purely cosmetic and is a hereditary feature of the location of the eyeballs in the sockets or a congenital abnormality that arose during the formation of organs in the embryo. The illusion of sideways eyes occurs during the development of facial bones in a newborn child, if his nose bridge is wide and the distance between the eyes is reduced.
Causes of true strabismus in children
What are the causes of true strabismus? The disease can be congenital or acquired. It happens that a child is born with a vision pathology, but often strabismus develops against the background of neurological diseases, as well as due to farsightedness or anisometropia (the difference in refraction between the left and right eyes).
As soon as a child begins to assemble mosaics and play with construction sets, the visual load increases, and at this time the growth and formation of the optical structures of the eye continues, and binocular vision is formed.
If, in addition to playing with construction sets and small parts, the baby is fond of playing games on a smartphone or tablet, then the load on his eyes increases many times over, which contributes to the development of various pathologies, including strabismus.
Any stress can be a provoking factor for the development of true strabismus in children: fear, trauma, infectious diseases that occur with a multi-day fever. If treatment for strabismus is not started in a timely manner, it can develop into a serious functional pathology. Unfortunately, people with untreated strabismus perceive the world as flat and cannot perceive volume.
Surgical intervention
Surgery to correct strabismus in children is performed only when conservative treatment has failed. In modern ophthalmology, this type of surgical intervention is considered uncomplicated. The operation is performed under local anesthesia and lasts about 30-45 minutes.
The prerequisites for the operation are:
- large angle of strabismus;
- paralysis of the eye muscles;
- damage to the extraocular muscles;
- disruption of innervation.
During the operation, overstressed muscles are loosened and weak ones are strengthened through surgery. This method helps to achieve balance for the correct location of the eyeball in relation to the central axis. In some cases, not one, but several operations are required.
It should be noted that this operation is not associated with the return of visual acuity. Its goal is to restore the synchrony of eyeball movements. Next, you will have to correct your vision with glasses, visual gymnastics and hardware treatment. Gymnastics for the eyes
To remove overstrain and relieve eye fatigue, experts have developed simple exercises. Two adults need to do eye exercises with children. One of them should hold the child's head so that he performs the exercises only with his eyes.
For the youngest patients, visual gymnastics will resemble a game. You should take the toy and move it sideways at a certain distance: up and down and left and right. Movements must also be made in a circle, diagonally and in a spiral. Schoolchildren can do eye exercises on their own. Exercises involve focusing on an object located at a far and close distance. You need to take turns looking at the thing that lies nearby and the one that is further away. There are many types of concentration exercises. The attending physician will certainly recommend several suitable ones. They should be performed daily at a slow pace before bed. Each must be done 3-5 times.
How to treat strabismus
This is not a cosmetic defect, it is a serious disorder, and strabismus must be treated. Over time, a squinting eye may stop participating in visual work due to the fact that the brain does not perceive the information coming from it. To prevent this from happening, a number of therapeutic measures are taken: correction with glasses is prescribed, and the load on the squinting eye is increased. Treatment methods for strabismus:
- pleoptic treatment - it is recommended to undergo up to three to four courses per year of hardware therapy, which stimulates the work of the squinting eye, loading it (computer programs, therapeutic laser are used);
- physiotherapy, daily exercises, including special exercises for the eyes, strengthening the accommodative muscle;
- glasses for the correction of visual impairments - wearing glasses you can perform interesting tasks to find a way out of the maze, solve puzzles, assemble whole pictures from parts;
- surgical intervention.
Treatment of strabismus depends on the causes that contributed to the appearance of the disease, and since it affects the work of all parts of the visual apparatus, the treatment must be comprehensive. If it turns out to be effective and the strabismus has become less noticeable, therapy should be continued until the age of 20-23, even if visible visual defects disappear.
In cases where hardware treatment does not help, experts recommend surgery.
Surgical treatment of childhood strabismus
Parents often ask the question of whether it is possible to decide once to take on the operational risk (which, as everyone understands, is inherent to one degree or another in any surgical intervention) rather than undergoing tedious and lengthy training treatment. The motives for such questions are understandable, but the situation should be clarified immediately.
Surgical correction of strabismus is prescribed in cases where pleoptic and orthoptic treatment are obviously futile or do not bring tangible results for at least one year. In case of strabismus with a large angle, the operation becomes the first, or rather, “zero”, preliminary stage of treatment, after which the same exercises and training will still be needed. Surgically, by strengthening or, conversely, weakening elements of the ocular muscular system, it is possible to achieve only an anatomically correct, coordinated position of the eyes, but this will not affect other visual functions: the body must “learn” to see with both eyes. It should also be borne in mind that sometimes the operation itself to eliminate strabismus is carried out in several stages.
Surgical correction of paralytic strabismus is often due to the need to eliminate its direct cause: tumor, infectious focus, traumatic changes, etc. To correct refractive error, glasses are prescribed, followed by pleoptic and orthoptic therapy. During treatment, proven and effective physiotherapeutic procedures (acupuncture, muscle electrical stimulation, etc.) and various drug regimens are widely practiced.
When is it necessary to treat strabismus and perform surgery?
In case of true strabismus, if it was not possible to achieve a lasting therapeutic effect using hardware techniques, simulators, correction with glasses and exercises, it is necessary to undergo surgery. Experts recommend it for children with strabismus up to four to six years of age. Thanks to new mathematical modeling techniques, operations have become less traumatic, and rehabilitation periods have been reduced. After the procedure is completed, the little patient will be able to go home the next day.
What happens during the operation? Depending on the causes of strabismus, the surgeon will operate in such a way as to strengthen the weak muscle that supports the eyeball. Or relax her if she fixes her eye in the wrong position. Today, doctors use laser techniques to correct strabismus. These methods are bloodless and gentle: operations are performed under local anesthesia, and recovery takes about a month.
Treatment of childhood strabismus
First of all, it must be emphasized again: the effectiveness of treatment directly depends on the stage at which it begins. Therefore, at the first signs of strabismus, you should immediately contact an ophthalmologist. Obviously, only a doctor can identify the causes, diagnose the type and degree of strabismus, and prescribe adequate treatment in each specific case. As a rule, correction of strabismus is a rather lengthy process and takes 2-3 years. It is important to understand this and be patient, without demanding immediate healing from the doctor using, for example, one miracle pill.
Conservative treatment of concomitant strabismus is carried out in several stages, at each of which a specific therapeutic task is set and solved, depending on the specifics of the existing problem.
So, if strabismus is combined with a refractive error, corrective glasses are prescribed, and today models have been developed and successfully used even for the youngest patients (from six months of age), made entirely of unbreakable plastic materials.
These glasses are prescribed for constant wear, and the sooner the better. Even if there are no visible changes in the angles of strabismus at first, you cannot refuse glasses; During regular monitoring by an ophthalmologist, they may need to be periodically replaced.
However, glasses alone are not enough to treat strabismus.
At the first stage, pleoptic therapy is used, which can be started only after 3-4 weeks of wearing glasses. Pleoptic treatment aims to “train” the eye muscles and thus is intended to prevent the development of amblyopia. The goal is to align vision in both eyes as much as possible and ensure their simultaneous, coordinated functioning.
Pleoptic treatment includes such basic methods as penalization, local irritation of the retina with light, direct occlusion, various exercise systems (for example, the method of negative sequential images). As additional methods, general illumination of the retina, various computerized techniques, exercises with dosed light and visual loads, and reflexology are prescribed. However, the basic and initial treatment method at the first stage is either penalization or direct occlusion.
The essence of both methods is to “force” the eye that sees worse to work. Penalization is used at the age of 1 to 4 years to treat convergent strabismus, if only one eye is squinting and visual acuity is below 0.4. A prerequisite is also the absence of myopia (normal or farsighted vision). Two modifications are used: for distance vision and for near vision. Penalization consists of a temporary artificial deterioration of vision in the better-seeing eye. This is achieved by instilling atropine into it according to the regimen prescribed by the doctor; Glasses with excess glass on the problem eye are also prescribed (i.e., with more powerful correction than is actually required). In this case, the healthier eye is excluded from near vision, and the problematic eye is “forced” to take over all these functions. This course lasts from 4 months to six months. If tangible results can be achieved, a similar scheme is used for distance vision. For young children, when it is impossible to accurately measure visual acuity, penalization of distance vision is used only if the gaze of the affected eye is focused on nearby objects. Sometimes atropine is not prescribed, but in these cases glasses must be worn constantly. In one of the variants of the technique, an excessively strong glass is installed on the side of the healthier eye, and the necessary correction is provided for the problematic one. This method “trains” the distance vision of the healthy eye and includes the eye with the abnormality in its work.
The occlusion method is used if there is no effect from penalization (in general, not earlier than 4 years of age). Direct occlusion , or “overlap” translated from Latin, consists of completely blocking the healthier eye - it is simply covered with glasses with one opaque glass - in order to “make” the diseased eye work. Wearing such glasses is prescribed according to various schemes: for the whole day, for several hours every day, only under conditions of increased load, etc. The period of wearing glasses with occluder glass varies from one month to a year or more; A follow-up examination by an ophthalmologist is required 1-2 times a month, since there is a possibility of decreased vision in the “resting” healthy eye. In the latter case, alternate occlusion is prescribed (either the “best” or the “worst” eye is closed for periods of several days). With at least an approximate leveling of visual acuity in both eyes, or with the transformation of constant strabismus into alternating strabismus, the achieved success is consolidated by alternating occlusion for about 3 months. Then wearing glasses with an occluder is gradually reduced until completely abolished.
The criterion for the effectiveness and duration of application of the occlusion method are the results of a control examination after the first two months of wearing glasses: if there is no positive dynamics, further wearing them loses all meaning. It should be noted that it is more difficult for the smallest patients to adapt to new conditions, so it is better to introduce them into the permanent occlusion mode gradually, starting with 20-30 minutes a day and increasing the time spent daily in glasses.
The technique of local “blinding” retinal exposure is used provided that the problem eye focuses correctly on objects. To illuminate a limited area of the retina, various types of pulsed light sources, including lasers, are used.
The negative sequential image method is a modification of the previous procedure: the central region of the retina is blocked from light by a three-millimeter ball, resulting in the creation of a specific field of vision that has therapeutic properties. This method can be prescribed even if it is difficult or incorrect to focus the gaze on target objects.
When visual acuity decreases from 0.2, a special tabletop device amblyotrener , designed for the development of visual orientation as part of the treatment of amblyopia, is effective. Exercises with a maculotester - this device was originally intended for diagnostics, but can also be used in training mode.
From two to three years of age, treatment with the method of general illumination of the retina ; When treating older children, specialized computer programs are widely used.
The next, so-called orthoptic stage of treatment begins when it is possible to achieve visual acuity of at least 0.4 in each eye. Necessary conditions are also full muscle balance and age from 4 years. The goal of orthoptic treatment is to restore and strengthen the natural ability of binocular perception, i.e. combining images obtained from two eyes separately into a single three-dimensional visual image. The main apparatus for training this ability is the synoptophore. This is one of the devices built on the principle of separately presenting images to each eye. Normally, these fragments are automatically merged by the brain into a complete image; with strabismus, this requires fine tuning to shift the right or left fragment (this shift is determined by the angle of the existing strabismus). After diagnosis, muscle balance training begins: the eyes gradually “get used” to seeing and turning in harmony.
The final stage in the correction of concomitant strabismus is diploptic treatment . This technique is aimed at restoring binocular, stereoscopic vision, and the body must gradually restore this ability itself through constant hard training. With the help of special interchangeable lenses (prismatic configuration), a bifurcation of the field of view is artificially caused; the eye and visual analyzer, forced to cope with optical aberration, try to recreate the original image. Diploptic treatment of this type is prescribed to children from the age of two and provided that the angle of strabismus does not exceed seven degrees.
An additional course after successful correction of strabismus is prescribed a special system of exercises to strengthen the eye muscles, coordination and ease of eye movements. Such a recommendation should also be taken seriously and responsibly, since training in the processes of accommodation, movements to the right and left, etc. is extremely important in terms of preventing the recurrent development of strabismus and visual impairment in the future (considering what time we live in and with what load on eyes of a modern “information” person).
Symptoms
The main sign of strabismus is the deviation of the pupil of the eye from the axis. But there are a number of other absolute signs of the disease:
- significant decrease or complete absence of movement of the affected eye;
- dizziness occurs if you close your eyes;
- the baby may complain of double vision;
- blurred vision and difficulty describing the image;
- involuntary tilt of the head when focusing your gaze;
- in a situation where the optic nerve is damaged, accommodation paralysis, pupil dilation or ptosis develops.
In children under 3 years of age, the main reason for a visit to an ophthalmologist may be regular squinting when focusing on an object.
What parents should know about their baby's vision
At birth, a child has only a number of visual reflexes: the reaction of the pupils to light, turning the eyes to a bright sudden source of light. The child cannot see well yet. He gradually acquires this skill only by the age of seven, and for the first months the baby learns to recognize objects, colors, contours and shapes. Two to three weeks after birth, color and object vision gradually develops, and after eight to ten weeks, tracking eye movements become smooth. In the fourth month, the ability to estimate distance appears. The child sees his hands, begins to coordinate movements between his eyes and hand, and his brain learns to compare, evaluate and draw conclusions from sensations from different senses. By the age of seven, the visual system should normally be completely formed, but the visual assessment of space improves at a later age. A completely healthy child may also have some discoordination in the work and movements of the eyes, but in order to eliminate the problem, one must not miss the obligatory visits to the ophthalmologist for all infants: every month, every six months and every year.
How to determine the disease
Ophthalmologists diagnose the disease quite simply by visually examining the child. The doctor will observe how the baby’s gaze fixates on the object and how his eyes react to bright light.
The diagnosis of the disease is made by an ophthalmologist after a thorough history taking, examination and clarification of the reasons that led to the development of the disease: how the pregnancy and childbirth went; when did strabismus appear? is it constant or periodic? squints one or both eyes; were there any infections or injuries; Do you have any relatives who suffer from visual impairments and what kind of impairments.
Without fail, the doctor checks visual acuity, determines the angle of strabismus, evaluates the joint functioning of the eyes, examines the mobility of the eyeballs in all directions, and examines the fundus. If paralytic strabismus is detected, a consultation with pediatric specialists in the field of neurology and psychiatry is prescribed.